ST elevation myocardial infarction initial care: Difference between revisions
No edit summary |
m (Bot: Removing from Primary care) |
||
| (4 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
{{ST elevation myocardial infarction}}{{CMG}}; | __NOTOC__ | ||
{{ST elevation myocardial infarction}} | |||
{{CMG}}; {{AE}}{{CZ}} | |||
==Overview== | ==Overview== | ||
The goal of initial care of the STEMI patient is to restore epicardial artery patency as rapidly and fully as possible, and to reduce the risk of early vessel [[reocclusion]]. Other goals include reducing the risk of lethal [[ventricular arrhythmias]] and other mechanical [[ST Elevation Myocardial Infarction Complications|complications]] as well as reducing myocardial oxygen demands to limit infarct size with [[ST elevation myocardial infarction beta blocker therapy|beta blockers]]. | The goal of initial care of the STEMI patient is to restore epicardial artery patency as rapidly and fully as possible, and to reduce the risk of early vessel [[reocclusion]]. Other goals include reducing the risk of lethal [[ventricular arrhythmias]] and other mechanical [[ST Elevation Myocardial Infarction Complications|complications]] as well as reducing myocardial oxygen demands to limit infarct size with [[ST elevation myocardial infarction beta blocker therapy|beta blockers]]. | ||
| Line 9: | Line 12: | ||
==Initial Care== | ==Initial Care== | ||
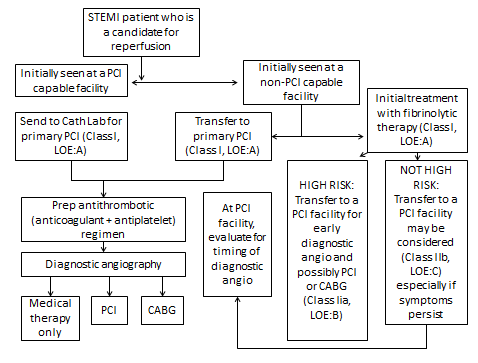
Triage and transfer for [[PCI]] in [[STEMI]]: | |||
[[Image:Triage_in_STEMI.png|center|450px]] | |||
You can read in greater detail about each of the therapies below in greater detail by clicking on the link for that therapy. | You can read in greater detail about each of the therapies below in greater detail by clicking on the link for that therapy. | ||
[[ST | [[ST elevation myocardial infarction oxygen therapy|Oxygen]] | [[ST elevation myocardial infarction nitrate therapy|Nitrates]] | [[ST elevation myocardial infarction analgesic therapy|Analgesics]] | [[ST elevation myocardial infarction aspirin therapy|Aspirin]] | [[ST elevation myocardial infarction beta blocker therapy|Beta Blockers]] | [[Coronary care unit|The coronary care unit]] | [[Step Down Unit|The step down unit]] | ||
==Sources== | ==Sources== | ||
| Line 20: | Line 27: | ||
{{reflist|2}} | {{reflist|2}} | ||
==External | ==External Links== | ||
* [http://www.themdtv.org The MD TV: Comments on Hot Topics, State of the Art Presentations in Cardiovascular Medicine, Expert Reviews on Cardiovascular Research] | * [http://www.themdtv.org The MD TV: Comments on Hot Topics, State of the Art Presentations in Cardiovascular Medicine, Expert Reviews on Cardiovascular Research] | ||
* [http://www.clinicaltrialresults.org Clinical Trial Results: An up to date resource of Cardiovascular Research] | * [http://www.clinicaltrialresults.org Clinical Trial Results: An up to date resource of Cardiovascular Research] | ||
| Line 32: | Line 39: | ||
{{STEMI}} | {{STEMI}} | ||
{{WikiDoc Help Menu}} | |||
{{WikiDoc Sources}} | |||
[[Category:Disease]] | |||
[[Category:Cardiology]] | |||
[[Category:Ischemic heart diseases]] | |||
[[Category:Intensive care medicine]] | |||
[[Category:Emergency medicine]] | [[Category:Emergency medicine]] | ||
[[Category: | [[Category:Mature chapter]] | ||
Latest revision as of 00:17, 30 July 2020
|
ST Elevation Myocardial Infarction Microchapters |
|
Differentiating ST elevation myocardial infarction from other Diseases |
|
Diagnosis |
|
Treatment |
|
|
Case Studies |
|
ST elevation myocardial infarction initial care On the Web |
|
Directions to Hospitals Treating ST elevation myocardial infarction |
|
Risk calculators and risk factors for ST elevation myocardial infarction initial care |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
The goal of initial care of the STEMI patient is to restore epicardial artery patency as rapidly and fully as possible, and to reduce the risk of early vessel reocclusion. Other goals include reducing the risk of lethal ventricular arrhythmias and other mechanical complications as well as reducing myocardial oxygen demands to limit infarct size with beta blockers.
Overview of Initial Therapies
Initial therapies include oxygen, aspirin, nitroglycerin or glyceryl trinitrate (an important exception is if the patient has a right ventricular myocardial infarction) and analgesia (usually morphine). [1] Morphine is the preferred analgesic agent due to its ability to reduce adrenergic drive and reduce preload (it is a venodilator). NSAIDs and COX-2 inhibitors should be discontinued due to their association with higher rates of adverse events.[2] [3] The antiplatelet agent aspirin has been associated with a reduction in mortality and has limited adverse effects. [4] Full dose non-enteric coated aspirin (162 mg to 325 mg) should be administered to a STEMI patient who does not have a history of hypersensitivity to ASA as soon as possible. In the absence of cardiogenic shock or heart failure, a beta blocker should also be administered.
Once the diagnosis of myocardial infarction is confirmed and diagnoses that would contraindicate the administration of antithrombins such as aortic dissection and pericarditis have been excluded, antithrombin therapy should be initiated. [1]
Initial Care
Triage and transfer for PCI in STEMI:
You can read in greater detail about each of the therapies below in greater detail by clicking on the link for that therapy.
Oxygen | Nitrates | Analgesics | Aspirin | Beta Blockers | The coronary care unit | The step down unit
Sources
- The 2004 ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction [5]
- The 2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients with ST-Elevation Myocardial Infarction [6]
References
- ↑ 1.0 1.1 Antman EM, Anbe DT, Armstrong PW; et al. (2004). "ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction--executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction)". Circulation. 110 (5): 588–636. doi:10.1161/01.CIR.0000134791.68010.FA. PMID 15289388. Unknown parameter
|month=ignored (help) - ↑ C. Michael Gibson, Yuri B. Pride, Philip E. Aylward, Jacques J. Col, Shaun G. Goodman, Dietrich Gulba, Mijo Bergovec, Vijayalakshmi Kunadian, Cafer Zorkun, Jacqueline L. Buros, Sabina A. Murphy and Elliott M. Antman.Association of non-steroidal anti-inflammatory drugs with outcomes in patients with ST-segment elevation myocardial infarction treated with fibrinolytic therapy: an ExTRACT-TIMI 25 analysis. DOI10.1007/s11239-008-0264-4.
- ↑ Gaziano JM, Gibson CM (2006). "Potential for drug-drug interactions in patients taking analgesics for mild-to-moderate pain and low-dose aspirin for cardioprotection". Am. J. Cardiol. 97 (9A): 23–9. doi:10.1016/j.amjcard.2006.02.020. PMID 16675319. Unknown parameter
|month=ignored (help) - ↑ "Randomised trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. ISIS-2 (Second International Study of Infarct Survival) Collaborative Group". Lancet. 2 (8607): 349–60. 1988. PMID 2899772. Unknown parameter
|month=ignored (help) - ↑ Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC, Alpert JS, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Halperin JL, Hiratzka LF, Hunt SA, Jacobs AK (2004). "ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction)". Circulation. 110 (9): e82–292. PMID 15339869. Unknown parameter
|month=ignored (help) - ↑ Antman EM, Hand M, Armstrong PW; et al. (2008). "2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: developed in collaboration With the Canadian Cardiovascular Society endorsed by the American Academy of Family Physicians: 2007 Writing Group to Review New Evidence and Update the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction, Writing on Behalf of the 2004 Writing Committee". Circulation. 117 (2): 296–329. doi:10.1161/CIRCULATIONAHA.107.188209. PMID 18071078. Unknown parameter
|month=ignored (help)
External Links
- The MD TV: Comments on Hot Topics, State of the Art Presentations in Cardiovascular Medicine, Expert Reviews on Cardiovascular Research
- Clinical Trial Results: An up to date resource of Cardiovascular Research
- Risk Assessment Tool for Estimating Your 10-year Risk of Having a Heart Attack - based on information of the Framingham Heart Study, from the United States National Heart, Lung and Blood Institute
- Heart Attack - overview of resources from MedlinePlus.
- Heart Attack Warning Signals from the Heart and Stroke Foundation of Canada
- Regional PCI for STEMI Resource Center - Evidence based online resource center for the development of regional PCI networks for acute STEMI
- STEMI Systems - Articles, profiles, and reviews of the latest publications involved in STEMI care. Quarterly newsletter.
- American College of Cardiology (ACC) Door to Balloon (D2B) Initiative.
- American Heart Association's Heart Attack web site - Information and resources for preventing, recognizing and treating heart attack.