|
|
| (17 intermediate revisions by 3 users not shown) |
| Line 4: |
Line 4: |
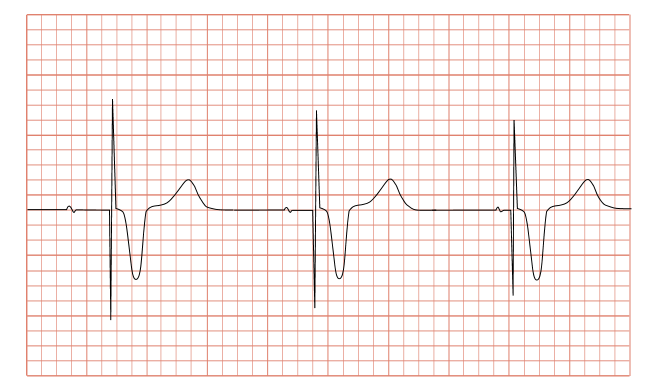
| | Image = Pacemaker_syndrome1.png | | | Image = Pacemaker_syndrome1.png |
| }} | | }} |
| {{SI}} | | {{Pacemaker syndrome}} |
| {{CMG}}; {{AE}} {{RT}} | | {{CMG}}; {{AE}} {{RT}} {{MIR}} [[User:Tayebah Chaudhry|Tayebah Chaudhry]][mailto:dr.thch@yahoo.com] |
|
| |
|
| ==Overview== | | ==[[Pacemaker syndrome overview|Overview]]== |
| Pacemaker syndrome is a disease that represents the clinical consequences of suboptimal [[Atrioventricular node|atrioventricular]] (AV) synchrony or AV dyssynchrony, regardless of the pacing mode, after the [[Artificial pacemaker#Insertion|pacemaker plantation]].<ref name="pmid9164889">{{cite journal |author=Ellenbogen KA, Gilligan DM, Wood MA, Morillo C, Barold SS |title=The pacemaker syndrome -- a matter of definition |journal=Am. J. Cardiol. |volume=79 |issue=9 |pages=1226–9 |year=1997 |month=May |pmid=9164889 |url=http://linkinghub.elsevier.com/retrieve/pii/S0002914997000854 |doi=10.1016/S0002-9149(97)00085-4}}</ref><ref name="pmid12555483">{{cite journal |author=Chalvidan T, Deharo JC, Djiane P |title=[Pacemaker syndromes] |language=French |journal=Ann Cardiol Angeiol (Paris) |volume=49 |issue=4 |pages=224–9 |year=2000 |month=July |pmid=12555483 }}</ref>. It is an [[iatrogenic]] disease that is often underdiagnosed<ref name="pmid9164889">{{cite journal |author=Ellenbogen KA, Gilligan DM, Wood MA, Morillo C, Barold SS |title=The pacemaker syndrome -- a matter of definition |journal=Am. J. Cardiol. |volume=79 |issue=9 |pages=1226–9 |year=1997 |month=May |pmid=9164889 |doi=10.1016/S0002-9149(97)00085-4 }}</ref><ref name="isbn0-07-141652-8">{{cite book |author=Baumgartner, William A.; Yuh, David D.; Luca A. Vricella |title=The Johns Hopkins manual of cardiothoracic surgery |publisher=McGraw-Hill Medical Pub |location=New York |year=2007 |origyear= |pages= |quote= |isbn=0-07-141652-8 }}</ref>. In general, the symptoms of the [[syndrome]] are a combination of decreased [[cardiac output]], loss of [[atrial]] contribution to [[ventricle|ventricular]] filling, loss of [[total peripheral resistance]] response, and nonphysiologic pressure waves.<ref name="pmid12555483" /><ref name="pmid7821326">{{cite journal |author=Frielingsdorf J, Gerber AE, Hess OM |title=Importance of maintained atrio-ventricular synchrony in patients with pacemakers |journal=Eur. Heart J. |volume=15 |issue=10 |pages=1431–40 |year=1994 |month=October |pmid=7821326 |url=http://eurheartj.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=7821326}}</ref><ref name="pmid7511223">{{cite journal |author=Furman S |title=Pacemaker syndrome |journal=Pacing Clin Electrophysiol |volume=17 |issue=1 |pages=1–5 |year=1994 |month=January |pmid=7511223 |doi=10.1111/j.1540-8159.1994.tb01342.x }}</ref>
| |
|
| |
|
| Individuals with a low heart rate prior to [[pacemaker]] implantation are more at risk of developing pacemaker syndrome. Normally the first chamber of the heart ([[atrium]]) contracts as the second chamber (ventricle) is relaxed, allowing the ventricle to fill before it contracts and pumps blood out of the heart. When the timing between the two chambers goes out of synchronization, less [[blood]] is delivered on each beat. Patients who develop pacemaker syndrome may require adjustment of the pacemaker timing, or another lead fitted to regulate the timing of the chambers separately.
| | ==[[Pacemaker syndrome historical perspective|Historical Perspective]]== |
|
| |
|
| ==Historical Perspective== | | ==[[Pacemaker syndrome pathophysiology|Pathophysiology]]== |
| Pacemaker syndrome was first described in 1969 by Mitsui et al. as a collection of symptoms associated with right ventricular pacing.<ref name="pmid1389730">{{cite journal |author=Travill CM, Sutton R |title=Pacemaker syndrome: an iatrogenic condition |journal=[[British Heart Journal]] |volume=68 |issue=2 |pages=163–6 |year=1992 |month=August |pmid=1389730 |pmc=1025005 |doi= 10.1136/hrt.68.8.163|url=http://heart.bmj.com/cgi/pmidlookup?view=long&pmid=1389730 |issn= |accessdate=2009-06-19}}</ref><ref>Mitsui T, Hori M, Suma K, et al. The "pacemaking syndrome." In: Jacobs JE, ed. Proceedings of the 8th Annual International Conference on Medical and Biological Engineering. Chicago, IL: Association for the Advancement of Medical Instrumentation;. 1969;29-3.</ref> The name pacemaker syndrome was first coined by Erbel in 1979.<ref name="pmid1389730" /><ref>2 Erbel R. Pacemaker syndrome. AmJ Cardiol 1979;44:771-2.</ref> Since its first discovery, there have been many definitions of pacemaker syndrome, and the understanding of the cause of pacemaker syndrome is still under investigation. In a general sense, pacemaker syndrome can be defined as the symptoms associated with right ventricular pacing relieved with the return of A-V and V-V synchrony.
| |
|
| |
|
| ==Pathophysiology== | | ==[[Pacemaker syndrome differential diagnosis|Differentiating Pacemaker syndrome from other Diseases]]== |
| The loss of [[physiology|physiologic]] timing of [[atrium (heart)|atrial]] and [[ventricle (heart)|ventricular]] contractions, or sometimes called AV dyssynchrony, leads to different mechanisms of [[symptom]]s production. This altered ventricular contraction will decrease [[cardiac output]], and in turn will lead to systemic hypotensive reflex response with varying symptoms.<ref name="pmid9164889">{{cite journal |author=Ellenbogen KA, Gilligan DM, Wood MA, Morillo C, Barold SS |title=The pacemaker syndrome—a matter of definition |journal=Am. J. Cardiol. |volume=79 |issue=9 |pages=1226–9 |year=1997 |month=May |pmid=9164889 |doi= 10.1016/S0002-9149(97)00085-4|url=http://linkinghub.elsevier.com/retrieve/pii/S0002914997000854}}</ref><ref name="pmid12555483" /><ref name="pmid7821326"/><ref name="pmid7511223"/>
| |
|
| |
|
| ===Loss of Atrial Contraction=== | | ==[[Pacemaker syndrome epidemiology and demographics|Epidemiology and Demographics]]== |
| Inappropriate pacing in patients with decreased [[ventricle (heart)|ventricular]] compliance, which may be caused by diseases such as [[hypertensive heart disease|hypertensive cardiomyopathy]], [[hypertrophic cardiomyopathy]], [[restrictive cardiomyopathy]], and [[aging]], can result in loss of [[atrium (heart)|atrial]] contraction and significantly reduces [[cardiac output]]. Because in such cases the atrias are required to provide 50% of [[cardiac output]], which normally provides only 15% - 25% of [[cardiac output]].<ref name="pmid1413181">{{cite journal |author=Petersen HH, Videbaek J |title=[The pacemaker syndrome] |language=Danish |journal=Ugeskr. Laeg. |volume=154 |issue=38 |pages=2547–51 |year=1992 |month=September |pmid=1413181 |doi= |url=}}</ref><ref name="pmid1442632">{{cite journal |author=Gross JN, Keltz TN, Cooper JA, Breitbart S, Furman S |title=Profound "pacemaker syndrome" in hypertrophic cardiomyopathy |journal=Am. J. Cardiol. |volume=70 |issue=18 |pages=1507–11 |year=1992 |month=December |pmid=1442632 |doi= 10.1016/0002-9149(92)90313-N|url=http://linkinghub.elsevier.com/retrieve/pii/0002-9149(92)90313-N |format=}} {{dead link|date=May 2010}}</ref>
| |
|
| |
|
| ===Cannon A Waves=== | | ==[[Pacemaker syndrome risk factors|Risk Factors]]== |
| {{main|Cannon A waves}}
| |
| [[Atrium (heart)|Atrial]] contraction against a closed [[tricuspid valve]] can cause pulsation in the neck and [[abdomen]], [[headache]], [[cough]], and jaw pain.<ref name="pmid1413181" /><ref name="pmid2032410">{{cite journal |author=Schüller H, Brandt J |title=The pacemaker syndrome: old and new causes |journal=Clin Cardiol |volume=14 |issue=4 |pages=336–40 |year=1991 |month=April |pmid=2032410 |doi=10.1002/clc.4960140410 }}</ref> | |
|
| |
|
| ===Increased Atrial Pressure=== | | ==[[Pacemaker syndrome natural history, complications and prognosis|Natural History, Complications and Prognosis]]== |
| [[ventricle (heart)|Ventricular]] pacing is associated with elevated [[right atrium|right]] and [[left atrium|left atrial]] pressures, as well as elevated [[pulmonary vein|pulmonary venous]] and [[pulmonary artery|pulmonary arterial]] pressures, which can lead to [[symptom]]atic [[pulmonary edema|pulmonary]] and [[liver|hepatic]] [[wiktionary:congestion|congestion]].<ref name="pmid7511223"/>
| |
| | |
| ===Increased Production of Natriuretic Peptides===
| |
| {{main|Atrial natriuretic peptide}}
| |
| {{main|Brain natriuretic peptide}}
| |
| Patients with [[artificial pacemaker|pacemaker]] [[syndrome]] exhibit increased plasma levels of [[atrial natriuretic peptide|ANP]]. That's due to increase in [[left atrium|left atrial]] pressure and [[left ventricle|left ventricular]] filling pressure, which is due to decreased [[cardiac output]] caused by dyssynchrony in [[atrium (heart)|atrial]] and [[ventricle (heart)|ventricular]] contraction. [[atrial natriuretic peptide|ANP]] and [[brain natriuretic peptide|BNP]] are potent [[artery|arterial]] and [[vein|venous]] [[vasodilation|vasodilators]] that can override [[common carotid artery|carotid]] and [[aorta|aortic]] [[baroreflex|baroreceptor reflex]]es attempting to compensate for decreased [[blood pressure]]. Usually patients with [[cannon A waves|cannon a waves]] have higher plasma levels of [[atrial natriuretic peptide|ANP]] than those without [[cannon A waves|cannon a waves]].<ref name="pmid9164889"/><ref name="pmid9036762">{{cite journal |author=Theodorakis GN, Panou F, Markianos M, Fragakis N, Livanis EG, Kremastinos DT |title=Left atrial function and atrial natriuretic factor/cyclic guanosine monophosphate changes in DDD and VVI pacing modes |journal=Am. J. Cardiol. |volume=79 |issue=3 |pages=366–70 |year=1997 |month=February |pmid=9036762 |url=http://linkinghub.elsevier.com/retrieve/pii/S0002914997892855 |doi=10.1016/S0002-9149(97)89285-5}}</ref><ref name="pmid1334465">{{cite journal |author=Theodorakis GN, Kremastinos DT, Markianos M, Livanis E, Karavolias G, Toutouzas PK |title=Total sympathetic activity and atrial natriuretic factor levels in VVI and DDD pacing with different atrioventricular delays during daily activity and exercise |journal=Eur. Heart J. |volume=13 |issue=11 |pages=1477–81 |year=1992 |month=November |pmid=1334465 |doi= |url=http://eurheartj.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=1334465}}</ref>
| |
| | |
| ===VA Conduction===
| |
| A major cause of AV dyssynchrony is VA conduction. VA conduction, sometimes referred to as retrograde conduction, leads to delayed, nonphysiologic timing of [[atrium (heart)|atrial]] contraction in relation to [[ventricle (heart)|ventricular]] [[muscle contraction|contraction]]. Nevertheless, many conditions other than VA conduction promote AV dyssynchrony.<ref name="pmid9164889"/><ref name="pmid12555483" /><ref name="pmid7821326"/><ref name="pmid1413181" /><ref name="pmid2032410"/>
| |
| | |
| This will further decrease [[blood pressure]], and secondary increase in [[atrial natriuretic peptide|ANP]] and [[brain natriuretic peptide|BNP]].<ref name="pmid9036762"/><ref name="pmid1334465"/>
| |
| | |
| ==Epidemiology and Demographics==
| |
| The reported [[incidence]] of pacemaker syndrome has ranged from 2%<ref name="pmid7983951">{{cite journal |author=Andersen HR, Thuesen L, Bagger JP, Vesterlund T, Thomsen PE |title=Prospective randomised trial of atrial versus ventricular pacing in sick-sinus syndrome |journal=[[The Lancet|Lancet]] |volume=344 |issue=8936 |pages=1523–8 |year=1994 |month=December |pmid=7983951 |doi= 10.1016/S0140-6736(94)90347-6|url=http://linkinghub.elsevier.com/retrieve/pii/S0140-6736(94)90347-6 |issn= |accessdate=2009-06-19}}</ref> to 83%.<ref name="pmid1704534">{{cite journal |author=Heldman D, Mulvihill D, Nguyen H, ''et al.'' |title=True incidence of pacemaker syndrome |journal=[[Pacing and Clinical Electrophysiology : PACE]] |volume=13 |issue=12 Pt 2 |pages=1742–50 |year=1990 |month=December |pmid=1704534 |doi= 10.1111/j.1540-8159.1990.tb06883.x|url= |issn= |accessdate=2009-06-19}}</ref> The wide range of reported incidence is likely attributable to two factors which are the criteria used to define pacemaker syndrome and the therapy used to resolve that diagnosis.<ref name="pmid16943933">{{cite journal |author=Farmer DM, Estes NA, Link MS |title=New concepts in pacemaker syndrome |journal=[[Indian Pacing and Electrophysiology Journal]] |volume=4 |issue=4 |pages=195–200 |year=2004 |pmid=16943933 |pmc=1502063 |doi= |url=http://www.ipej.org/4/195 |issn= |accessdate=2009-06-19}}</ref>
| |
| | |
| ==Risk Factors==
| |
| *In the pre-implantation period, two variables are predicted to predispose to the syndrome. First is low [[sinus node|sinus rate]], and second is a higher programmed lower rate limit. In post-implantation, an increased percentage of [[ventricle|ventricular]] paced beats is the only variable that significantly predicts development of pacemaker syndrome.
| |
| | |
| *Patients with intact VA conduction are at greater risk for developing pacemaker syndrome. Around 90% of patients with preserved AV conduction have intact VA conduction, and about 30-40% of patients with complete [[Atrioventricular block|AV block]] have preserved VA conduction. Intact VA conduction may not be apparent at the time of pacemaker implantation or even may develop at any time after implantation.<ref name="pmid1704534">{{cite journal |author=Heldman D, Mulvihill D, Nguyen H, ''et al.'' |title=True incidence of pacemaker syndrome |journal=Pacing Clin Electrophysiol |volume=13 |issue=12 Pt 2 |pages=1742–50 |year=1990 |month=December |pmid=1704534 |doi=10.1111/j.1540-8159.1990.tb06883.x }}</ref>
| |
| | |
| *Patients with noncompliant [[ventricle (heart)|ventricles]] and [[diastolic]] dysfunction are particularly sensitive to loss of [[atrial]] contribution to ventricular filling, where that highly increase the chance of developing the syndrome. This includes patients with [[cardiomyopathy]] ([[hypertensive cardiomyopathy|hypertensive]], [[hypertrophic cardiomyopathy|hypertrophic]], [[restrictive cardiomyopathy|restrictive]]) and elderly individuals.
| |
| | |
| *Other factors correlated with development of pacemaker syndrome include decreased [[stroke volume]], decreased [[cardiac output]], and decreased [[left atrium|left atrial]] total emptying fraction associated with [[ventricle|ventricular]] pacing.
| |
| | |
| ==Natural History, Complications and Prognosis==
| |
| ===Complications===
| |
| Studies have shown that patients with pacemaker syndrome and/or with [[sick sinus syndrome]] are at higher risk of developing fatal complications that calls for the patients to be carefully monitored in the [[ICU]]. Complications include:
| |
| * [[Atrial fibrillation]]
| |
| * [[thrombo-embolic disease|Thrombo-embolic events]]
| |
| * [[Heart failure]]<ref name="pmid2316455"/>
| |
|
| |
|
| ==Diagnosis== | | ==Diagnosis== |
| ===Symptoms===
| |
| No specific set of criteria has been developed for [[diagnosis]] of [[pacemaker]] [[syndrome]]. Most of the signs and [[symptoms]] of pacemaker syndrome are nonspecific, and many are prevalent in the elderly population at baseline. In the lab, pacemaker interrogation plays a crucial role in determining if the pacemaker mode had any contribution to symptoms.<ref name="pmid7511223"/><ref name="pmid6184693">{{cite journal |author=Nishimura RA, Gersh BJ, Vlietstra RE, Osborn MJ, [[Duane Ilstrup|Ilstrup DM]], Holmes DR |title=Hemodynamic and symptomatic consequences of ventricular pacing |journal=Pacing Clin Electrophysiol |volume=5 |issue=6 |pages=903–10 |year=1982 |month=November |pmid=6184693 }}</ref><ref name="pmid2316455">{{cite journal |author=Santini M, Alexidou G, Ansalone G, Cacciatore G, Cini R, Turitto G |title=Relation of prognosis in sick sinus syndrome to age, conduction defects and modes of permanent cardiac pacing |journal=Am. J. Cardiol. |volume=65 |issue=11 |pages=729–35 |year=1990 |month=March |pmid=2316455 |url=http://linkinghub.elsevier.com/retrieve/pii/0002-9149(90)91379-K |doi=10.1016/0002-9149(90)91379-K |format= }} {{dead link|date=May 2010}}</ref>
| |
|
| |
| Symptoms commonly documented in patients history, classified according to [[etiology]]:<ref name="pmid12555483">{{cite journal |author=Chalvidan T, Deharo JC, Djiane P |title=[Pacemaker syndromes] |language=French |journal=Ann Cardiol Angeiol (Paris) |volume=49 |issue=4 |pages=224–9 |year=2000 |month=July |pmid=12555483 |doi= |url=}}</ref><ref name="pmid7511223"/><ref name="pmid6184693"/><ref name="pmid1413181">{{cite journal |author=Petersen HH, Videbaek J |title=[The pacemaker syndrome] |language=Danish |journal=Ugeskr. Laeg. |volume=154 |issue=38 |pages=2547–51 |year=1992 |month=September |pmid=1413181 }}</ref><ref name="pmid677029">{{cite journal |author=Alicandri C, Fouad FM, Tarazi RC, Castle L, Morant V |title=Three cases of hypotension and syncope with ventricular pacing: possible role of atrial reflexes |journal=Am. J. Cardiol. |volume=42 |issue=1 |pages=137–42 |year=1978 |month=July |pmid=677029 |doi=10.1016/0002-9149(78)90998-0 }}</ref>
| |
|
| |
| *[[Neurological]] - [[Dizziness]], near [[Syncope (medicine)|syncope]], and [[confusion]].
| |
| *[[Heart failure]] - [[Dyspnea]], [[orthopnea]], [[paroxysmal nocturnal dyspnea]], and [[edema]].
| |
| *[[Hypotension]] - [[Seizure]], [[mental status]] change, [[diaphoresis]], and signs of [[orthostatic hypotension]] and [[hypovolemic shock|shock]].
| |
| *Low [[cardiac output]] - [[Fatigue (medical)|Fatigue]], [[weakness]], [[dyspnea on exertion]], [[lethargy]], and lightheadedness.
| |
| *[[Hemodynamic]] - [[pulse|Pulsation]] in the neck and [[abdomen]], [[choking]] sensation, [[jaw]] pain, [[right upper quadrant]] (RUQ) pain and [[headache]].
| |
| *[[Heart rate]] related - [[Palpitations]] associated with [[arrhythmias]]
| |
|
| |
| In particular, the examiner should look for the following in the [[physical examination]], as these are frequent findings at the time of admission:<ref name="pmid12555483" /><ref name="pmid7511223"/><ref name="pmid6184693"/><ref name="pmid1413181" />
| |
|
| |
| *[[Vital signs]] may reveal [[hypotension]], [[tachycardia]], [[tachypnea]], or low [[oxygen saturation]].
| |
| *[[Pulse amplitude]] may vary, and [[blood pressure]] may fluctuate.
| |
| *Look for neck [[vein]] [[distension]]{{disambiguation needed|date=March 2012}} and [[Cannon A waves|cannon waves]] in the neck veins.
| |
| *[[Lungs]] may exhibit crackles.
| |
| *[[Cardiac]] examination may reveal [[Regurgitation (circulation)|regurgitant]] [[murmurs]] and variability of [[heart sounds]].
| |
| *[[Liver]] may be pulsatile, and the [[Right upper quadrant|RUQ]] may be [[Tenderness|tender]]{{disambiguation needed|date=March 2012}} to [[palpation]]. [[Ascites]] may be present in severe cases.
| |
| *[[lower limbs|The lower extremities]] may be [[edematous]].
| |
| *[[Neurologic]] examination may reveal [[confusion]], [[dizziness]], or altered [[mental status]].
| |
|
| |
| ===Physical Examination===
| |
| ====Appearance of the Patient====
| |
| * [[Diaphoretic]]
| |
|
| |
| ====Vitals====
| |
| =====Pulse=====
| |
| * [[Tachycardia]]
| |
| =====Blood Pressure=====
| |
| * [[Orthostatic hypotension]]
| |
| * [[Hypovolemic shock]]
| |
|
| |
|
| |
|
| |
| =====Respiratory Rate=====
| |
|
| |
| * [[Tachypnea]]
| |
|
| |
|
| |
|
| |
|
| |
| ====Neck====
| |
|
| |
| * Neck [[vein]] [[distension]] (elevated [[JVP]])
| |
|
| |
| * [[Cannon A waves|cannon waves]] in the neck veins
| |
|
| |
|
| |
|
| |
|
| |
| ====Lungs====
| |
|
| |
| * [[Lungs]] may exhibit crackles
| |
|
| |
|
| |
|
| |
|
| |
| ====Heart====
| |
|
| |
| *[[Cardiac]] examination may reveal regurgitant [[murmurs]] and variability of [[heart sounds]]
| |
|
| |
|
| |
|
| |
|
| |
| ====Abdomen====
| |
|
| |
| *[[Liver]] may be pulsatile, and the [[Right upper quadrant|RUQ]] may be [[Tenderness|tender]] to [[palpation]].[[Ascites]] may be present in severe cases.
| |
|
| |
|
| |
| ====Extremities====
| |
| * [[Edema]]
| |
|
| |
|
| |
|
| |
|
| | [[Pacemaker syndrome history and symptoms|History and Symptoms ]] | [[ Pacemaker syndrome physical examination|Physical Examination]] | [[Pacemaker syndrome laboratory findings|Laboratory Findings]] | [[Pacemaker syndrome electrocardiogram|Electrocardiogram]] | [[Pacemaker syndrome chest x ray|Chest X Ray]] | [[Pacemaker syndrome echocardiography|Echocardiography]] | [[Pacemaker syndrome other imaging findings|Other Imaging Findings]] | [[Pacemaker syndrome other diagnostic studies|Other Diagnostic Studies]] |
|
| |
|
| ====Neurologic==== | | ==Treatment== |
| | [[Pacemaker syndrome medical therapy|Medical Therapy]] | [[Pacemaker syndrome surgery |Surgery]] | [[Pacemaker syndrome primary prevention|Primary Prevention]] | [[Pacemaker syndrome secondary prevention|Secondary Prevention]] | [[Pacemaker syndrome cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Pacemaker syndrome future or investigational therapies|Future or Investigational Therapies]] |
|
| |
|
| *[[Neurologic]] examination may reveal [[confusion]], [[dizziness]], or altered [[mental status]].
| | ==Case Studies== |
| | [[Pacemaker syndrome case study one|Case #1]] |
|
| |
|
| ==References==
| |
| {{Reflist|2}}
| |
| {{WH}} | | {{WH}} |
| {{WS}} | | {{WS}} |