Pulmonary alveolar proteinosis: Difference between revisions
(Created page with "__NOTOC__ {{SI}} {{CMG}} {{AE}} Your Name {{SK}} Synonym 1; Synonym 2; Synonym 3 ==Overview== '''Pulmona...") |
No edit summary |
||
| Line 4: | Line 4: | ||
{{SK}} Synonym 1; Synonym 2; Synonym 3 | {{SK}} Synonym 1; Synonym 2; Synonym 3 | ||
==Overview== | |||
==Historical Perspective== | |||
*[Disease name] was first discovered by [scientist name], a [nationality + occupation], in [year] during/following [event]. | |||
*In [year], [gene] mutations were first identified in the pathogenesis of [disease name]. | |||
*In [year], the first [discovery] was developed by [scientist] to treat/diagnose [disease name]. | |||
==Classification== | |||
*[Disease name] may be classified according to [classification method] into [number] subtypes/groups: | |||
:*[group1] | |||
:*[group2] | |||
:*[group3] | |||
*Other variants of [disease name] include [disease subtype 1], [disease subtype 2], and [disease subtype 3]. | |||
==Pathophysiology== | |||
*The pathogenesis of [disease name] is characterized by [feature1], [feature2], and [feature3]. | |||
*The [gene name] gene/Mutation in [gene name] has been associated with the development of [disease name], involving the [molecular pathway] pathway. | |||
*On gross pathology, [feature1], [feature2], and [feature3] are characteristic findings of [disease name]. | |||
*On microscopic histopathological analysis, [feature1], [feature2], and [feature3] are characteristic findings of [disease name]. | |||
==Causes== | |||
* [Disease name] may be caused by either [cause1], [cause2], or [cause3]. | |||
* [Disease name] is caused by a mutation in the [gene1], [gene2], or [gene3] gene[s]. | |||
* There are no established causes for [disease name]. | |||
==Differentiating [disease name] from other Diseases== | |||
*[Disease name] must be differentiated from other diseases that cause [clinical feature 1], [clinical feature 2], and [clinical feature 3], such as: | |||
:*[Differential dx1] | |||
:*[Differential dx2] | |||
:*[Differential dx3] | |||
==Epidemiology and Demographics== | |||
* The prevalence of [disease name] is approximately [number or range] per 100,000 individuals worldwide. | |||
* In [year], the incidence of [disease name] was estimated to be [number or range] cases per 100,000 individuals in [location]. | |||
===Age=== | |||
*Patients of all age groups may develop [disease name]. | |||
*[Disease name] is more commonly observed among patients aged [age range] years old. | |||
*[Disease name] is more commonly observed among [elderly patients/young patients/children]. | |||
===Gender=== | |||
*[Disease name] affects men and women equally. | |||
*[Gender 1] are more commonly affected with [disease name] than [gender 2]. | |||
* The [gender 1] to [Gender 2] ratio is approximately [number > 1] to 1. | |||
===Race=== | |||
*There is no racial predilection for [disease name]. | |||
*[Disease name] usually affects individuals of the [race 1] race. | |||
*[Race 2] individuals are less likely to develop [disease name]. | |||
==Risk Factors== | |||
*Common risk factors in the development of [disease name] are [risk factor 1], [risk factor 2], [risk factor 3], and [risk factor 4]. | |||
== Natural History, Complications and Prognosis== | |||
*The majority of patients with [disease name] remain asymptomatic for [duration/years]. | |||
*Early clinical features include [manifestation 1], [manifestation 2], and [manifestation 3]. | |||
*If left untreated, [#%] of patients with [disease name] may progress to develop [manifestation 1], [manifestation 2], and [manifestation 3]. | |||
*Common complications of [disease name] include [complication 1], [complication 2], and [complication 3]. | |||
*Prognosis is generally [excellent/good/poor], and the [1/5/10year mortality/survival rate] of patients with [disease name] is approximately [#%]. | |||
== Diagnosis == | |||
===Diagnostic Criteria=== | |||
*The diagnosis of [disease name] is made when at least [number] of the following [number] diagnostic criteria are met: | |||
:*[criterion 1] | |||
:*[criterion 2] | |||
:*[criterion 3] | |||
:*[criterion 4] | |||
=== Symptoms === | |||
*[Disease name] is usually asymptomatic. | |||
*Symptoms of [disease name] may include the following: | |||
:*[symptom 1] | |||
:*[symptom 2] | |||
:*[symptom 3] | |||
:*[symptom 4] | |||
:*[symptom 5] | |||
:*[symptom 6] | |||
=== Physical Examination === | |||
*Patients with [disease name] usually appear [general appearance]. | |||
*Physical examination may be remarkable for: | |||
:*[finding 1] | |||
:*[finding 2] | |||
:*[finding 3] | |||
:*[finding 4] | |||
:*[finding 5] | |||
:*[finding 6] | |||
=== Laboratory Findings === | |||
*There are no specific laboratory findings associated with [disease name]. | |||
*A [positive/negative] [test name] is diagnostic of [disease name]. | |||
*An [elevated/reduced] concentration of [serum/blood/urinary/CSF/other] [lab test] is diagnostic of [disease name]. | |||
*Other laboratory findings consistent with the diagnosis of [disease name] include [abnormal test 1], [abnormal test 2], and [abnormal test 3]. | |||
===Imaging Findings=== | |||
*There are no [imaging study] findings associated with [disease name]. | |||
*[Imaging study 1] is the imaging modality of choice for [disease name]. | |||
*On [imaging study 1], [disease name] is characterized by [finding 1], [finding 2], and [finding 3]. | |||
*[Imaging study 2] may demonstrate [finding 1], [finding 2], and [finding 3]. | |||
=== Other Diagnostic Studies === | |||
*[Disease name] may also be diagnosed using [diagnostic study name]. | |||
*Findings on [diagnostic study name] include [finding 1], [finding 2], and [finding 3]. | |||
== Treatment == | |||
=== Medical Therapy === | |||
*There is no treatment for [disease name]; the mainstay of therapy is supportive care. | |||
*The mainstay of therapy for [disease name] is [medical therapy 1] and [medical therapy 2]. | |||
*[Medical therapy 1] acts by [mechanism of action 1]. | |||
*Response to [medical therapy 1] can be monitored with [test/physical finding/imaging] every [frequency/duration]. | |||
=== Surgery === | |||
*Surgery is the mainstay of therapy for [disease name]. | |||
*[Surgical procedure] in conjunction with [chemotherapy/radiation] is the most common approach to the treatment of [disease name]. | |||
*[Surgical procedure] can only be performed for patients with [disease stage] [disease name]. | |||
=== Prevention === | |||
*There are no primary preventive measures available for [disease name]. | |||
*Effective measures for the primary prevention of [disease name] include [measure1], [measure2], and [measure3]. | |||
*Once diagnosed and successfully treated, patients with [disease name] are followed-up every [duration]. Follow-up testing includes [test 1], [test 2], and [test 3]. | |||
==References== | |||
{{Reflist|2}} | |||
[[Category:Pick One of 28 Approved]] | |||
{{WS}} | |||
{{WH}} | |||
==Overview== | ==Overview== | ||
Revision as of 20:33, 1 March 2018
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Your Name
Synonyms and keywords: Synonym 1; Synonym 2; Synonym 3
Overview
Historical Perspective
- [Disease name] was first discovered by [scientist name], a [nationality + occupation], in [year] during/following [event].
- In [year], [gene] mutations were first identified in the pathogenesis of [disease name].
- In [year], the first [discovery] was developed by [scientist] to treat/diagnose [disease name].
Classification
- [Disease name] may be classified according to [classification method] into [number] subtypes/groups:
- [group1]
- [group2]
- [group3]
- Other variants of [disease name] include [disease subtype 1], [disease subtype 2], and [disease subtype 3].
Pathophysiology
- The pathogenesis of [disease name] is characterized by [feature1], [feature2], and [feature3].
- The [gene name] gene/Mutation in [gene name] has been associated with the development of [disease name], involving the [molecular pathway] pathway.
- On gross pathology, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
- On microscopic histopathological analysis, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
Causes
- [Disease name] may be caused by either [cause1], [cause2], or [cause3].
- [Disease name] is caused by a mutation in the [gene1], [gene2], or [gene3] gene[s].
- There are no established causes for [disease name].
Differentiating [disease name] from other Diseases
- [Disease name] must be differentiated from other diseases that cause [clinical feature 1], [clinical feature 2], and [clinical feature 3], such as:
- [Differential dx1]
- [Differential dx2]
- [Differential dx3]
Epidemiology and Demographics
- The prevalence of [disease name] is approximately [number or range] per 100,000 individuals worldwide.
- In [year], the incidence of [disease name] was estimated to be [number or range] cases per 100,000 individuals in [location].
Age
- Patients of all age groups may develop [disease name].
- [Disease name] is more commonly observed among patients aged [age range] years old.
- [Disease name] is more commonly observed among [elderly patients/young patients/children].
Gender
- [Disease name] affects men and women equally.
- [Gender 1] are more commonly affected with [disease name] than [gender 2].
- The [gender 1] to [Gender 2] ratio is approximately [number > 1] to 1.
Race
- There is no racial predilection for [disease name].
- [Disease name] usually affects individuals of the [race 1] race.
- [Race 2] individuals are less likely to develop [disease name].
Risk Factors
- Common risk factors in the development of [disease name] are [risk factor 1], [risk factor 2], [risk factor 3], and [risk factor 4].
Natural History, Complications and Prognosis
- The majority of patients with [disease name] remain asymptomatic for [duration/years].
- Early clinical features include [manifestation 1], [manifestation 2], and [manifestation 3].
- If left untreated, [#%] of patients with [disease name] may progress to develop [manifestation 1], [manifestation 2], and [manifestation 3].
- Common complications of [disease name] include [complication 1], [complication 2], and [complication 3].
- Prognosis is generally [excellent/good/poor], and the [1/5/10year mortality/survival rate] of patients with [disease name] is approximately [#%].
Diagnosis
Diagnostic Criteria
- The diagnosis of [disease name] is made when at least [number] of the following [number] diagnostic criteria are met:
- [criterion 1]
- [criterion 2]
- [criterion 3]
- [criterion 4]
Symptoms
- [Disease name] is usually asymptomatic.
- Symptoms of [disease name] may include the following:
- [symptom 1]
- [symptom 2]
- [symptom 3]
- [symptom 4]
- [symptom 5]
- [symptom 6]
Physical Examination
- Patients with [disease name] usually appear [general appearance].
- Physical examination may be remarkable for:
- [finding 1]
- [finding 2]
- [finding 3]
- [finding 4]
- [finding 5]
- [finding 6]
Laboratory Findings
- There are no specific laboratory findings associated with [disease name].
- A [positive/negative] [test name] is diagnostic of [disease name].
- An [elevated/reduced] concentration of [serum/blood/urinary/CSF/other] [lab test] is diagnostic of [disease name].
- Other laboratory findings consistent with the diagnosis of [disease name] include [abnormal test 1], [abnormal test 2], and [abnormal test 3].
Imaging Findings
- There are no [imaging study] findings associated with [disease name].
- [Imaging study 1] is the imaging modality of choice for [disease name].
- On [imaging study 1], [disease name] is characterized by [finding 1], [finding 2], and [finding 3].
- [Imaging study 2] may demonstrate [finding 1], [finding 2], and [finding 3].
Other Diagnostic Studies
- [Disease name] may also be diagnosed using [diagnostic study name].
- Findings on [diagnostic study name] include [finding 1], [finding 2], and [finding 3].
Treatment
Medical Therapy
- There is no treatment for [disease name]; the mainstay of therapy is supportive care.
- The mainstay of therapy for [disease name] is [medical therapy 1] and [medical therapy 2].
- [Medical therapy 1] acts by [mechanism of action 1].
- Response to [medical therapy 1] can be monitored with [test/physical finding/imaging] every [frequency/duration].
Surgery
- Surgery is the mainstay of therapy for [disease name].
- [Surgical procedure] in conjunction with [chemotherapy/radiation] is the most common approach to the treatment of [disease name].
- [Surgical procedure] can only be performed for patients with [disease stage] [disease name].
Prevention
- There are no primary preventive measures available for [disease name].
- Effective measures for the primary prevention of [disease name] include [measure1], [measure2], and [measure3].
- Once diagnosed and successfully treated, patients with [disease name] are followed-up every [duration]. Follow-up testing includes [test 1], [test 2], and [test 3].
References
Overview
Pulmonary alveolar proteinosis -(PAP) is a rare lung disease in which abnormal accumulation of surfactant occurs within the alveoli, interfering with gas exchange. PAP can occur in a primary form or secondarily in the settings of malignancy (especially in myeloid leukemia), pulmonary infection, or environmental exposure to dusts or chemicals. Rare familial forms have also been recognized, suggesting a genetic component in some cases. [1] [2] [3] [4]
Historical Perspective
PAP was first described in 1958 by the physicians Samuel Rosen, Benjamin Castleman, and Averill Liebow. In their case series published in the New England Journal of Medicine on June 7th of that year, they described 27 patients with pathologic evidence of periodic acid Schiff positive material filling the alveoli. This lipid rich material was subsequently recognized to be surfactant.
Pathophysiology
Although the cause of PAP remains obscure, a major breakthrough in the understanding of the etiology of the disease came by the chance observation that mice bred for experimental study to lack a hematologic growth factor known as granulocyte-macrophage colony stimulating factor (GM-CSF) developed a pulmonary syndrome of abnormal surfactant accumulation resembling human PAP. The implications of this finding are still being explored, but significant progress was reported in February, 2007. Researchers in that report discussed the presence of anti-GM-CSF autoantibodies in patients with PAP, and duplicated that syndrome with the infusion of these autoantibodies into mice. [5]
Causes
Pulmonary alveolar proteinosis is an idiopathic disease, but studies have linked causes to production of antibodies that neutralize GM-CSF, granulocyte-macrophage colony-stimulating factor. Occasionally, development of pulmonary alveolar proteinosis is related to exposure of toxic substances, such as inorganic dusts, infection with Pneumocystis jirovecii, certain cancers, and immunosuppressants. It rarely occurs in newborns.
There are several types of clinical forms of Pulmonary alveolar proteinosis; primary, secondary, and congenital. Primary PAP involves high levels of antibodies that neutralize GM-CSF, granulocyte-macrophage colony-stimulating factor. Secondary PAP occurs from clinical conditions that reduce the numbers and functions of alveolar macrophages. Congenital PAP is due to genetic mutations in the genes encoding surfactant proteins of the receptor for granulocyte-macrophage colony-stimulating factor.[6]
Causes
Common Causes
- Pneumocystis jirovecii
- Respiratory failure
- Uncontrolled infection
- Respiratory Pathogens
- Opportunistic Pathogens: Nocardia
- Sirolimus
- Prednisone
- Inorganic dusts
- Inhalation of silica dust
- Exposure to insecticides
- aluminum dust
- titanium dioxide
- Haematological malignancies
- HIV infection.
Causes by Organ System
| Cardiovascular | No underlying causes |
| Chemical / poisoning | No underlying causes |
| Dermatologic | No underlying causes |
| Drug Side Effect | Sirolimus, Prednisone |
| Ear Nose Throat | No underlying causes |
| Endocrine | No underlying causes |
| Environmental | Inorganic dusts, Inhalation of silica dust, Exposure to insecticides, aluminum dust, titanium dioxide |
| Gastroenterologic | No underlying causes |
| Genetic | No underlying causes |
| Hematologic | Haematological malignancies |
| Iatrogenic | No underlying causes |
| Infectious Disease | Uncontrolled infection, Respiratory Pathogens, Nocardia, HIV infection |
| Musculoskeletal / Ortho | [No underlying causes |
| Neurologic | No underlying causes |
| Nutritional / Metabolic | No underlying causes |
| Obstetric/Gynecologic | No underlying causes |
| Oncologic | Haematological malignancies |
| Opthalmologic | No underlying causes |
| Overdose / Toxicity | No underlying causes |
| Psychiatric | No underlying causes |
| Pulmonary | Pneumocystis jirovecii, Respiratory failure |
| Renal / Electrolyte | No underlying causes |
| Rheum / Immune / Allergy | No underlying causes |
| Sexual | No underlying causes |
| Trauma | No underlying causes |
| Urologic | No underlying causes |
| Dental | No underlying causes |
| Miscellaneous | No underlying causes |
Causes in Alphabetical Order
|
Natural History
The clinical course of PAP is unpredictable. Spontaneous remission is recognized; some patients have stable symptoms.
Complications
Death may occur due to progression of PAP or due to the underlying disease associated with PAP. Individuals with PAP are more vulnerable to infection of the lung by bacteria or fungi.
Prognosis
History and Symptoms
The symptoms of PAP include:
Chest X Ray
Classic radiographic finding is bilateral, symmetric alveolar consolidation or ground-glass opacity, particularly in a perihilar or hilar distribution resembling pulmonary edema.
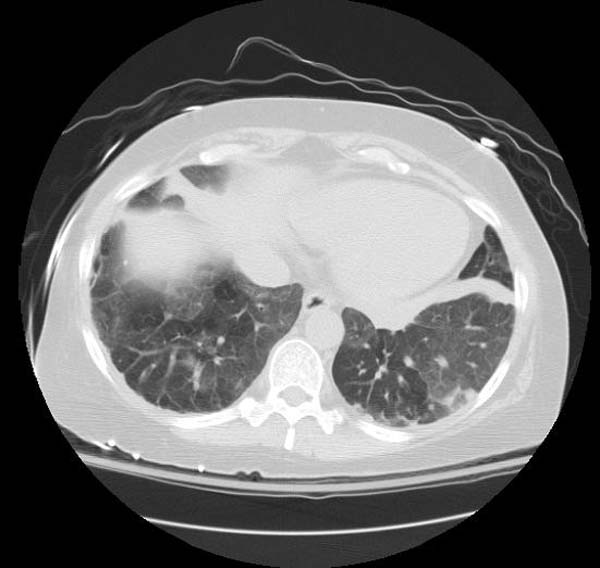
CT
- CT typically shows diffuse ground-glass attenuation with superimposed crazy-paving pattern (intra- and interlobular septal thickening, often in polygonal shapes representing the secondary pulmonary lobule).
Patient#1
Patient #1: Proven PAP but not quite the classic crazy-paving pattern
Other Diagnostic Studies
Diagnosis is generally made by surgical or endoscopic biopsy of the lung, revealing the distinctive pathologic finding.
Histopathological Findings: Pulmonary alveolar proteinosis
{{#ev:youtube|L9fVRzcPkEQ}}
Medical Therapy
The use of GM-CSF injections has also been attempted, with variable success.
Surgery
The standard treatment for PAP is whole-lung lavage, in which sterile fluid is instilled into the lung and then removed, along with the abnormal surfactant material. This is generally effective at ameliorating symptoms, often for prolonged periods. Lung transplantation can be performed in refractory cases.
References
- ↑ Rosen SH, Castleman B, and Liebow AA. Pulmonary alveolar proteinosis. New England Journal of Medicine 1958; 258: 1123-1142.
- ↑ Seymour JF and Presneill JJ. Pulmonary alveolar proteinosis: progress in the first 44 years. American Journal of Respiratory and Critical Care Medicine 2002; 166: 215-235.
- ↑ Shah PL, Hansell D, Lawson PR, et al. Pulmonary alveolar proteinosis; clinical aspects and current concepts on pathogenesis. Thorax 2000; 55: 67-77.
- ↑ Stanley E, Lieschke GJ, Grail D, et al. Granulocyte/macrophage colony-stimulating factor-deficient mice show no major perturbation of hematopoiesis but develop a characteristic pulmonary pathology. Proc. Natl. Acad. Sci. USA 1994; 91: 5592-5596.
- ↑ Uchida K, Beck D, Yamamoto T, Berclaz P, Abe S, Staudt M, Carey B, Filippi M, Wert S, Denson L, Puchalski J, Hauck D, Trapnell B (2007). "GM-CSF autoantibodies and neutrophil dysfunction in pulmonary alveolar proteinosis". N Engl J Med. 356 (6): 567–79. PMID 17287477.
- ↑ 6.0 6.1 Trapnell BC, Whitsett JA, Nakata K (2003). "Pulmonary alveolar proteinosis". N Engl J Med. 349 (26): 2527–39. doi:10.1056/NEJMra023226. PMID 14695413.