Pheochromocytoma CT: Difference between revisions
(→CT) |
(→CT) |
||
| Line 10: | Line 10: | ||
==CT== | ==CT== | ||
[[Computed tomography]]: Radiological evaluation should follow lab tests to locate site of the tumour.<ref name="pmid1787652">{{cite journal| author=Bravo EL| title=Pheochromocytoma: new concepts and future trends. | journal=Kidney Int | year= 1991 | volume= 40 | issue= 3 | pages= 544-56 | pmid=1787652 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1787652 }} </ref> | [[Computed tomography]]: Radiological evaluation should follow lab tests to locate site of the tumour.<ref name="pmid1787652">{{cite journal| author=Bravo EL| title=Pheochromocytoma: new concepts and future trends. | journal=Kidney Int | year= 1991 | volume= 40 | issue= 3 | pages= 544-56 | pmid=1787652 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1787652 }} </ref> | ||
Most common extraadrenal locations are superior and inferior abdominal paraaortic areas,the urinary bladder,thorax,head,neck and pelvis.<ref name="pmid1729490">{{cite journal| author=Whalen RK, Althausen AF, Daniels GH| title=Extra-adrenal pheochromocytoma. | journal=J Urol | year= 1992 | volume= 147 | issue= 1 | pages= 1-10 | pmid=1729490 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1729490 }} </ref> | |||
In sporadic pheochromocytoma, CT and MRI are good choices.Choosing depends on availability and cost.<ref name="pmid191248172">{{cite journal| author=Baid SK, Lai EW, Wesley RA, Ling A, Timmers HJ, Adams KT et al.| title=Brief communication: radiographic contrast infusion and catecholamine release in patients with pheochromocytoma. | journal=Ann Intern Med | year= 2009 | volume= 150 | issue= 1 | pages= 27-32 | pmid=19124817 | doi= | pmc=3490128 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19124817 }}</ref> | |||
In sporadic pheochromocytoma, | |||
●Familial pheochromocytoma – In patients with the multiple endocrine neoplasia type 2 (MEN2) syndrome, computing imaging may miss about one-quarter of the tumors [23]. In a selected group of patients with a 40 percent incidence of pheochromocytoma, the respective positive and negative predictive values of CT were 69 and 98 percent [6]. | ●Familial pheochromocytoma – In patients with the multiple endocrine neoplasia type 2 (MEN2) syndrome, computing imaging may miss about one-quarter of the tumors [23]. In a selected group of patients with a 40 percent incidence of pheochromocytoma, the respective positive and negative predictive values of CT were 69 and 98 percent [6]. | ||
Revision as of 15:25, 3 July 2017
|
Pheochromocytoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Pheochromocytoma CT On the Web |
|
American Roentgen Ray Society Images of Pheochromocytoma CT |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ahmad Al Maradni, M.D. [2]
Please help WikiDoc by adding content here. It's easy! Click here to learn about editing.
Overview
Head, neck, chest, and abdominal CT scans may be helpful in the diagnosis of pheochromocytoma.
CT
Computed tomography: Radiological evaluation should follow lab tests to locate site of the tumour.[1]
Most common extraadrenal locations are superior and inferior abdominal paraaortic areas,the urinary bladder,thorax,head,neck and pelvis.[2]
In sporadic pheochromocytoma, CT and MRI are good choices.Choosing depends on availability and cost.[3]
●Familial pheochromocytoma – In patients with the multiple endocrine neoplasia type 2 (MEN2) syndrome, computing imaging may miss about one-quarter of the tumors [23]. In a selected group of patients with a 40 percent incidence of pheochromocytoma, the respective positive and negative predictive values of CT were 69 and 98 percent [6].
●Imaging phenotype of pheochromocytoma/paragangliomas
•Increased attenuation on nonenhanced CT (>20 Hounsfield units)
•Increased mass vascularity
•Delay in contrast medium washout (10 minutes after administration of contrast, an absolute contrast medium washout of less than 50 percent)
•High signal intensity on T2-weighted MRI
•Cystic and hemorrhagic changes
•Variable size and may be bilateral
Additional imaging
MIBG
●If abdominal and pelvic CT or MRI is negative in the presence of clinical and biochemical evidence of pheochromocytoma, one ought first to reconsider the diagnosis. If it is still considered likely, then iodine-123 (123-I) metaiodobenzylguanidine (MIBG) scintigraphy may be done. MIBG is a compound resembling norepinephrine that is taken up by adrenergic tissue. A MIBG scan can detect tumors not detected by CT or MRI or multiple tumors when CT or MRI is positive [6].
●MIBG scintigraphy is superfluous in patients with sporadic solitary adrenal pheochromocytoma identified on CT/MRI [57].
●MIBG scintigraphy is indicated in patients with large (eg, >10 cm) adrenal pheochromocytomas (increased risk of malignancy) or paraganglioma (increased risk of multiple tumors and malignancy) (image 2) [25].
●Surgery is never indicated based on MIBG findings alone; MIBG findings should always be corroborated by findings on computed imaging. Normal adrenal glands take up MIBG, and the uptake may be asymmetric.
FDG-PET — Fludeoxyglucose-positron emission tomography (FDG-PET) is more sensitive than 123-I MIBG and CT/MRI for detection of metastatic disease (image 3) [58-62]. The utility of integrated FDG-PET/CT imaging as compared with 123-I MIBG and conventional cross-sectional imaging with CT or MRI was directly addressed in a prospective study of 216 patients with suspected pheochromocytoma/paraganglioma, 60 of whom had nonmetastatic pheochromocytoma/paraganglioma, 95 of whom had metastatic pheochromocytoma/paraganglioma, and 61 of whom did not have pheochromocytoma/paraganglioma [59]. For the primary tumor, the sensitivity of PET/CT for nonmetastatic tumors was similar to that of 123-I MIBG but less than that of CT/MRI(77, 75, and 96 percent, respectively). Among the patients who had paraganglioma/pheochromocytoma ruled out, specificity was comparable (90, 92, and 90 percent, respectively). When the analysis was limited to 26 paragangliomas of the head and neck, PET/CT was more sensitive than 123-I MIBG (85 versus 52 percent).
Other
●111-In-pentetreotide scintigraphy (OctreoScan) or total body MRI are other imaging options. 111-In-pentetreotide will rarely detect a tumor in an unusual location (eg, the heart) when the other techniques have failed [63].
●Several positron-emitting radiolabeled somatostatin analogs have emerged (such as gallium 68 [(68)Ga] 1,4,7,10-tetraazacyclododecane-1,4,7,10-tetraacetic acid [DOTA]-octreotate [DOTATATE]) that, in combination with high-resolution PET integrated with CT, may eventually improve the detection and staging of a variety of neuroendocrine tumors, including paraganglioma. These novel PET modalities offer higher spatial resolution than conventional 111-In pentetreotide and are associated with improved sensitivity for detection of small lesions. A kit for preparation of 68-Ga DOTATATE injection as a radioactive diagnostic agent for PET imaging (Netspot) was approved by the US Food and Drug Administration (FDA) in June 2016. (See "Paragangliomas: Epidemiology, clinical presentation, diagnosis, and histology", section on 'Radioisotope imaging'.)
●Selective adrenal venous sampling (AVS) may result in inappropriate adrenalectomy. When AVS for catecholamines was performed in 18 patients without pheochromocytoma, epinephrine and norepinephrine concentrations were significantly higher in the right versus the left adrenal vein (up to 83-fold difference for epinephrine) [64]. These data highlight why AVS should not be used in the investigation of adrenal pheochromocytoma.
●In addition, image-guided needle biopsy of suspected pheochromocytoma or paraganglioma should be avoided due to a high rate of biopsy-related complications. This was illustrated in a report of 20 patients who were diagnosed at the time of needle biopsy, of whom 14 (70 percent) developed a biopsy-related complication [65]. Complications included: increased difficulty of the definitive operation in 7 of 17 (41 percent) operative cases, with one patient requiring conversion to an open procedure; severe hypertension (15 percent); hematoma (30 percent); incorrect or inadequate biopsy (25 percent); severe pain (25 percent); and delay in surgical treatment (15 percent) [65].
-
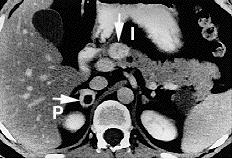
Pheochromocytoma. CT abdomen.
-
Pheochromocytoma. CT abdomen.
References
- ↑ Bravo EL (1991). "Pheochromocytoma: new concepts and future trends". Kidney Int. 40 (3): 544–56. PMID 1787652.
- ↑ Whalen RK, Althausen AF, Daniels GH (1992). "Extra-adrenal pheochromocytoma". J Urol. 147 (1): 1–10. PMID 1729490.
- ↑ Baid SK, Lai EW, Wesley RA, Ling A, Timmers HJ, Adams KT; et al. (2009). "Brief communication: radiographic contrast infusion and catecholamine release in patients with pheochromocytoma". Ann Intern Med. 150 (1): 27–32. PMC 3490128. PMID 19124817.