Primary ciliary dyskinesia
| Primary ciliary dyskinesia | |
 | |
|---|---|
| ICD-10 | Q89.3 |
| ICD-9 | 759.3 |
| OMIM | 244400 242650 |
| DiseasesDB | 7111 Template:DiseasesDB2 |
| MeSH | D002925 |
|
Primary ciliary dyskinesia Microchapters |
|
Differentiating Primary ciliary dyskinesia from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Primary ciliary dyskinesia On the Web |
|
American Roentgen Ray Society Images of Primary ciliary dyskinesia |
|
Risk calculators and risk factors for Primary ciliary dyskinesia |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Synonyms and keywords: PCD; immotile ciliary syndrome; Kartagener Syndrome; ciliary motility disorder; immotile cilia; ciliary dyskinesia
Overview
Historical Perspective
In 1981, Rossman and coworkers came up with the primary ciliary dyskinesia PCD.
Classification
There is no established system for the classification of primary ciliary dyskinesia.
Pathophysiology
In many people with primary ciliary dyskinesia, the cause of the disease is unknown, but the main factor contributing to the pathogenesis is mutations in the proteins forming the cilia which result in the formation of abnormal or immotile cilia. Clearly, cilia have many important functions within the body, defects in these cell structures cause a variety of signs and symptoms.
Causes
There are no established causes for Primary ciliary dyskinesia.PCD is related to defects in mucociliary clearance due to abnormal ciliary structure. Mutations in around 46 different genes throughout the genome have been found to be causative. Some of these include DNAH5, CCDC39, DNAI1, CCDC40, DNAH11, ZMYND10, CCDC103, CCDC151 and ARMC4.
Differentiating Primary ciliary dyskinesia from other Diseases
Primary ciliary dyskinesia must be differentiated from other conditions that cause infertility, sinusitis, otitis media, and rhinitis.
Epidemiology and Demographics
Primary ciliary dyskinesia (PCD) is generally documented as etiology of bronchiectasis not only in children or young adults but also in older patients. It is challenging to demonstrate the prevalence of PCD in diverse population with estimates varying between one in 4000 to one in 40,000. PCD is linked with the high levels of consanguinity. Clinical suspicion of PCD is high in these communities, chronic cough and nasal symptoms should rise concern for prompt diagnostic testing.
Risk Factors
There are no established risk factors for primary ciliary dyskinesia.
Natural History, Complications and Prognosis
The long-term effects of primary ciliary dyskinesia (PCD) are dependent on respiratory symptoms. PCD is not considered to be life-threatening, but persistent lung and airway disease can lead to permanent damage. Recurrent ear infections can lead to hearing loss, which is sometimes permanent, prompt diagnosis and early treatment improve long-term outcomes.
Diagnosis
- A high level of suspicion is required to warrant early diagnosis and initiation of appropriate management before irreversible lung damage ensues. Diagnostic investigations are complex, requiring expensive arrangements and an experienced team of clinicians and scientists. People with persistent respiratory symptoms such as rhinitis, rhino-sinusitis, infertility, recurrent otitis media should seek medical care and undergo further testing. Nasal nitric oxide levels are low in PCD and should be performed as a screening test. Transmission electron microscopy to assess the ultrastructure of cilia is another important investigation that can confirm the diagnosis.
- Patients with primary ciliary dyskinesia may present in early infancy with respiratory distress or later in life with chronic bronchitis, persistent rhinorrhea, sinusitis, bronchiectasis, or male infertility.
Primary ciliary dyskinesia has no characteristic physical examination findings, however, any clue to recurrent sinus infections or respiratory distress should raise concern for diagnosing primary ciliary dyskinesia.
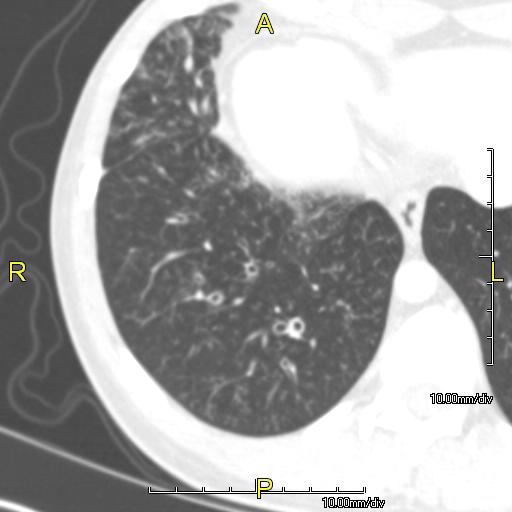
Laboratory Findings | Electrocardiogram | X-Ray Findings | Echocardiography and Ultrasound | CT-Scan Findings | MRI Findings | Other Imaging Findings | Other Diagnostic Studies
Treatment
There are no definite treatment options, the goal is to manage associated conditions that can lead to worsening of PCD.
There are no established measures for interventions of Primary ciliary dyskinesia.
There are no established surgical indications for primary ciliary dyskinesia.
There are no established measures for the primary prevention of primary ciliary dyskinesia.
There are no established measures for the secondary prevention of primary ciliary dyskinesia.
| Cost-Effectiveness of Therapy | Future or Investigational Therapies
Case Studies