Rocky Mountain spotted fever natural history
|
Rocky Mountain spotted fever Microchapters |
|
Differentiating Rocky Mountain spotted fever from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Rocky Mountain spotted fever natural history On the Web |
|
American Roentgen Ray Society Images of Rocky Mountain spotted fever natural history |
|
Directions to Hospitals Treating Rocky Mountain spotted fever |
|
Risk calculators and risk factors for Rocky Mountain spotted fever natural history |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Ilan Dock, B.S.
Overview
Rocky Mountain spotted fever, like all rickettsial infections, is classified as a zoonosis. Zoonoses are diseases of animals that can be transmitted to humans. Many zoonotic diseases require a vector (e.g., a mosquito, tick, or mite) in order to be transmitted from the animal host to the human host. In the case of Rocky Mountain spotted fever, ticks are the natural hosts, serving as both reservoirs and vectors of R. rickettsii. Ticks transmit the organism to vertebrates primarily by their bite. Less commonly, infections may occur following exposure to crushed tick tissues, fluids, or tick feces.
A female tick can transmit R. rickettsii to her eggs in a process called transovarial transmission. Ticks can also become infected with R. rickettsii while feeding on blood from the host in either the larval or nymphal stage. After the tick develops into the next stage, the R. rickettsii may be transmitted to the second host during the feeding process. Male ticks may transfer R. rickettsii to female ticks through body fluids or spermatozoa during the mating process. These types of transmission represent how generations or life stages of infected ticks are maintained. Once infected, the tick can carry the pathogen for life.
Natural history
Early Onset Symptoms (2-14 days after infected tick bite):
- Fever
- Vomiting
- Nausea
- Severe Headache
- Muscular Soreness and Pain
- Anorexia
- Rash<ref= “Austin RMSF”> Mills, Jackie. Rocky Mountain Spotted Fever. Austin CC. Derived: Masters, E. J., G. S. Olson, S. J. Weiner, and C. D. Paddock. 2003. Rocky Mountain spotted fever: a clinician’s dilemma. Archive of Internal Medicine 163:769–774. http://archinte.ama-assn.org/cgi/content/full/163/7/769 Accessed January 11, 2016</ref>
Late Stage:
Untreated or Improperly Diagnosed:
- Gangrene
- ARDS
- Myocarditis
- Acute Renal Failure
- Meningoencephalitis
- Pulmonary hemorrhaging
- Pulmonary Edema
- Cerebral Edema
- Death <ref= “Austin RMSF”> Mills, Jackie. Rocky Mountain Spotted Fever. Austin CC. Derived: Masters, E. J., G. S. Olson, S. J. Weiner, and C. D. Paddock. 2003. Rocky Mountain spotted fever: a clinician’s dilemma. Archive of Internal Medicine 163:769–774. http://archinte.ama-assn.org/cgi/content/full/163/7/769 Accessed January 11, 2016</ref>
Complications
Possible complications include:
- Meningitis
- Brain damage
- Clotting problems
- Heart failure
- Kidney failure
- Lung failure
- Adult Respiratory Distress Syndrome
- Pneumonitis (lung inflammation)
- Encephalitis
- Noncardiogenic pulmonary edema
- Cardiac arrythmia
- Impaired blood clotting
- Skin Necrosis
- Gastrointestinal Bleeding
- Shock[1][2]
Long term complications:
- Paralysis of lower extremities
- Impaired bladder function
- Impaired bowel function
- Amputation
- Hearing impairment
- Speech Disorders[1]
Prognosis
- Treatment usually cures the infection.
- Complications can include paralysis, hearing loss, nerve damage, and, if left untreated or treated but less commonly occurring, death.
- Rocky Mountain spotted fever can be a severe illness, and the majority of patients are hospitalized.
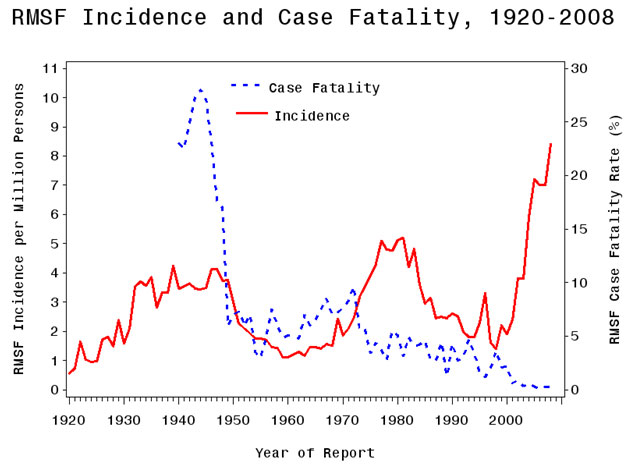
- Prior to the development of tetracycline and chloramphenicol, antibiotics, Rocky mountain spotted fever's mortality rate was as high as 87%. Now, with new medical practices including the implementation of antibiotic therapies, the mortality rate is approximately 20% if untreated and 5% if treated properly. [3]
- Infection with R. rickettsii may provide long lasting immunity against re-infection.
- Previous infection with Rocky Mountain spotted fever should not deter persons from practicing good tick-preventive measures or visiting a physician if signs and symptoms consistent with Rocky Mountain spotted fever occur, especially following a tick bite, as other diseases may also be transmitted by ticks. [4]
Illness Severity
Initial health problems
- Rocky Mountain spotted fever can be a very severe illness and patients often require hospitalization. Because R. rickettsii infects the cells lining blood vessels throughout the body, severe manifestations of this disease may involve the respiratory system, central nervous system, gastrointestinal system, or renal system.
- Host factors associated with severe or fatal Rocky Mountain spotted fever include advanced age, male sex, African-American race, chronic alcohol abuse, and
glucose-6-phosphate dehydrogenase (G6PD) deficiency.
- Deficiency of G6PD is a sex-linked genetic condition affecting approximately 12% of the U.S.
- African-American male population; deficiency of this enzyme is associated with a high proportion of severe cases of Rocky Mountain spotted fever. This is a rare clinical course that is often fatal within 5 days of onset of illness. [5]
- Long-term health problems following acute Rocky Mountain spotted fever infection include partial paralysis of the lower extremities, gangrene requiring amputation of fingers, toes, or arms or legs, hearing loss, loss of bowel or bladder control, movement disorders, and language disorders.
- These complications are most frequent in persons recovering from severe, life-threatening disease, often following lengthy hospitalizations. [5]
Long term health problems
- Patients who had a particularly severe infection requiring prolonged hospitalization may have long-term health problems caused by this disease.
- Rickettsia rickettsii infects the endothelial cells that line the blood vessels.
- The damage that occurs in the blood vessels results in a disease process called a "vasculitis", and bleeding or clotting in the brain or other vital organs may occur. *Loss of fluid from damaged vessels can result in loss of circulation to the extremities and damaged fingers, toes or even limbs may ultimately need to be amputated. *Patients who suffer this kind of severe vasculitis in the first two weeks of illness may also be left with permanent long-term health problems such as profound neurological deficits, or damage to internal organs.
- Those who do not have this kind of vascular damage in the initial stages of the disease typically recover fully within several days to months. [5]
References
- ↑ 1.0 1.1 Rocky Mountain Spotted Fever general information. American Lyme Disease Foundation (2016). Accessed on January 11, 2016
- ↑ Rocky Mountain Spotted Fever Symptoms. Centers for Disease Control and Prevention (2015). http://www.cdc.gov/rmsf/symptoms/index.html Accessed on December 30, 2015
- ↑ Dantas-Torres, Filipe. Lancet Infect Disease 2007;7:724-32. Department of Immunology, Center of Research Aggeu Magalhaes, Oswaldo Cruz Foundation. Recife Pernambuco, Brazil. Volume 7, November 2007. Accessed on January 11, 2016
- ↑ Rocky Moutnain Spotted Fever. Department of Health. Idaho Health District 4. http://www.cdhd.idaho.gov/CD/public/factsheets/rockymtnspottedfever.htm Accessed on January 11, 2016
- ↑ 5.0 5.1 5.2 Rocky Mountain Spotted Fever Symptoms. Centers for Disease Control and Prevention (2015). http://www.cdc.gov/rmsf/symptoms/index.html Accessed on December 30, 2015