Sandbox:Christina
Wikidoc
Nasal polyp
Diagnosis
History and symtoms
Nasal polyps don't cause any symptoms and could be an incidental finding if it's smaller in size. Larger polyps or clusters cause many symptoms of obstruction like lack of smell or taste, stuffy nose, facial pain or headache, sneezing, and runny nose, postnasal dripping, itchiness around the eyes, and snoring.
Physical examination
Laboratory findings
Electrocardiogram
XRAY
CT
MRI
Ultrasound
Other Diagnostic studies
Pathophysiology
PMID: 8521175 Even though it is considered an idiopathic condition, it has been considered that frequent infections and inflammations could cause polyps originating from the lining of ethmoidal or maxillary sinuses. Histopathological study on the polyp shows epithelial damage, edema, fibrosis, hyperplastic or metaplastic changes of epithelium, and basement thickening.PMID: 8922142 These nasal polyps are also abundant in eosinophils, mast cells, T lymphocytes, cytokines, chemokines, interleukins, TNF-α, and adhesion molecules. Multiple studies have been performed to establish how genetic factors correlate with the development and persistence of mucosal inflammation that causes nasal polyps. Several genes and single nucleotide RYD5 polymorphism has been studied to be found to be a potential cause.PMID: 26204469 It has been postulated that subjects with HLA-DQA1*0201-DQB1*0201 haplotype expression increase the risk of having nasal polyp by 5.53 times.PMID: 10718431 Weakened mucosal innate immunity and impaired immune response also contribute to the pathogenesis of the disease.PMID: 18416964 A zinc metalloenzyme, Carbonic Anhydrase(CA) functions by transporting water and electrolyte across the epithelium. Hence, a downregulated expression of CA plays a role in edema in nasal polyps, and studies on the genes and variants that cause this reduced expression can help in with diagnosis and management of the disease. PMID: 18622311
Fungal particles usually reside in the nasal mucosa of healthy individuals. However, the same fungal particles can act as antigens in immunocompromised individuals. This antigen response leads to increased eosinophils and inflammatory markers. Superinfections stem from translocating germinating spores in contrast to fungus balls which are irritant to the neighboring cells. Most common species involved in nasal polyposis is Aspergillus and Alternaria."""PMID: 16210651"""
Biofilm:
Etiology
Although the etiology of the disease is unclear, it is a common disease affecting 4% of the population. It is often associated with many pathogenic conditions like aspirin sensitivity(36%), asthma(7%), cystic fibrosis(20%) and especially chronic rhinosinusitis. Other conditions with nasal polyps are Churg-Strauss Syndrome(eosinophilic granulomatosis with polyangiitis), allergic fungal sinusitis, and cilia dyskinetic syndrome, (Kartagener's),Young Syndrome and Nasal mastocytosis. Nasal polyps are found more commonly in non allergic asthma than in allergic asthma.
Cystic fibrosis (CF) is the most common cause of nasal polyps in children. Therefore, any child under 12 to 20 years old with nasal polyps should be tested for CF. Half of the people with CF will experience extensive polyps leading to nasal obstruction and requiring aggressive management.-- management
Differential Diagnosis
Most of the nasal masses might look like a nasal polyp. Hence,some of the differential diagnosis among benign masses include encephalocele, glioma,antrochoanal polyp, angiofibroma and inverted papilloma . While malignant masses include squamous cell carcinoma (SCC), esthesioneuroblastoma, nasal lymphoma and rhabdomyosarcoma .
Epidemology
Nasal polyposis is a common disease in the population and has been estimated to as 1-4%. Nasal polyposis occurs more in men compared to women. The prevalence of nasal polyps increases substantially between 40 to 60 years of age. Since the exact etiology of nasal polyp is unclear, studies have postulated multiple theories including genetic associations and increased incidence among asthmatic patients. Patients with Chronic rhinosinusitis(10%-54%) especially allergic fungal rhinusinusitis aspirin sensitivity (40%-80%) and cystic fibrosis (36%) found to have nasal polyp. Hence, children with nasal polyps should get a mandatory cystic fibrosis workup to rule it out.
Risk Factors
| Risk factors for Nasal polyps |
|---|
|
Screening
Natural History,complications and prognosis
Classification
- Primary classification
- Ethmoidal Polyps: Mostly found in adults. These are small and grape-like masses, originating from ethmoidal sinuses and grows into the middle meatus.
- Antrochoanal Polyp: They are common in children and present as a large solitary polyp. They originate from the maxillary sinus but grow backward to the posterior choana and hang down behind the soft palate.
- Histopathological Classification of Nasal polyp PMID:8922142
- Eosinophilic edematous(allergic): It is the most common nasal polyp which is characterized by edema, goblet cell hyperplasia of the epithelium, basement membrane thickening. They are abundant with eosinophils and leukocytes too.
- Fibroinflammatory: These nasal polyps are a result of chronic inflammation and metaplasia.
- Polyp with Hyperplasia seromucinous glands: Rare
- Polyp with Atypical stroma: Rare
- Phenotypical classification of Chronic Rhinosinusitis with Nasal polyp :
- Eosinophilic
- Neutrophilic
- Non Eosinophilic Non-Neutrophilic
Otosclerosis
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: CSN, M.D.
Synonyms and keywords: Otospongiosis
Overview
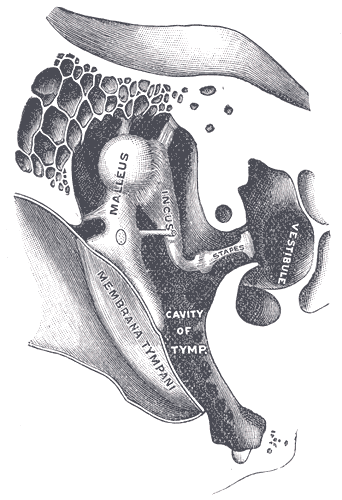
Otosclerosis is a word derived from the Greek word "sklērós" meaning hardening and oto meaning ear. Otosclerosis is an osseous dyscrasia of the otic capsule, which should be an endochondral dense bony part in the labyrinth, replaced by irregularly laid spongy bone leading to the fixation of stapes. It is one of the most common causes of conductive deafness with normal tympanic membranes. Thereby affecting sound transmission to the inner ear at the level of the oval window Though majority of cases are observed at the oval window, otosclerosis can also affect the round window, cochlear apex, posterior to the oval window, posterior and anterior wall of the internal auditory canal (IAC), cochlear aqueduct, semicircular canals, and within the stapes footplate. It can be asymptomatic or in advanced cases extend into the bony labyrinth and affect cochlea which causes mixed conductive and sensorineural hearing loss depending on the position of foci. Otosclerosis is common in Caucasians and predominantly women. Hormonal fluctuations in women like during pregnancy and menopause may aggravate the disease. Many genetic factors contribute to the development of otosclerosis. And it is an autosomal dominant inheritance with incomplete penetrance. Measles was found to be one of the reasons for otosclerosis. Other factors include inflammatory cytokine and cytotoxic mediators secondary to inflammation. (CT) scanning of the temporal bone can often demonstrate foci of demineralization in the otic capsule in cases of cochlear otosclerosis. The treatment for hearing loss is essentially stapes surgery with successful improvement of 90%-95% in the first 5 years; decreases to 63% after 30years and rarely need revision surgery. Additionally, hearing aid and cochlear implants could be used along with surgery.
Historical perspective
- 1704:Antonio Maria Valsalva identified fixation of stapes as a cause of hearing loss
- 1841:Toyn bee stated, "osseous ankylosis of the stapes to the fenestra ovalis as one of the causes of deafness".
- 1876:Johannes Kessel described stapes surgery as the treatment.
- 1930-1950: Used Julius Lempert’s single-stage fenestration of stapes as treatment.
- 1956:John Shea modernized stapedectomy.
Classification
- Based on Symons/fanning grading system
- Grade 1: Fenestral Otosclerosis
- Grade 2: Cochlear Otosclerosis
- Grade 2A:Basal cochlear turn Otosclerosis
- Grade 2B:Middle/Apical turn Otosclerosis
- Grade 2C:Both Basal and Middle/apical Otosclerosis
- Grade 3:Diffuse confluent cochlear involvement (with or without fenestral involvement)
Embryology
Table explains the embryological process for the development of bony labyrinth
| Gestational week | Developmental process |
|---|---|
| 4th week |
|
| 8th week |
|
| 16th week |
|
In certain cases, completion of the third stage of bone formation doesn't occur leading to cartilages between bony structures. During labyrinth bone formation, the anterior to the oval window is usually the last area to develop. This area is the most common site for otosclerosis.
Pathophysiology
Accumulation of bone deposits because of increased bone remodeling which is bone resorption followed by bone deposition in the otic capsule result in otosclerosis. Audiological findings are directly proportionate to the extent of bone remodeling. Bone remodeling happens in 3 phases:
| Phase | Mechanism of action |
|---|---|
| Otospongiosis | Increase in both osteoclast activity and microvascularity |
| Transitional phase | begins with deposits of spongy bone by osteoblasts in areas of previous bone reabsorption |
| Otosclerotic phase | characterized by spongy bone deposits developing into dense bone that narrows the microcirculation previously developed in the otospongiosis phase |
The lesions occur mostly in the anterior to the oval window by calcifying of annular ligament or by involving stapes footplate (80%). While 30% of cases have the lesion at the round window,21% have it at pericochlear region, and 19% at the anterior segment of the internal auditory canal.
Etiology
Though the exact cause of otosclerosis is unknown and multiple research studies are still ongoing, several etiologies are the following:
- Embryological Cause
- During the maturation of the otic capsule of the labyrinth, certain places skip the complete conversion to endochondral, leading to irregularly laid spongy bone. This most commonly is seen at fissula ante fenestram.
- Genetic Cause
- Studies have been conducted and found Type 1 collagen gene(COL1A1), a component essential for bone metabolism plays a role in otosclerosis. TGF-beta 1(BMP 2 and BMP 4 gene and Angiotensin II (AGT M235T and ACE I/D genes) are also found associated with otosclerosis. Other genetic causes for otosclerosis include sex hormones, autoimmune reaction, human leucocyte antigen, inflammatory and regulatory cytokines, parathyroid hormone, and expression of parathyroid hormone-related peptides receptors, and oxidative stress
- Gender
- Women are more likely to have otosclerosis than men , suggesting the role of sex hormones.
- Ethinicity
- Otosclerosis is more common in Caucasians and Japanese compared to African populations.
- Age
- Even though otosclerosis could be seen in patients at their twenties and thirties, it usually causes hearing loss only in or after their forties.
- Pregnancy
- There is no strong evidence why pregnancy worsens hearing loss in some patients with otosclerosis.However 33% women with otosclerosis are found to deteriote in hering after one pregnancy.
- Measles
- RNA of measles virus was detected at the footplate of stapes in otosclerotic patients , suggesting its role in casuing it, while incidence has reduced significantly in vaccinated populations.
Trauma and Major surgeries also cause otosclerosis.
- Autoimmune
- Though research on this is in the initial stages, inflammatory cytokine like TNF-alpha and cytotoxic mediators were found at the otosclerotic bone suggesting its role in the pathology.
Differentiating otosclerosis from other diseases
| Conditions mimicking Otosclerosis |
|---|
|
Epidemiology and demographics
- Though a variable pattern of inheritance is observed, 60% of patients report a family with a history of otosclerosis. Thus researchers conclude this condition as an autosomal dominant with incomplete penetrance.
- Greater preponderance in women compared to men in a ratio of 2:1.
- Even though the disease begins in the second and third decade of life, it doesn't result in hearing loss until the fourth decade.
- Clinical prevalence of otosclerosis is found to be higher in Caucasians by 0.04%-1% while the histological incidence of otosclerosis increases to 10% in the same..The incidence of histological otosclerosis is 1% and 5% in African and Asian population respectively.
Risk Factors
- Genetic factor
- Otosclerosis is an autosomal dominant disease with incomplete penetrance. When 60% of patients were found with family history, 40-50% of patients have it with variable patterns of inheritance. But hearing loss in otosclerosis is found only with family history of the same.[1]
- Hormonal conditions
- Puberty, pregnancy, and menopause increase the occurrence of hearing loss in pre-existing otosclerosis.
- Measles
- Persistent measles virus infection of stapes footplate results in activated osteoclast and inflammatory pathways by TNF-alpha mRNA. The protective function of osteoprotegerin at the otic capsule is inhibited by TNF-alpha and its action on RANK production
Screening
Even though otosclerosis appears to be genetic deafness, early prevention can help in combating the disorder and its prevention.
- Systematic Impedance-audiometry screening: The purpose of this screening is to detect a possible diphasic impedance change (on-off effect) by eliciting stapedius reflex. It is done in school going-children and helps in the early detection of stapedial fixation.
- Systematic Bone-conducted audiometry screening: It is done in young children with a family history of otosclerosis.
Natural History, complications and Prognosis
Prognosis
Most of the patients find improvement in their hearing ability after the surgery. Only a few don't have any change post-surgery and rarely hearing loss worsens. There have been cases where the prosthesis was found displaced from its original position, causing conductive hearing loss again in some patients. The second surgery was observed to be less successful than the first.
Complications
Post-op complications:
- Perilymph fistula (3-10%): Progressive hearing loss, tinnitus, or vertigo.
- Taste disturbance(9%)
- Facial nerve injury (< 1%)
- Sensorineural Hearing loss(< 1% chance)
- Poststapedectomy granulomas
- Vertigo: Usually mild, subsides over time.
Clinical presentaion
Patients present with the following:
- Most cases are asymptomatic and diagnosed as an incidental finding in temporal autopsies.
- Bilateral(80%) or unilateral involvement earlier in the disease.
- Progressive hearing loss, which might worsen with lower tone and frequencies like male voices and vowels.
- vertigo(10%)
- tinnitis (50%)
- Schwartz sign or flemingo's pink sign(not necessary for diagnosis): redness along the promontory of tymphanic membrane on otoscopic examination
Diagnosis
Physical Examintaion
Tuning fork
- Pros of using a tuning fork for diagnosis:
- Negative Rinne test
- Weber test lateralizes to the ear with severe conductive loss.
- Cons of using tuning fork for diagnosis
- Rinne test cannot differentiate between sensorineural hearing loss and normal hearing loss.
- Weber test's inability to differentiate a bilateral hearing loss.
Whisper test
Audiometry and tympanometry
- Caharts notch: Bone conduction depression in threshold at 2000Hz. After stapedectomy caharts notch diappears.
- Tympanometry normal at early disease. In severe cases, flattening and stiffening of curve representing low complaince of ossicular chain and tympanic membrane. Good test to differentiate between otosclerosis and pathologies with low resonance.
CT Imaging

- High resolution computed tomography (CT) of the temporal bones is the imaging technique of choice in the diagnosis of otosclerosis.
- However, preoperative CT has little to add in establishing otosclerosis diagnosis and may not even be necessary to confirm diagnosis.
- CT is recommended to be reserved for those patients with presumed additional abnormalities, for specific preoperative planning, or for legal necessity.
- CT Finding: increased bony radiolucency in the otic capsule around the anterior footplate, thickening of the stapes, and widening of the oval window.
- Early sign on CT: halo sign; demineralized area outlining the cochlea.
Treatment
- Medical Management
- Sodium flouride: Though controversial, it is used to slow the progression of otosclerosis.
- Bisphosphonates: By inducing osteoclastic apoptosis, bisphosphates cause antiresorptive action, with promising results.
- Hearing aid:It is used alone or in combination with other treatments.
- Surgical Management:Stapedotomy or Stapedectomy along with placement of a prosthesis, has shown a good prognosis with improved hearing ability. Only rare cases have shown no benefit. Revision surgery is controversial but proposed for patients with no improvement of hearing loss, facial nerve damage, or persistent vertigo.Most common cause of stapedectomy failure is prosthesis displacement with or without incus erosion. Revision surgery is also recommended post surgery for patients with footplate fixation, perilymph fistula, otosclerotic regrowth. Post surgery, some are still encouraged to use a hearing aid..
Prevention
Otosclerosis cannot be prevented but early detection of the disease can help in combatting the disease better.
References
- ↑ Rudic M, Keogh I, Wagner R, Wilkinson E, Kiros N, Ferrary E; et al. (2015). "The pathophysiology of otosclerosis: Review of current research". Hear Res. 330 (Pt A): 51–6. doi:10.1016/j.heares.2015.07.014. PMID 26276418.