Pulmonary alveolar proteinosis
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Your Name
Synonyms and keywords: Synonym 1; Synonym 2; Synonym 3
Overview
Pulmonary alveolar proteinosis -(PAP) is a rare lung disease in which abnormal accumulation of surfactant occurs within the alveoli, interfering with gas exchange. PAP can occur in a primary form or secondarily in the settings of malignancy (especially in myeloid leukemia), pulmonary infection, or environmental exposure to dusts or chemicals. Rare familial forms have also been recognized, suggesting a genetic component in some cases. [1] [2] [3] [4]
Historical Perspective
PAP was first described in 1958 by the physicians Samuel Rosen, Benjamin Castleman, and Averill Liebow. In their case series published in the New England Journal of Medicine on June 7th of that year, they described 27 patients with pathologic evidence of periodic acid Schiff positive material filling the alveoli. This lipid rich material was subsequently recognized to be surfactant.
Pathophysiology
Although the cause of PAP remains obscure, a major breakthrough in the understanding of the etiology of the disease came by the chance observation that mice bred for experimental study to lack a hematologic growth factor known as granulocyte-macrophage colony stimulating factor (GM-CSF) developed a pulmonary syndrome of abnormal surfactant accumulation resembling human PAP. The implications of this finding are still being explored, but significant progress was reported in February, 2007. Researchers in that report discussed the presence of anti-GM-CSF autoantibodies in patients with PAP, and duplicated that syndrome with the infusion of these autoantibodies into mice. [5]
Causes
Pulmonary alveolar proteinosis is an idiopathic disease, but studies have linked causes to production of antibodies that neutralize GM-CSF, granulocyte-macrophage colony-stimulating factor. Occasionally, development of pulmonary alveolar proteinosis is related to exposure of toxic substances, such as inorganic dusts, infection with Pneumocystis jirovecii, certain cancers, and immunosuppressants. It rarely occurs in newborns.
There are several types of clinical forms of Pulmonary alveolar proteinosis; primary, secondary, and congenital. Primary PAP involves high levels of antibodies that neutralize GM-CSF, granulocyte-macrophage colony-stimulating factor. Secondary PAP occurs from clinical conditions that reduce the numbers and functions of alveolar macrophages. Congenital PAP is due to genetic mutations in the genes encoding surfactant proteins of the receptor for granulocyte-macrophage colony-stimulating factor.[6]
Causes
Common Causes
- Pneumocystis jirovecii
- Respiratory failure
- Uncontrolled infection
- Respiratory Pathogens
- Opportunistic Pathogens: Nocardia
- Sirolimus
- Prednisone
- Inorganic dusts
- Inhalation of silica dust
- Exposure to insecticides
- aluminum dust
- titanium dioxide
- Haematological malignancies
- HIV infection.
Causes by Organ System
| Cardiovascular | No underlying causes |
| Chemical / poisoning | No underlying causes |
| Dermatologic | No underlying causes |
| Drug Side Effect | Sirolimus, Prednisone |
| Ear Nose Throat | No underlying causes |
| Endocrine | No underlying causes |
| Environmental | Inorganic dusts, Inhalation of silica dust, Exposure to insecticides, aluminum dust, titanium dioxide |
| Gastroenterologic | No underlying causes |
| Genetic | No underlying causes |
| Hematologic | Haematological malignancies |
| Iatrogenic | No underlying causes |
| Infectious Disease | Uncontrolled infection, Respiratory Pathogens, Nocardia, HIV infection |
| Musculoskeletal / Ortho | [No underlying causes |
| Neurologic | No underlying causes |
| Nutritional / Metabolic | No underlying causes |
| Obstetric/Gynecologic | No underlying causes |
| Oncologic | Haematological malignancies |
| Opthalmologic | No underlying causes |
| Overdose / Toxicity | No underlying causes |
| Psychiatric | No underlying causes |
| Pulmonary | Pneumocystis jirovecii, Respiratory failure |
| Renal / Electrolyte | No underlying causes |
| Rheum / Immune / Allergy | No underlying causes |
| Sexual | No underlying causes |
| Trauma | No underlying causes |
| Urologic | No underlying causes |
| Dental | No underlying causes |
| Miscellaneous | No underlying causes |
Causes in Alphabetical Order
|
Natural History
The clinical course of PAP is unpredictable. Spontaneous remission is recognized; some patients have stable symptoms.
Complications
Death may occur due to progression of PAP or due to the underlying disease associated with PAP. Individuals with PAP are more vulnerable to infection of the lung by bacteria or fungi.
Prognosis
History and Symptoms
The symptoms of PAP include:
Chest X Ray
Classic radiographic finding is bilateral, symmetric alveolar consolidation or ground-glass opacity, particularly in a perihilar or hilar distribution resembling pulmonary edema.
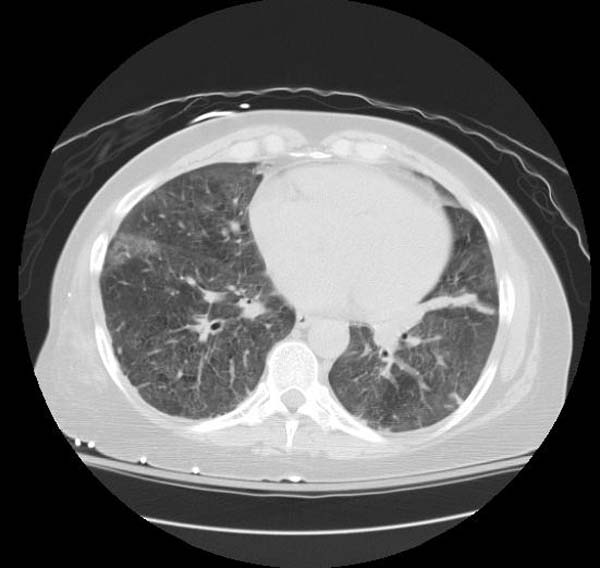
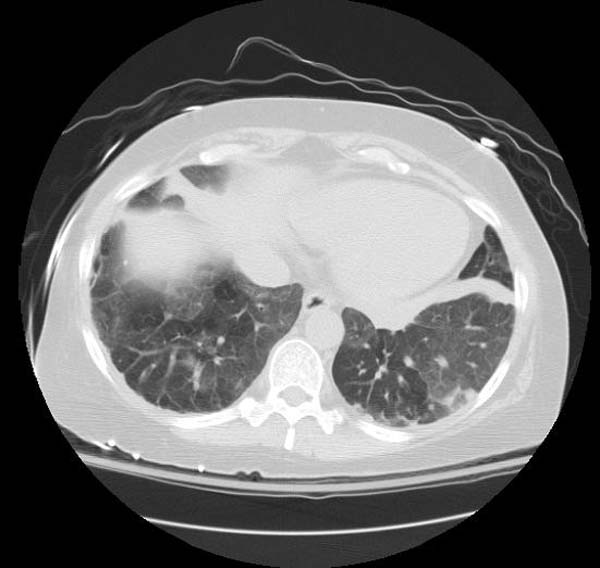
CT
- CT typically shows diffuse ground-glass attenuation with superimposed crazy-paving pattern (intra- and interlobular septal thickening, often in polygonal shapes representing the secondary pulmonary lobule).
Patient#1
Patient #1: Proven PAP but not quite the classic crazy-paving pattern
Other Diagnostic Studies
Diagnosis is generally made by surgical or endoscopic biopsy of the lung, revealing the distinctive pathologic finding.
Histopathological Findings: Pulmonary alveolar proteinosis
{{#ev:youtube|L9fVRzcPkEQ}}
Medical Therapy
The use of GM-CSF injections has also been attempted, with variable success.
Surgery
The standard treatment for PAP is whole-lung lavage, in which sterile fluid is instilled into the lung and then removed, along with the abnormal surfactant material. This is generally effective at ameliorating symptoms, often for prolonged periods. Lung transplantation can be performed in refractory cases.
References
- ↑ Rosen SH, Castleman B, and Liebow AA. Pulmonary alveolar proteinosis. New England Journal of Medicine 1958; 258: 1123-1142.
- ↑ Seymour JF and Presneill JJ. Pulmonary alveolar proteinosis: progress in the first 44 years. American Journal of Respiratory and Critical Care Medicine 2002; 166: 215-235.
- ↑ Shah PL, Hansell D, Lawson PR, et al. Pulmonary alveolar proteinosis; clinical aspects and current concepts on pathogenesis. Thorax 2000; 55: 67-77.
- ↑ Stanley E, Lieschke GJ, Grail D, et al. Granulocyte/macrophage colony-stimulating factor-deficient mice show no major perturbation of hematopoiesis but develop a characteristic pulmonary pathology. Proc. Natl. Acad. Sci. USA 1994; 91: 5592-5596.
- ↑ Uchida K, Beck D, Yamamoto T, Berclaz P, Abe S, Staudt M, Carey B, Filippi M, Wert S, Denson L, Puchalski J, Hauck D, Trapnell B (2007). "GM-CSF autoantibodies and neutrophil dysfunction in pulmonary alveolar proteinosis". N Engl J Med. 356 (6): 567–79. PMID 17287477.
- ↑ 6.0 6.1 Trapnell BC, Whitsett JA, Nakata K (2003). "Pulmonary alveolar proteinosis". N Engl J Med. 349 (26): 2527–39. doi:10.1056/NEJMra023226. PMID 14695413.