Polyarteritis nodosa
For patient information, click here Template:DiseaseDisorder infobox Template:Search infobox
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Haritha Machavarapu, M.B.B.S.
Synonyms and keywords: PAN; Kussmaul disease; Kussmaul-Meier disease; periarteritis nodosa
For the heart in Polyarteritis Nodosa click here
Overview
Polyarteritis nodosa is a vasculitis of medium-sized arteries, which become swollen and damaged from attack by rogue immune cells.
Historical Perspective
Polyarteritis nodosa is also called Kussmaul disease or Kussmaul-Meier disease[1] after Kussumaul and Maier, who first described the syndrome in 1866.
Pathophysiology
Polyarteritis nodosa is a disease of unknown cause that affects arteries, the blood vessels that carry oxygenated blood to organs and tissues. It occurs when certain immune cells attack the affected arteries.Inflammation starts in the vessel intima and results in fibrinoid necrosis by destroying the internal and external elastic lamina. Aneurysms and thrombi may develop at the site of lesions. One hypothesis is that this condition is caused by antibodies against HBV, via a type IIII hypersensitivity reaction. Hepatitis C associated polyarteritis nodosa is the most common type among the hepatitis C associated vasculitis and has a severe clinical presentation.[2]
Causes
Polyarteritis nodosa is a disease of unknown cause that affects arteries, the blood vessels that carry oxygenated blood to organs and tissues. It occurs when certain immune cells attack the affected arteries.More adults than children get this disease. It damages the tissues supplied by the affected arteries because the tissues aren't receiving the oxygen and nourishment they need. People with active hepatitis B and hepatitis C may develop this disease.
Epidemiology and Demographics
The condition affects adults more frequently than children. It damages the tissues supplied by the affected arteries because they don't receive enough oxygen and nourishment without a proper blood supply. Polyarteritis nodosa is more common in people with hepatitis B infection.
Natural History, Prognosis, and Complications
Therapy results in remissions or cures in 90% of cases. Untreated, the disease is fatal in most cases. The most serious associated conditions generally involve the kidneys and gastrointestinal tract. Without treatment, the outlook is poor. Guillevin and coworkers have described five prognostic factors that predict high probability of mortality and are considered indications for another immunosuppressive drug in addition to prednisone.
- Proteinuria >1g/day
- Azotemia
- Cardiomyopathy
- Gastrointestinal involvement
- Central nervous system disease
With none of these factors, 5-year mortality is 12%. With 2 or more 5-year mortality is 46%[3]
Complications include the following:
- Stroke
- Kidney failure
- Heart attack
- Intestinal necrosis and perforation
Diagnosis
Symptoms
- Fatigue
- Weakness
- Fever
- Abdominal pain
- Decreased appetite
- Unintentional weight loss
- Muscle aches
- Joint aches
- Skin ulcers
In this disease, symptoms result from damage to affected organs, often the skin, heart, kidneys, and nervous system.
Generalized symptoms include fever, fatigue, weakness, loss of appetite, and weight loss. Muscle and joint aches are common. Cutaneous polyarteritis nodosa most frequently manifests as nodules in the lower legs. They may not leave any residual changes but sometimes livedo reticularis is observed. Ulcerations and splinter hemorrhages are the frequent complications.[4]
Nerve involvement may cause sensory changes with numbness, pain, burning, and weakness.Frequently affected nerves are peroneal, median, ulnar and sural nerves. Central nervous system polyarteritis nodosa presents in three major forms : diffuse encepalopathy,focal neurological deficits and seizures. Diffuse encepahalopathy is characterised by loss of intellectual capacity, disorientation and occasionally psychosis with visual hallucinations.Cerebrovascular accidents in cerebrum, cerebellum or brain stem cause focal defecits.[5]. Kidney involvement can produce varying degrees of renal failure.Arteritis in the renal circulation leads to hypertension.Sometimes patients present with severe flank pain because of renal infarction or rupture of intrarenal aneurysm.
Involvement of the arteries of the heart may cause a heart attack, heart failure, and inflammation of the sac around the heart (pericarditis).
Vasculitis of testicular vessels can cause testicular infarction, manifesting as testicular pain or tenderness.[6].
Abdominal pain,weight loss, food avoidance, gastrointestinal bleeding, peritonitis are seen in mesentric vasculitis.[7]
Laboratory Findings
There are no specific lab tests for diagnosing polyarteritis nodosa. Diagnosis is generally based upon the physical examination and a few laboratory studies that help to confirm the diagnosis:
- CBC (may demonstrate an elevated white blood count)
- ESR (often elevated)
- Perinuclear pattern of antineutrophil cytoplasmic antibodies (p-ANCA) - not associated with "classic" polyarteritis nodosa, but is present in a form of the disease affecting smaller blood vessels, known as microscopic polyangiitis or leukocytoclastic angiitis.
- Tissue biopsy (reveals inflammation in small arteries, called arteritis)
- Elevated c reactive protein
- EMG and nerve conduction studies can be done in cases of nerve involvement and help in nerve biopsy.[8]
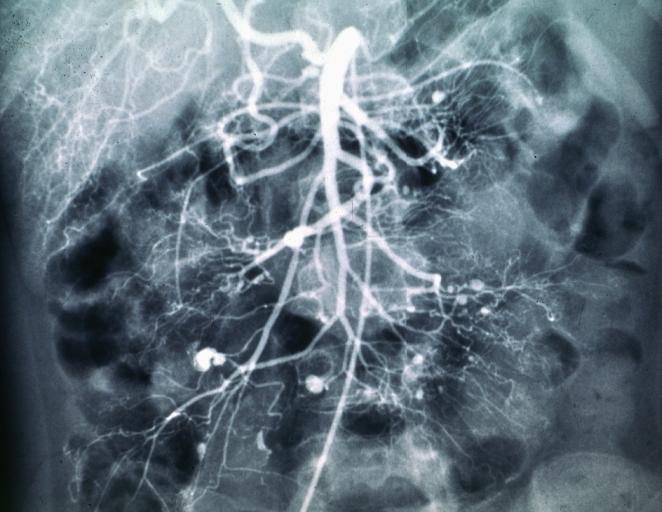
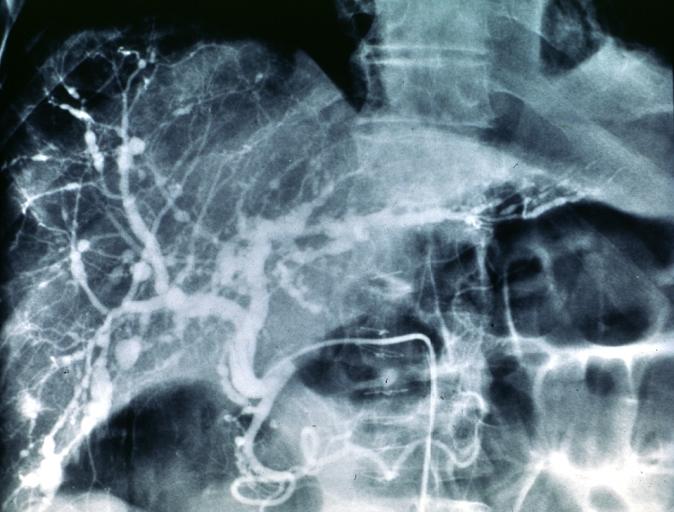
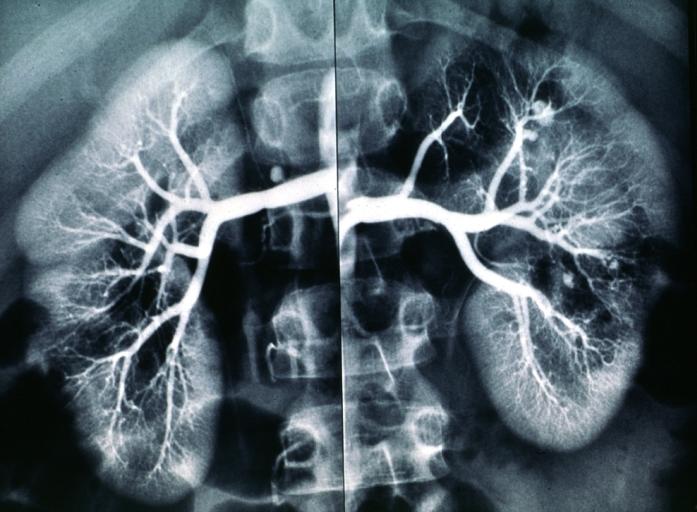
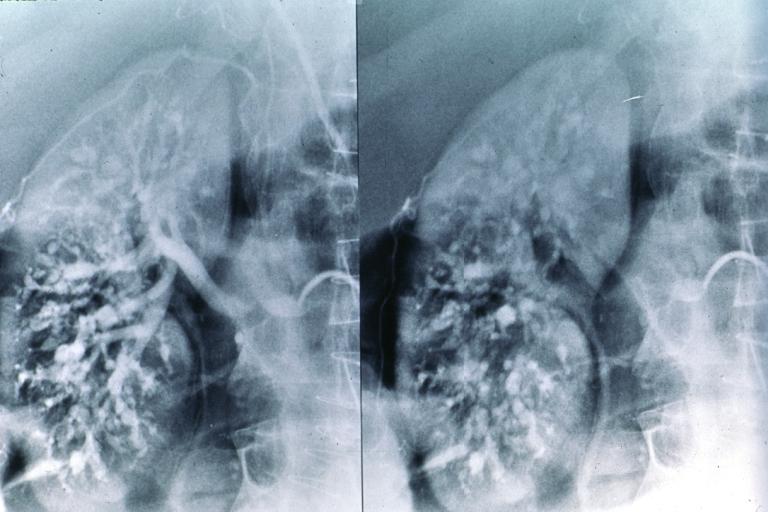
- Angiography and arteriograms help in identifying aneurysms in mesentry.[9]
- CT and MRI of abdomen in GI involvement.
- MRI in CNS involvement helps in identifying hemorrhage and ischemia.
Diagnostic Criteria
A patient is said to have polyarteritis nodosa if he or she has 3 of the 10 following signs:
- Weight loss ≥4 kg.
- Livedo reticularis (a mottled purplish skin discoloration over the extremities or torso).
- Testicular pain or tenderness. (occasionally, a site biopsied for diagnosis).
- Muscle pain, weakness, or leg tenderness.
- Nerve disease (either single or multiple).
- Diastolic blood pressure greater than 90mmHg (high blood pressure).
- Elevated kidney blood tests (BUN greater than 40 mg/dl or creatinine greater than 1.5 mg/dl).
- Hepatitis B virus tests positive (for surface antigen or antibody).
- Arteriogram (angiogram) showing the arteries that are dilated (aneurysms) or constricted by the blood vessel inflammation.
- Biopsy of tissue showing the arteritis (typically inflamed arteries).[10]
Diagnostic x-ray images
Treatment
Treatment involves medications to suppress the immune system such as prednisone and cyclophosphamide. Addition of immunosuppressants like cyclophosphamide, methotrexate, azathioprine to corticosteroid therapy has better prognosis.[11]. Patients with hepatitis B associated polyarteritis nodosa are treated with corticosteroid therapy, antiviral agents and plasma exchanges.[12].[13]. Unlike hepatitis b associated PAN, Hepatitis C associated PAN is treated with Rituximab and corticosteoid therapy without antiviral agents, emphasizing the B cell targeted therapy.[14]
Mild cases of cutaneous polyarteritis nodosa are treated with nonsteroidal anti-inflammatory drugs[15]. Severe cases are treated with corticosteroid and adjunctive therapy. Antibiotics are added to the treatment of patients with antecedent streptococcal infections or high ASO titer.[4].
Intravenous immunoglobulin is suggested for treatment of corticosteroid therapy resistant cases, but the effect is transient.[16][17].It is also used in the treatment of Parvovirus B19 associated polyarteritis nodosa.[18]
References
- ↑ Template:WhoNamedIt
- ↑ Saadoun D, Terrier B, Semoun O; et al. (2011). "Hepatitis C virus-associated polyarteritis nodosa". Arthritis Care Res (Hoboken). 63 (3): 427–35. doi:10.1002/acr.20381. PMID 20981809. Unknown parameter
|month=ignored (help) - ↑ Kelley's Textbook of Rheumatology,8th edition
- ↑ 4.0 4.1 Díaz-Pérez JL, De Lagrán ZM, Díaz-Ramón JL, Winkelmann RK (2007). "Cutaneous polyarteritis nodosa". Semin Cutan Med Surg. 26 (2): 77–86. doi:10.1016/j.sder.2007.02.003. PMID 17544958. Unknown parameter
|month=ignored (help) - ↑ Rosenberg MR, Parshley M, Gibson S, Wernick R (1990). "Central nervous system polyarteritis nodosa". West. J. Med. 153 (5): 553–6. PMC 1002622. PMID 1979706. Unknown parameter
|month=ignored (help) - ↑ Meeuwissen J, Maertens J, Verbeken E, Blockmans D (2008). "Case reports: testicular pain as a manifestation of polyarteritis nodosa". Clin. Rheumatol. 27 (11): 1463–6. doi:10.1007/s10067-008-0970-5. PMID 18651100. Unknown parameter
|month=ignored (help) - ↑ Guillevin L, Lhote F, Gallais V; et al. (1995). "Gastrointestinal tract involvement in polyarteritis nodosa and Churg-Strauss syndrome". Ann Med Interne (Paris). 146 (4): 260–7. PMID 7653948.
- ↑ Lacomis D, Zivković SA (2007). "Approach to vasculitic neuropathies". J Clin Neuromuscul Dis. 9 (1): 265–76. doi:10.1097/CND.0b013e31815202b3. PMID 17989592. Unknown parameter
|month=ignored (help) - ↑ Hughes LB, Bridges SL (2002). "Polyarteritis nodosa and microscopic polyangiitis: etiologic and diagnostic considerations". Curr Rheumatol Rep. 4 (1): 75–82. PMID 11798986. Unknown parameter
|month=ignored (help) - ↑ Shiel, Jr., William C, http://www.medicinenet.com/polyarteritis_nodosa/article.htm
- ↑ Leib ES, Restivo C, Paulus HE (1979). "Immunosuppressive and corticosteroid therapy of polyarteritis nodosa". Am. J. Med. 67 (6): 941–7. PMID 42314. Unknown parameter
|month=ignored (help) - ↑ Mouthon L (1999). "[Periarteritis nodosa induced by hepatitis B virus]". Pathol. Biol. (in French). 47 (3): 237–44. PMID 10214615. Unknown parameter
|month=ignored (help) - ↑ Trepo C, Guillevin L (2001). "Polyarteritis nodosa and extrahepatic manifestations of HBV infection: the case against autoimmune intervention in pathogenesis". J. Autoimmun. 16 (3): 269–74. doi:10.1006/jaut.2000.0502. PMID 11334492. Unknown parameter
|month=ignored (help) - ↑ Néel A, Masseau A, Hervier B; et al. (2011). "Life-threatening hepatitis C virus-associated polyarteritis nodosa successfully treated by rituximab". J Clin Rheumatol. 17 (8): 439–41. doi:10.1097/RHU.0b013e31823a58d7. PMID 22089995. Unknown parameter
|month=ignored (help) - ↑ Morgan AJ, Schwartz RA (2010). "Cutaneous polyarteritis nodosa: a comprehensive review". Int. J. Dermatol. 49 (7): 750–6. doi:10.1111/j.1365-4632.2010.04522.x. PMID 20618492. Unknown parameter
|month=ignored (help) - ↑ Kroiss M, Hohenleutner U, Gruss C, Glaessl A, Landthaler M, Stolz W (2001). "Transient and partial effect of high-dose intravenous immunoglobulin in polyarteritis nodosa". Dermatology (Basel). 203 (2): 188–9. PMID 11586025.
- ↑ Balbir-Gurman A, Nahir AM, Braun-Moscovici Y (2007). "Intravenous immunoglobulins in polyarteritis nodosa restricted to the limbs: case reports and review of the literature". Clin. Exp. Rheumatol. 25 (1 Suppl 44): S28–30. PMID 17428360.
- ↑ Viguier M, Guillevin L, Laroche L (2001). "Treatment of parvovirus B19-associated polyarteritis nodosa with intravenous immune globulin". N. Engl. J. Med. 344 (19): 1481–2. doi:10.1056/NEJM200105103441919. PMID 11357850. Unknown parameter
|month=ignored (help)
de:Polyarteriitis nodosa nl:Polyarteritis nodosa sv:Polyarteritis nodosa