Osteoarthritis overview: Difference between revisions
Irfan Dotani (talk | contribs) No edit summary |
Irfan Dotani (talk | contribs) No edit summary |
||
| Line 11: | Line 11: | ||
=='''Overview'''== | =='''Overview'''== | ||
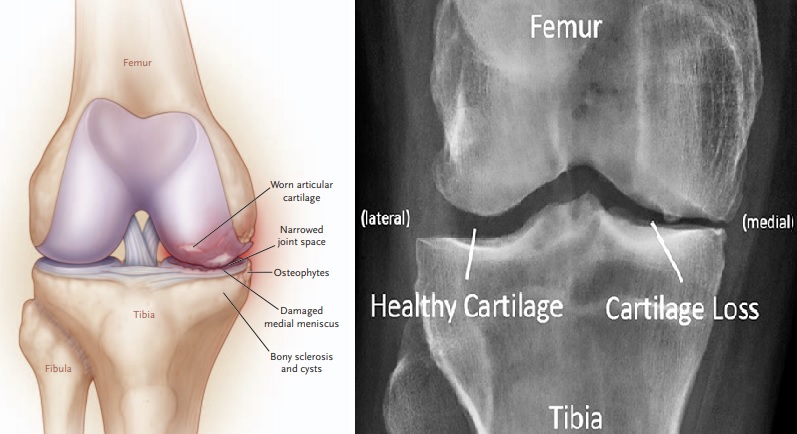
'''Osteoarthritis / Osteoarthrosis''' (OA, also known as [[degenerative joint disease]], [[degenerative arthritis]], arthrosis or in more colloquial terms "wear and tear") is the most common form of arthritis, caused by wearing of the [[cartilage]] that covers and cushions joint spaces. As the cartilage wears away, the patient may experience pain described as "weight-bearing" whenever walking and standing. Due to the movement limitations caused by pain, regional muscles may experience [[atrophy]]. [[Ligament|Ligaments]] may become laxer as well due to this. OA is derived from the Greek word "''osteo''", meaning "of the bone", "''arthro''", meaning "joint", and "''itis''", meaning [[inflammation]], although inflammation is not a common finding in this regard. [[Osteoarthritis|OA]] possesses a great degree of variability in disease onset, progression, and severity. [[Osteoarthritis|OA]] is characterized by a variety of structural and functional impairments occurring in an involved joint. Destruction, degeneration, articular cartilage loss, and even the soft tissue involvement are the main pathological process of this disease. It can be diagnosed through radiographic evaluations. Moreover, clinical sign and symptoms are helpful in the final diagnosis of this disease. OA can be defined radiologically, clinically, or pathologically, with radiographic OA being considered as the reference standard [5]. The symptoms that are consistently associated with OA are joint pain, stiffness, swelling, and limitation of joint function. Few individuals who present these symptoms may not demonstrate radiographic OA. However, others confirmed to have OA using radiographic techniques may not present with clinical manifestations of the disease [5]. These unique characteristics have made it difficult to identify the underlying mechanisms contributing to the disease as well as the treatments for reducing the incidence and severity of the disease. In addition, the stimuli that may initiate the processes associated with OA are multifactorial and include occupational and non-occupational (e.g., genetics, obesity, age, etc.) factors. [[Osteoarthritis|OA]] affects nearly 43 million patients in [[United States]] and almost 15% of the world population, accounting for 25% of visits to [[Primary care physician|primary care physicians]], and half of all [[NSAID]] (Non-Steroidal Anti-Inflammatory Drugs) [[Medical prescription|prescriptions]]. It is estimated that 80% of the population will have [[Radiograph|radiographic]] evidence of OA by age 65, although only 60% of those will be [[symptomatic]].[[Osteoarthritis overview#cite note-1|[1]]] | '''Osteoarthritis / Osteoarthrosis''' (OA, also known as [[degenerative joint disease]], [[degenerative arthritis]], arthrosis or in more colloquial terms "wear and tear") is the most common form of arthritis, caused by wearing of the [[cartilage]] that covers and cushions joint spaces. As the cartilage wears away, the patient may experience pain described as "weight-bearing" whenever walking and standing. Due to the movement limitations caused by pain, regional muscles may experience [[atrophy]]. [[Ligament|Ligaments]] may become laxer as well due to this. OA is derived from the Greek word "''osteo''", meaning "of the bone", "''arthro''", meaning "joint", and "''itis''", meaning [[inflammation]], although inflammation is not a common finding in this regard. [[Osteoarthritis|OA]] possesses a great degree of variability in disease onset, progression, and severity. [[Osteoarthritis|OA]] is characterized by a variety of structural and functional impairments occurring in an involved joint. Destruction, degeneration, articular cartilage loss, and even the soft tissue involvement are the main pathological process of this disease. It can be diagnosed through radiographic evaluations. Moreover, clinical sign and symptoms are helpful in the final diagnosis of this disease. OA can be defined radiologically, clinically, or pathologically, with radiographic OA being considered as the reference standard [5]. The symptoms that are consistently associated with OA are joint pain, stiffness, swelling, and limitation of joint function. Few individuals who present these symptoms may not demonstrate radiographic OA. However, others confirmed to have OA using radiographic techniques may not present with clinical manifestations of the disease [5]. These unique characteristics have made it difficult to identify the underlying mechanisms contributing to the disease as well as the treatments for reducing the incidence and severity of the disease. In addition, the stimuli that may initiate the processes associated with OA are multifactorial and include occupational and non-occupational (e.g., genetics, obesity, age, etc.) factors. [[Osteoarthritis|OA]] affects nearly 43 million patients in [[United States]] and almost 15% of the world population, accounting for 25% of visits to [[Primary care physician|primary care physicians]], and half of all [[NSAID]] (Non-Steroidal Anti-Inflammatory Drugs) [[Medical prescription|prescriptions]]. It is estimated that 80% of the population will have [[Radiograph|radiographic]] evidence of OA by age 65, although only 60% of those will be [[symptomatic]].[[Osteoarthritis overview#cite note-1|[1]]] There is no recent discovery of a cure for OA, as cartilage has not been induced to regenerate. However, if OA is caused by cartilage damage (for example as a result of an injury) Autologous Chondrocyte Implantation may be a possible treatment. Other treatments are with NSAIDs, local injections of [[glucocorticoid]] or [[hyaluronan]], and in severe cases, with [[joint replacement]] surgery. Many physicians have also reported good pain relief by treating ligaments (which is responsible for a bone to bone connection) with [[Prolotherapy]]. Clinical trials employing [[Tissue engineering|tissue-engineering]] methods have demonstrated regeneration of cartilage in damaged knees, including those that have progressed to osteoarthritis.[[Osteoarthritis overview#cite note-2|[2]]] Furthermore, in January 2007, Johns Hopkins University was offering to license a technology of this kind, listing several clinical competitors in its market analysis. Osteoarthritis is capable of influencing any joint in the human body; meanwhile, the most commonly affected joints are the knee and hip joints given that the degree of weight bearing required of these joints is immense. Other joints, such as the [[distal interphalangeal joints]] of the fingers and shoulder joints are also commonly affected as well. The economic burden of OA for United States economy is more than $60 billion per year; which have more economic pressure than [[rheumatoid arthritis]]. This cost can be considered into two subgroups: the medical related costs and the lost expediency of patients at work. | ||
=='''Historical Perspective'''== | =='''Historical Perspective'''== | ||
Revision as of 20:22, 15 April 2018
| https://https://www.youtube.com/watch?v=sUOlmI-naFs%7C350}} |
|
Osteoarthritis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Osteoarthritis overview On the Web |
|
American Roentgen Ray Society Images of Osteoarthritis overview |
|
Risk calculators and risk factors for Osteoarthritis overview |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mohammadmain Rezazadehsaatlou, Irfan Dotani
Overview
Osteoarthritis / Osteoarthrosis (OA, also known as degenerative joint disease, degenerative arthritis, arthrosis or in more colloquial terms "wear and tear") is the most common form of arthritis, caused by wearing of the cartilage that covers and cushions joint spaces. As the cartilage wears away, the patient may experience pain described as "weight-bearing" whenever walking and standing. Due to the movement limitations caused by pain, regional muscles may experience atrophy. Ligaments may become laxer as well due to this. OA is derived from the Greek word "osteo", meaning "of the bone", "arthro", meaning "joint", and "itis", meaning inflammation, although inflammation is not a common finding in this regard. OA possesses a great degree of variability in disease onset, progression, and severity. OA is characterized by a variety of structural and functional impairments occurring in an involved joint. Destruction, degeneration, articular cartilage loss, and even the soft tissue involvement are the main pathological process of this disease. It can be diagnosed through radiographic evaluations. Moreover, clinical sign and symptoms are helpful in the final diagnosis of this disease. OA can be defined radiologically, clinically, or pathologically, with radiographic OA being considered as the reference standard [5]. The symptoms that are consistently associated with OA are joint pain, stiffness, swelling, and limitation of joint function. Few individuals who present these symptoms may not demonstrate radiographic OA. However, others confirmed to have OA using radiographic techniques may not present with clinical manifestations of the disease [5]. These unique characteristics have made it difficult to identify the underlying mechanisms contributing to the disease as well as the treatments for reducing the incidence and severity of the disease. In addition, the stimuli that may initiate the processes associated with OA are multifactorial and include occupational and non-occupational (e.g., genetics, obesity, age, etc.) factors. OA affects nearly 43 million patients in United States and almost 15% of the world population, accounting for 25% of visits to primary care physicians, and half of all NSAID (Non-Steroidal Anti-Inflammatory Drugs) prescriptions. It is estimated that 80% of the population will have radiographic evidence of OA by age 65, although only 60% of those will be symptomatic.[1] There is no recent discovery of a cure for OA, as cartilage has not been induced to regenerate. However, if OA is caused by cartilage damage (for example as a result of an injury) Autologous Chondrocyte Implantation may be a possible treatment. Other treatments are with NSAIDs, local injections of glucocorticoid or hyaluronan, and in severe cases, with joint replacement surgery. Many physicians have also reported good pain relief by treating ligaments (which is responsible for a bone to bone connection) with Prolotherapy. Clinical trials employing tissue-engineering methods have demonstrated regeneration of cartilage in damaged knees, including those that have progressed to osteoarthritis.[2] Furthermore, in January 2007, Johns Hopkins University was offering to license a technology of this kind, listing several clinical competitors in its market analysis. Osteoarthritis is capable of influencing any joint in the human body; meanwhile, the most commonly affected joints are the knee and hip joints given that the degree of weight bearing required of these joints is immense. Other joints, such as the distal interphalangeal joints of the fingers and shoulder joints are also commonly affected as well. The economic burden of OA for United States economy is more than $60 billion per year; which have more economic pressure than rheumatoid arthritis. This cost can be considered into two subgroups: the medical related costs and the lost expediency of patients at work.
Historical Perspective
The earliest descriptions of OA were provided by Heberden and Haygarth in the 19th century. [3] [4] In the 1930s and 1940s, Dr. Stecher showed that there were two forms of OA, idiopathic and post-traumatic. [5] And, in the 1950s the links between Heberden’s nodes and large joint OA were revealed by Kellgren and Moore. In this regard, the first x-ray grading system for OA was developed by Jonas Kellgren and John Lawrence in the 1950s. Surgical management of OA was developed in the 1960s by Drs. Charnley and McKee
Classification
Osteoarthritis is radiographically classified depending on degree of joint involvement. The Kellgren-Lawrence is a common method to classify the severity of OA in knee using five different grades. This classification was proposed by Kellgren et al. in 1957 and then it was accepted by WHO in 1961.
| I: Idiopathic | |||
|---|---|---|---|
| A: Localized | |||
| 1: Hands: Heberden’s and Bouchard’s nodes (nodal), erosive interphalangeai arthritis (nonnodal), scaphometacarpal joint, scaphotrapezial | |||
| 2. Feet: hallux valgus. hallux rigidus, contracted toes (hammer/cockup toes), talonavicular | |||
| 3. Knee | a. Medial compartment
b. Lateral compartment c. Patellofemoral compartment (chondromalacia) | ||
| 4. Hip | a. Eccentric (superior)
b. Concentric (axial, medial) c. Diffuse (coxae senilis) | ||
| 5. Spine (particularly cervical and lumbar) | a. Apophyseal
b. Intervertebral (disc) c. Spondylosis (osteophytes) d. Ligamentous (hyperostosis [Forestier’s disease or DISH]) | ||
| 6. Other single sites: shoulder, temporomandibular, sacroiliac, ankle, wrist, acromioclavicular | |||
| B. Generalized: includes 3 or more areas listed above (Kellgren-Moore) | 1. Small (peripheral) and spine
2. Large (central) and spine 3. Mixed (peripheral and central) and spine |
||
| II. Secondary | |||
| A. Posttraumatic | |||
| B. Congenital or Developmental Diseases | 1. Localized | a. Hip diseases: Legg-Calve-Perthes, congenital hip dislocation, slipped capital femoral epiphysis, shallow acetabulum
b. Mechanical and local factors: obesity (7). unequal lower extremity length, extreme valgus/varus deformity, hypermobility syndromes, scoliosis | |
| 2. Generalized | a. Bone dysplasias: epiphyseal dysplasia, spondyloapophyseal dysplasia
b. Metabolic diseases: hemachromatosis, ochronosis, Gaucher’s disease, hemoglobinopathy, Ehlers-Danlos | ||
| c. Calcium Deposition Disease | 1. Calcium pyrophosphate deposition disease
2. Apatite atthropathy 3. Destructive arthropathy (shoulder, knee) |
||
| D. Other Bone and Joint Disorders: avascular necrosis, rheumatoid arthritis, gouty arthritis, septic arthritis, Paget’s disease, osteopetrosis, osteochondritis | |||
| E. Other Diseases | 1. Endocrine diseases: diabetes mellitus, acromegaly, hypothyroidism, hyperparathyroidism
2. Neuropathic arthropathy (Charcot joints) 3. Miscellaneous: frostbite, Kashin-Beck disease, Caisson’s disease |
Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) is used to evaluate the pain, stiffness, and physical function among patients with hip or/and knee osteoarthritis (OA) and it is consists of 24 different items divided into 3 subtypes:
- Pain consisted of 5 items: staying in bed, sitting or lying, and standing. during walking, and using stairs,
- Stiffness consisted of 2 items: after waking up in morning and later in the day.
- Physical Function consisted of 17 items: using stairs, sitting, rising from sitting, standing, bending, walking, getting in and/or getting out of a car, during shopping, heavy household duties, light household duties, putting on/taking off socks, lying in bed, rising from bed, getting in and/or getting out of bath, getting on/off toilet.
Knee
| Grade | Description |
|---|---|
| A | No joint space narrowing (JSN) |
| B | >4 mm joint space; small osteophytes, slight sclerosis, or femoral condyle flattening |
| C | 2-4 mm joint space |
| D | <2 mm joint space |
| Grade | Description |
|---|---|
| I (mild) | Patellofemoral joint space > 3mm |
| II (moderate) | Joint space < 3 mm but no bony contact |
| III(severe) | Bony surfaces in contact over less than one quarter of the joint surface |
| IV (very severe) | Bony contact throughout the entire joint surface |
| Grade | Description |
|---|---|
| 0 | Normal |
| 1 | Joint space narrowing is <3 mm of the joint space or <50% of the other compartment (with or without subchondral sclerosis) |
| 2 | Obliteration of joint space |
| 3 | Bone defect/loss <5 mm |
| 4 | Bone defect and/or loss 5-10 mm |
Hip
| Grade | Description |
|---|---|
| 0 | No joint space narrowing (JSN) or reactive changes |
| I | Doubtful JSN, possible osteophytic lipping |
| II | Definite osteophytes, possible JSN |
| III | Moderate osteophytes, definite JSN, some sclerosis, possible bone-end deformity |
| IV | Large osteophytes, marked JSN, severe sclerosis, definite bone ends deformity |
| Grade | Description |
|---|---|
| 0 | No osteoarthritis signs |
| I (Mild) | Increased sclerosis, slight narrowing of the joint space, no or slight loss of head sphericity or lipping at the joint margins |
| II (Moderate) | Small cysts, moderate narrowing of the joint space, moderate loss of head sphericity |
| III (Severe) | Large cysts, severe narrowing or obliteration of the joint space, severe deformity of the head |
Shoulder
| Grade | Description |
|---|---|
| I | Inferior humeral or glenoid exostosis, or both, measuring less than 3 mm in height. |
| II | Inferior humeral or glenoid exostosis, or both, between 3 and 7 mm in height, with slight glenohumeral joint irregularity. |
| III | Inferior humeral or glenoid exostosis, or both, more than 7 mm in height, with narrowing of the glenohumeral joint and sclerosis |
Vertebral column
| Grade | Description |
|---|---|
| I | Minimal anterior osteophytosis |
| II | Definite anterior osteophytosis with possible narrowing of the disc space and some sclerosis of vertebral plates |
| III | Moderate narrowing of the disc space with definite sclerosis of vertebral plates and osteophytosis |
| IV | Severe narrowing of the disc space with sclerosis of vertebral plates and multiple large osteophytes |
| Grade | Description |
|---|---|
| 1 | Doubtful osteophytes on margins of the articular facets of apophyseal joints |
| 2 | Definite osteophytes and subchondral sclerosis in apophyseal joints |
| 3 | Moderate osteophytes, subchondral sclerosis and some irregularity of articular facets |
| 4 | Many large osteophytes and severe sclerosis and irregularity of the apophyseal joints |
| Grade | Joint space narrowing | Osteophytes anterior and posterior | Sclerosis |
|---|---|---|---|
| 0 | None | None | None |
| I | Definite (mild) narrowing | Small | Present |
| II | Moderate | Moderate | – |
| III | Severe (complete loss of joint space) | Large | – |
| Grade | Nucleus | Anulus | Endplate | Vertebral body |
|---|---|---|---|---|
| I | Bulging gel | Discrete fibrous laminae | Hyaline, uniform thickness | Rounded margins |
| II | Peripheral white fibrous tissue | Mucinous material between laminae | Irregular thickness | Pointed margins |
| III | Consolidated fibrous tissue | Extensive mucinous infiltration; loss of annular-nuclear demarcation | Focal defects in cartilage | Small chondrophytes or osteophytes at margins |
| IV | Horizontal clefts parallel to endplate | Focal disruptions | Fibrocartilage extending from subchondral bone; irregularity and focal sclerosis in subchondral bone | Osteophytes smaller than 2 mm |
| V | Clefts extended through nucleus and annulus | Diffuse sclerosis | Osteophytes greater than 2 mm |
| Grade | Description |
|---|---|
| 0 | Normal |
| I | Joint space narrowing (mild degenerative disease) |
| II | Narrowing plus sclerosis or hypertrophy (moderate degenerative disease) |
| III | Severe osteoarthrosis with narrowing, sclerosis, and osteophytes (severe degenerative disease) |
| Grade | Description |
|---|---|
| 0 | Normal facet joint space (2–4 mm width) |
| I | Narrowing of the facet joint space (<2 mm) and/or small osteophytes and/or mild hypertrophy of the articular process |
| II | Narrowing of the facet joint space and/or moderate osteophytes and/or moderate hypertrophy of the articular process and/or mild subarticular bone erosions |
| III | Narrowing of the facet joint space and/or large osteophytes and/or severe hypertrophy of the articular process and/or severe subarticular bone erosions and/or subchondral cysts |
Temporomandibular joint
| flattening: common (in one series 27%) |
| osteophytes: common (27%) |
| erosions: 13% |
| sclerosis: less common (9%) |
| subchondral cysts |
Ankle
| Grade | Description |
| I | Early sclerosis and osteophyte formation, no joint space narrowing |
| II | Narrowing of medial joint space (no subchondral bone contact) |
| IIIA | Obliteration of joint space at the medial malleolus, with subchondral bone contact |
| IIIB | Obliteration of joint space over roof of talar dome, with subchondral bone contact |
| IV | Obliteration of joint space with complete bone contact |
| Grade | Description |
| 0 | Normal joint or subchondral sclerosis |
| I | Presence of osteophytes without joint-space narrowing |
| II | Joint-space narrowing with or without osteophytes |
| III | Subtotal or total disappearance or deformation of joint space |
| Grade | Description |
| 0 | No reduction of the joint space
Normal alignment |
| I | Slight reduction of the joint space
Slight formation of deposits at the joint margins Normal alignment |
| II | More pronounced change than mentioned above
Subchondral osseous sclerotic configuration Mild malalignment |
| III | Joint space reduced to about half the height of the uninjured side
Rather pronounced formation of deposits Obvious varus or valgus alignment |
| IV | Joint space has completely or practically disappeared |
| Grade | Description |
| I | Isolated ankle arthritis |
| II | Ankle arthritis with intra-articular varus or valgus deformity or a tight heel cord, or both |
| III | Ankle arthritis with hindfoot deformity, tibial malunion, midfoot abductus or adductus, supinated midfoot, plantarflexed first ray, etc |
| IV | Types 1–3 plus subtalar, calcaneocuboid, or talonavicular arthritis |
Pathophysiology
Causes
Differentiating Osteoarthritis overview from Other Diseases
Epidemiology and Demographics
Risk Factors
Screening
Routine screening for osteoarthritis is not indicated unless the patient is symptomatic.