Oral cancer causes
|
Oral cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Oral cancer causes On the Web |
|
American Roentgen Ray Society Images of Oral cancer causes |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]:Associate Editor(s)-in-Chief: Simrat Sarai, M.D. [2]
Overview
Common causes of oral cancer include premalignant lesion, tobacco, alcohol, human papillomavirus, and hematopoietic stem cell transplantation.
Causes
Common causes of oral cancer include:
Premalignant lesion
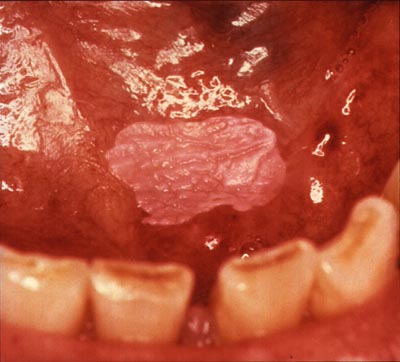
A premalignant (or precancerous) lesion is defined as "a benign, morphologically altered tissue that has a greater than normal risk of malignant transformation." There are several different types of premalignant lesion that occur in the mouth. Some oral cancers begin as white patches (leukoplakia), red patches (erythroplakia) or mixed red and white patches (erythroleukoplakia or "speckled leukoplakia"). Other common premalignant lesions include oral lichen planus (particularly the erosive type), oral submucous fibrosis and actinic cheilitis. In the Indian subcontinent oral submucous fibrosis is very common. This condition is characterized by limited opening of mouth and burning sensation on eating of spicy food. This is a progressive lesion in which the opening of the mouth becomes progressively limited, and later on even normal eating becomes difficult. It occurs almost exclusively in India and Indian communities living abroad. The overall prevalence of oral potentially malignant disorders in the Middle East was 2.8%. Lichen planus/lichenoid lesions were the most common lesions (1.8%) followed by leukoplakias (0.48%), chronic hyperplastic candidiosis (0.38%), and erythroplakia (0.096%).

Tobacco
In a study of Europeans, smoking and other tobacco use was associated with about 75 percent of oral cancer cases, caused by irritation of the mucous membranes of the mouth from smoke and heat of cigarettes, cigars, and pipes. Tobacco contains over 60 known carcinogens, and the combustion of it, and by-products from this process, is the primary mode of involvement. Use of chewing tobacco or snuff causes irritation from direct contact with the mucous membranes. Tobacco use in any form by itself, and even more so in combination with heavy alcohol consumption, continues to be an important risk factor for oral cancer. However, due to the current trends in the spread of HPV 16, as of early 2011 the virus is now considered the primary causative factor in 63% of newly diagnosed patients.[1]
Alcohol
Alcohol consumption is a major risk factor for certain head and neck cancers, particularly cancers of the oral cavity (excluding the lips), pharynx (throat), and larynx (voice box). People who consume 50 or more grams of alcohol per day (approximately 3.5 or more drinks per day) have at least a two to three times greater risk of developing these cancers than nondrinkers. Moreover, the risks of these cancers are substantially higher among persons who consume this amount of alcohol and also use tobacco. In its Report on carcinogens, the National Toxicology Program of the US Department of Health and Human Services lists consumption of alcoholic beverages as a known human carcinogen. The research evidence indicates that the more alcohol a person drinks—particularly the more alcohol a person drinks regularly over time—the higher his or her risk of developing an alcohol-associated cancer. Based on data from 2009, an estimated 3.5 percent of all cancer deaths in the United States (about 19,500 deaths) were alcohol related.[2]
Human Papilloma Virus
Infection with human papillomavirus (HPV), particularly type 16 (there are over 180 types), is a known risk factor and independent causative factor for oral cancer. About 70 percent of oropharyngeal cancers are caused by HPV. In the United States, more than half of cancers diagnosed in the oropharynx are linked to HPV type 16. Recent research from multiple peer-reviewed journal articles indicates that HPV16 is the primary risk factor in this new population of oral cancer victims. HPV16 (along with HPV18) is the same virus responsible for the vast majority of all cervical cancers and is the most common sexually transmitted infection in the US. Oral cancer in this group tends to favor the tonsil and tonsillar pillars, base of the tongue, and the oropharynx. Recent data suggest that individuals that come to the disease from this particular etiology have a significant survival advantage, as the disease responds better to radiation treatments than tobacco etiology disease.[3]
Hematopoietic Stem Cell Transplantation
Patients after hematopoietic stem cell transplantation (HSCT) are at a higher risk for oral squamous cell carcinoma. Post-HSCT oral cancer may have more aggressive behavior with poorer prognosis, when compared to oral cancer in non-HSCT patients. This effect is supposed to be owing to the continuous lifelong immune suppression and chronic oral graft-versus-host disease.[4]