Pheochromocytoma pathophysiology
|
Pheochromocytoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Pheochromocytoma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Pheochromocytoma pathophysiology |
|
Risk calculators and risk factors for Pheochromocytoma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ahmad Al Maradni, M.D. [2]
Overview
Pheochromocytoma arise from chromaffin cells of the adrenal medulla.On gross pathology, pheochromocytoma has a multinodular and a multicentric pattern of growth. On microscopic histopathological analysis, nesting (Zellballen) pattern composed of well-defined clusters of tumor cells separated by fibrovascular stroma is a characteristic finding.it may be benign or malignant, familial origin(multiple endocrine neoplasia type 2) or sporadic one. Both of them have genetic origin depends on large number of genes: VHL, SDH, NF1, RET.
Pathophysiology
Pheochromocytoma arise from chromaffin cells of the adrenal medulla and sympathetic ganglia. Traditionally pheochromocytoma known as the "10% tumor":
- Approximately 10% of patients have bilateral disease
- Approximately 10% of tumors are malignant
- Approximately 10% are located in chromaffin tissue outside of the adrenal gland, The most common extradrenal locations are the abdomen and thorax .
- Approximately 10% occur in childhood
- Approximately 10% are familial
- Approximately 10% recur after being resected
- Approximately 10% of patients do not have hypertension
Malignant and benign pheochromocytomas are the same; The only difference is the ability to spread locally and distant. [1]
Genetics
Pheochromocytomas can be familial and occur in patients with multiple endocrine neoplasia (MEN 2 and MEN 3). Patients with Von Hippel Lindau (VHL) may also develop pheocromocytoma.[2] It is autosomal dominant inheritance and has two pathways of tumor pathogenesis. Cluster 1 tumorsare noradrenergic. Cluster 2 tumors are adrenergic.[3]
| Cluster 1 | Cluster 2 |
|---|---|
| •Succinate dehydrogenase (SDH) subunit genes
•von Hippel-Lindau (VHL) disease •Fumarate hydratase gene mutations |
•Multiple endocrine neoplasia type 2A
•Multiple endocrine neoplasia type 2B •Neurofibromatosis type 1 (NF1) |
Associated conditions
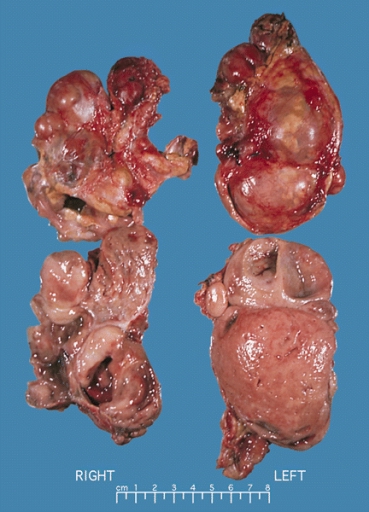
Gross Pathology
On gross pathology, A multinodular and multicentric pattern of growth of pheochromocytoma may be seen.
-
Bilateral pheochromocytoma in MEN2. Gross image.
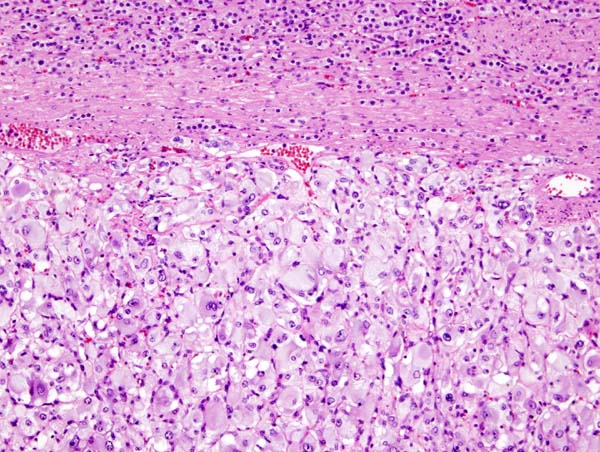
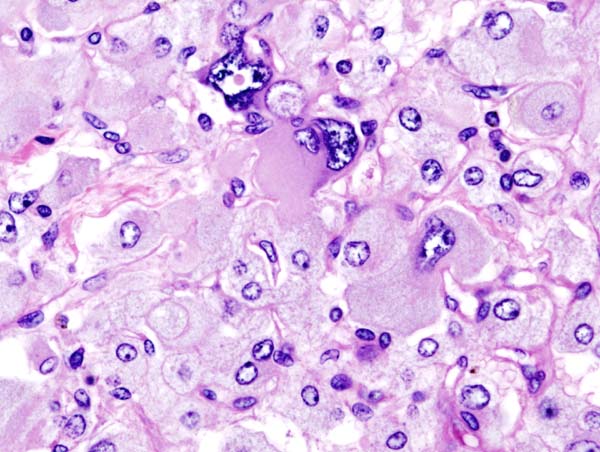
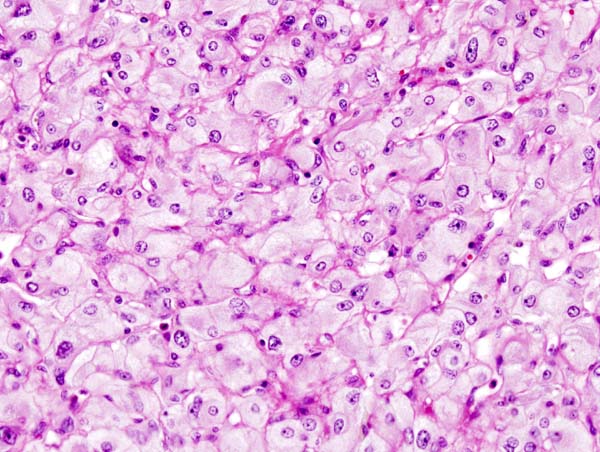
Microscopic Pathology
On microscopic pathology, Pheochromocytoma typically demonstrates a nesting (Zellballen) pattern on microscopy. This pattern is composed of well-defined clusters of tumor cells containing eosinophilic cytoplasm separated by fibrovascular stroma.
-
Micrograph of pheochromocytoma.
-
Histopathology of adrenal pheochromocytoma. Adrenectomy specimen.
-
Micrograph of pheochromocytoma.
-
Micrograph of pheochromocytoma.
Videos
{{#ev:youtube|7yjxG3KmX98}}
References
- ↑ Goldstein RE, O'Neill JA, Holcomb GW, Morgan WM, Neblett WW, Oates JA; et al. (1999). "Clinical experience over 48 years with pheochromocytoma". Ann Surg. 229 (6): 755–64, discussion 764-6. PMC 1420821. PMID 10363888.
- ↑ Shuch B, Ricketts CJ, Metwalli AR, Pacak K, Linehan WM (2014). "The genetic basis of pheochromocytoma and paraganglioma: implications for management". Urology. 83 (6): 1225–32. doi:10.1016/j.urology.2014.01.007. PMC 4572836. PMID 24642075.
- ↑ King KS, Pacak K (2014). "Familial pheochromocytomas and paragangliomas". Mol Cell Endocrinol. 386 (1–2): 92–100. doi:10.1016/j.mce.2013.07.032. PMC 3917973. PMID 23933153.