Rocky Mountain spotted fever pathophysiology
|
Rocky Mountain spotted fever Microchapters |
|
Differentiating Rocky Mountain spotted fever from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Rocky Mountain spotted fever pathophysiology On the Web |
|
American Roentgen Ray Society Images of Rocky Mountain spotted fever pathophysiology |
|
Directions to Hospitals Treating Rocky Mountain spotted fever |
|
Risk calculators and risk factors for Rocky Mountain spotted fever pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Ilan Dock, B.S.
Overview
Rocky Mountain spotted fever is caused by a bacterial organism of the Rickettsia genus known as Rickettsia ricketsii. The organism is a Gram-negative bacteria, ranging in sizes between 0.2 x 0.5 micrometers to 0.3 x 2.0 micrometers. Rickettsia ricketsii is non-spore forming, non- motile, and varies in shape. Early in it's life cycle, Rickettsia ricketsii survives within an invertebrate host. The invertebrate host may then transmit the organism through blood meals, open skin, and breakages in mucous barriers. [1] The disease is most often transmitted through arthropod vectors, especially the hard tick- Ixodidae family. Rickettsia ricketsii requires an invertebrate vector and vertebrate host. Humans are considered an accidental host within the R. ricketsii life cycle. The organism has evolved a set of strategic mechanisms in order to evade the human immune system. Infection begins with an induced phagocytosis of the organism into an endothelial host cell. Usually endothelial cells are not phagocytic, however R. ricketsii is able to induce changes to the overall cytoskeleton of the cell. Invasion goes largely unnoticed, enabling the organism to avoid lysosomal fusion and an escape into the cytoplasm for future reproduction. [2]
Pathogenesis
- Rocky Mountain spotted fever is caused by Rickettsia rickettsii, a small bacterium that grows inside the cells of its hosts.
- These bacteria range in size from 0.2 x 0.5 μm to 0.3 x 2 μm.
- The bacteria is a pleomorphic Gram-negative coccobacillus organism. [3]
- Cell wall and lipopolysaccharide resembles those of the average gram-negative bacteria. [3]
- They are difficult to see in tissues by using routine histologic stains and generally require the use of special staining methods.
- In the human body, rickettsiae live and multiply primarily within cells that line small- to medium-sized blood vessels.
- Spotted fever group rickettsiae can grow in the cytoplasm or in the nucleus of the host cell.
- Once inside the host, the rickettsiae multiply, resulting in damage and death to these cells.
- This causes blood to leak through tiny holes in vessel walls into adjacent tissues.
- In turn, the leakage process causes the rash that is traditionally associated with Rocky Mountain spotted fever and also causes damage to organs and tissues. [1]
Pathogen life cycle
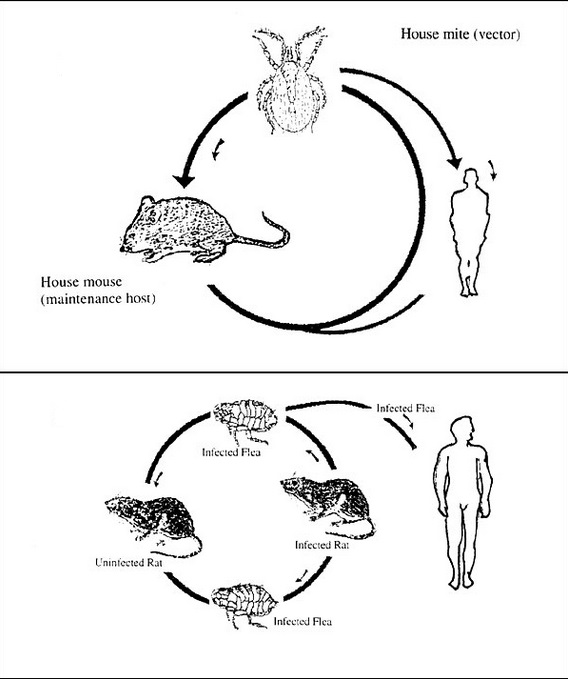
The life cycle of Rickettsia rickettsii is considered to be a complex one. Survival is dependent on both an invertebrate vector, (the hard tick- Family Ixodidae) and a vertebrate host (including mice, dogs, rabbits). Humans are considered to be accidental vectors and are not essential in the rickettsial cycle. In addition, a sequence of events occur between both hosts in the successful transmission of rickettsial disease.
Rickettsia rickettsii mostly affects canines and humans.
Transmission in arthropod vectors
- Three arthropod vectors in the United States have been identified in transmitting R. rickettsii to humans, causing the potentially fatal disease Rocky Mountain spotted fever. The American Dog Tick (Dermacentor variabilis), the Rocky Mountain Wood Tick (Dermacentor andersoni), and the Brown Dog Tick (Rhipicephalus sanguineus) can acquire Rickettsia rickettsii in a number of different ways.
- First, an uninfected tick can become infected when feeding on the blood of an infected mammalian host in the larval or nymph stages, a mode of transmission called transstadial transmission. Once a tick becomes infected with this pathogen, they are infected for life.
- Both the American dog tick and the Rocky Mountain Wood Tick serve as long-term reservoirs for Rickettsia rickettsii, in which the organism resides in the tick posterior diverticulae of the midgut, the small intestine and the ovaries.
- Due to its confinement in the midgut and small intestine, it is possible for mammals, including humans, to contract rickettsial disease from open skin/wound contact with the feces of the organism. In addition, an infected male tick can transmit the organism to an uninfected female during mating.
- Once infected, the female tick can transmit the infection to her offspring, in a process known as transovarial transmission. [2]
Transmission in mammals
- An uninfected mammal can become infected with Rickettsia rickettsii when eating food that contains the feces of the infected tick. They can also be infected through the bite of an infected tick.
- Humans acquire Rickettsia rickettsii infection from infected vectors. After getting bitten by an infected tick, rickettsiae are transmitted to the bloodstream by tick salivary secretions or, as mentioned previously, through contamination of broken skin by an infected vector's feces.
- All these modes of transmission ensure the survival of Rickettsia. [4]
Virulence
- R. rickettsii have evolved a number of strategical mechanisms or virulence factors that allow them to evade the host immune system and successfully infect the host. [2]
- R. rickettsii invades the endothelial cells that line the blood vessels. Endothelial cells are not phagocytic in nature; however, after attachment to the host cell surface, the pathogen causes changes in the host cell cytoskeleton that induces phagocytosis. They are able to avoid lysosomal fusion and oxidative burst by escaping from the phagosome into the cytoplasm where they multiply and spread.
- This invasion can cause significant endothelial damage that can lead to end organ failure, DIC, and even death.
OmpA and OmpB
- OmpA (rOmp) and Omp B (rOmp) have been identified as rickettsial outer surface proteins and are implicated in adherence of the bacterium to the host cell.
- The genes that encode these two surface proteins are designated as ompA and ompB, respectively.
- rOmp B is the predominant surface membrane protein in R. rickettsii; Policastro et al., identified the rOmpA to rOmpB ratio to be 1:9 (1994).[5]
- While the surface proteins of the bacterium have been identified, the host cell protein receptor(s) have not.
T4SS
- Entry into the host cell is mediated by a Type 4 secretion system' (T4SS) which is found in all Rickettsiae.
- The T4SS apparatus is a tunnel-shaped structure that is embedded in the bacterial inner membrane and extends to the outer membrane. At least 12 or more proteins help form the tunnel-like apparatus.
- Once adherence to the host cell is established, the T4SS of Rickettsiae recruits substrates to the bottom of the apparatus, activating the complex via an ATP-dependent process that results in the direct transfer of the bacterium's DNA and other proteins into the host cell.
Phospholipase A2
- Invasion of the host endothelial cell immediately triggers phagocytosis, where the rickettsiae escape from the phagosome and into the cytosol where replication takes place. Although the escape from the phagosome is not well understood, it is thought to be mediated by phospholipase A2 activity.
Actin polymerization
- In the cytosol, the virulence factor Sca2 (Surface Cell Antigen 2) and the protein RickA form an actin tail that provides motility.
- RickA is thought to be responsible for directing the actin-based motility in R. rickettsii.
- RickA has been shown to activate the Arp2/3 complex in vitro, but "R. raoulti" expresses RickA and does not have acting-based motility.[6]
- The Sca2 virulence factor has been shown to be essential for actin tail formation in "R.rickettsii" Listeria. Comparisons of actin motility mechanisms appears to be independently evolved in Listeria, Shigella, and Rickettsia.
- The actin tail in R. rickettsii is both longer and provides a straighter trajectory due the production of linear actin filaments.[7] The actin-based motility of R. rickettsii allows swift, unidirectional movement across the cytoplasm into adjacent cells, promoting cell to cell spread.
References
- ↑ 1.0 1.1 Walker, David H. Medical Microbiology 4th Edition. Chapter 38. Rickettsiae. (1996). http://www.ncbi.nlm.nih.gov/books/NBK7624/#A2139 Accessed on January 7, 2016
- ↑ 2.0 2.1 2.2 Azad, F. Abdu; Beard, B. Charles. Ricketssial Pathogens and their Arthropod Vectors (1998). http://wwwnc.cdc.gov/eid/article/4/2/pdfs/98-0205.pdf Accessed on January 7, 2016
- ↑ 3.0 3.1 Dantas-Torres, Filipe. Lancet Infect Disease 2007;7:724-32. Department of Immunology, Center of Research Aggeu Magalhaes, Oswaldo Cruz Foundation. Recife Pernambuco, Brazil. Volume 7, November 2007. Accessed on January 11, 2016
- ↑ Rocky Moutnain Spotted Fever. Department of Health. Information for a Healthy New York. https://www.health.ny.gov/diseases/communicable/rocky_mountain_spotted_fever/fact_sheet.htm Accessed on January 11, 2016
- ↑ Policastro PF, Hackstadt T (November 1994). "Differential activity of Rickettsia rickettsii opmA and ompB promoter regions in a heterologous reporter gene system" (PDF). Microbiology (Reading, Engl.). 140 (11): 2941–9. doi:10.1099/13500872-140-11-2941. PMID 7812435.
- ↑ Kleba, Betsy; Tina R. Clark; Erika I. Lutter; Damon W. Ellison; Ted Hackstadt (March 1, 2010). "Disruption of the Rickettsia rickettsii Sca2 Autotransporter Inhibits Actin-Based Motility". Infection and Immunity. 78 (5): 2240–7. doi:10.1128/IAI.00100-10. PMC 2863521. PMID 20194597. Retrieved March 9, 2014.
- ↑ Goldberg, Marcia (December 2001). "Actin-Based Motility of Intracellular Microbial Pathogens". MICROBIOLOGY AND MOLECULAR BIOLOGY REVIEWS. 65 (4): 31. doi:10.1128/MMBR.65.4.595-626.2001. PMC 99042. PMID 11729265. Retrieved March 9, 2014.