Ovarian cancer epidemiology and demographics
|
Ovarian cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Ovarian cancer epidemiology and demographics On the Web |
|
American Roentgen Ray Society Images of Ovarian cancer epidemiology and demographics |
|
Risk calculators and risk factors for Ovarian cancer epidemiology and demographics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Ovarian cancer is the fifth leading cause of cancer death in women, the leading cause of death from gynecological malignancy, and the second most commonly diagnosed gynecologic malignancy.[1]
Epidemiology and Demographics
The exact cause is usually unknown. The disease is more common in industrialized nations, with the exception of Japan. In the United States, females have a 1.4% to 2.5% (1 out of 40-60 women) lifetime chance of developing ovarian cancer.
Older women are at highest risk. More than half of the deaths from ovarian cancer occur in women between 55 and 74 years of age and approximately one quarter of ovarian cancer deaths occur in women between 35 and 54 years of age.
The risk of developing ovarian cancer appears to be affected by several factors. The more children a woman has, the lower her risk of ovarian cancer. Early age at first pregnancy, older ages of final pregnancy and the use of low dose hormonal contraception have also been shown to have a protective effect. Ovarian cancer is reduced in women after tubal ligation.
The link to the use of fertility medication, such as Clomiphene citrate, has been controversial. An analysis in 1991 raised the possibility that use of drugs may increase the risk of ovarian cancer. Several cohort studies and case-control studies have been conducted since then without providing conclusive evidence for such a link. [2] It will remain a complex topic to study as the infertile population differs in parity from the "normal" population.
There is good evidence that in some women genetic factors are important. Carriers of certain mutations of the BRCA1 or the BRCA2 gene and certain populations (e.g. Ashkenazi Jewish women) are at a higher risk of both breast cancer and ovarian cancer, often at an earlier age than the general population. Patients with a personal history of breast cancer or a family history of breast and/or ovarian cancer, especially if at a young age, may have an elevated risk. A strong family history of uterine cancer, colon cancer, or other gastrointestinal cancers may indicate the presence of a syndrome known as hereditary nonpolyposis colorectal cancer (HNPCC, also known as Lynch II syndrome), which confers a higher risk for developing ovarian cancer. Patients with strong genetic risk for ovarian cancer may consider the use of prophylactic i.e. preventative oophorectomy after completion of child-bearing.
A Swedish study, which followed more than 61,000 women for 13 years, has found a significant link between milk consumption and ovarian cancer. According to the BBC, "[Researchers] found that milk had the strongest link with ovarian cancer - those women who drank two or more glasses a day were at double the risk of those who did not consume it at all, or only in small amounts." [3] Recent studies have shown that women in sunnier countries have a lower rate of ovarian cancer, which may have some kind of connection with exposure to Vitamin D.
Other factors that have been investigated, such as talc use, asbestos exposure, high dietary fat content, and childhood mumps infection, are controversial and have not been definitively proven.
"Associations were also found between alcohol consumption and cancers of the ovary and prostate, but only for 50 g and 100 g a day."[4]
Prevalence
- In the United States, the age-adjusted prevalence of ovarian cancer is 71.3 per 100,000 in 2011.[5]
Incidence
- The delay-adjusted incidence of ovarian cancer in 2011 was estimated to be 12.46 per 100,000 persons in the United States.[5]
- In 2011, the age-adjusted incidence of ovarian cancer was 12.09 per 100,000 persons in the United States.[5]
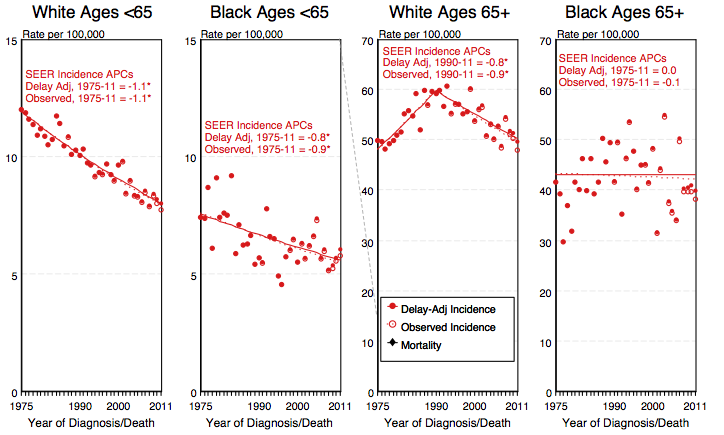
Age
- While the overall age-adjusted incidence of ovarian cancer in the United States between 2007 and 2011 is 12.3 per 100,000, the age-adjusted incidence of ovarian cancer by age category is:[5]
- Under 65 years: 7.5 per 100,000
- 65 and over: 45.2 per 100,000
- Shown below is an image depicting the delay-adjusted incidence and observed incidence of ovarian cancer by age and race in the United States between 1975 and 2011. These graphs are adapted from SEER: The Surveillance, Epidemiology, and End Results Program of the National Cancer Institute.[5]
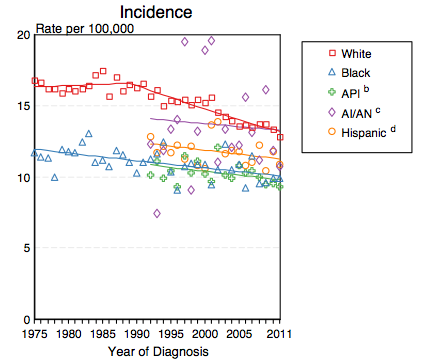
Race
- Shown below is a table depicting the age-adjusted prevalence of ovarian cancer by race in 2011 in the United States.[5]
| All Races | White | Black | Asian/Pacific Islander | Hispanic | |
| Age-adjusted prevalence | 71.3 per 100,000 | 76.2 per 100,000 | 44.2 per 100,000 | 63.2 per 100,000 | 59.1 per 100,000 |
- Shown below is an image depicting the incidence of ovarian cancer by race in the United States between 1975 and 2011.[5]
API: Asian/Pacific Islander; AI/AN: American Indian/ Alaska Native
Percent Distribution of Ovarian Cancer by Histology
- Among patients with histologically confirmed cases of ovarian cancer, the percent distribution of the types of the disease between 2007 and 2011 in the United States are:[5]
References
- ↑ The Merck Manual of Diagnosis and Therapy Section 18. Gynecology And Obstetrics Chapter 241. Gynecologic Neoplasms
- ↑ Brinton LA, Moghissi KS, Scoccia B, Westhoff CL, Lamb EJ (2005). "Ovulation induction and cancer risk". Fertil. Steril. 83 (2): 261–74, quiz 525-6. doi:10.1016/j.fertnstert.2004.09.016. PMID 15705362.
- ↑ BBC News Milk link to ovarian cancer risk 29 November 2004
- ↑ Alcohol consumption and cancer risk
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.