Mitral valve prolapse echocardiography: Difference between revisions
(Created page with "__NOTOC__ {{Mitral valve prolapse}} {{CMG}} ==Overview== Two- and three-dimensional echocardiography are valuable in the diagnosis of MVP as they allow visualization of t...") |
Rim Halaby (talk | contribs) |
||
| (8 intermediate revisions by 2 users not shown) | |||
| Line 9: | Line 9: | ||
=== 2D Echo features === | === 2D Echo features === | ||
To diagnose mitral valve prolapse on 2D echocardiography, the following criteria should be fulfilled:<ref name="pmid2670319">{{cite journal| author=Perloff JK, Child JS| title=Mitral valve prolapse. Evolution and refinement of diagnostic techniques. | journal=Circulation | year= 1989 | volume= 80 | issue= 3 | pages= 710-1 | pmid=2670319 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2670319 }} </ref> | |||
# '''Movement of either leaflet more than 2 mm superiorly into the left atrium during systole in the parasternal long axis view with leaflet thickness of at least 5 mm''' | |||
# '''Movement of the point of co-aptation behind the annular plane in the apical 4 chamber view.''' | |||
Other findings on echo include enlarged LA size thick and redundant leaflets and chordae, chordal elongation, and annular dilatation. Reduced tensile strength leads to progressive elongation or rupture of chordae that usually appear as flail segments.<ref name="pmid22248324">{{cite journal| author=Guy TS, Hill AC| title=Mitral valve prolapse. | journal=Annu Rev Med | year= 2012 | volume= 63 | issue= | pages= 277-92 | pmid=22248324 | doi=10.1146/annurev-med-022811-091602 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22248324 }} </ref> | |||
=== Doppler === | === Doppler === | ||
Doppler echocardiography is important in detecting the severity of the mitral valve prolapse. Color flow mapping and CW doppler show predominantly late systolic mitral regurgitation. Severe mitral regurgitation is usually condsidered in the presence of one ore more of the following findings: <ref name="pmid22248324">{{cite journal| author=Guy TS, Hill AC| title=Mitral valve prolapse. | journal=Annu Rev Med | year= 2012 | volume= 63 | issue= | pages= 277-92 | pmid=22248324 | doi=10.1146/annurev-med-022811-091602 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22248324 }} </ref> | |||
# '''Vena contracta width >0.7 cm''' | |||
# '''Large central mitral regurgitation jet (area >40% of left atrium)''' | |||
# '''Pulmonary vein reversal''' | |||
# '''Effective regurgitant orifice >40 mm<sup>2</sup>''' | |||
# '''Regurgitant fraction >50%''' | |||
# '''Regurgitant volume >60 cc''' | |||
The proximal isovelocity surface area (PISA) method is also used to determine severity of mitral valve prolapse. PISA can usually be detected in almost all severe cases of mitral regurgitation but in only half of cases of mild regurgitation. <ref name="pmid9083972">{{cite journal| author=Yamachika S, Reid CL, Savani D, Meckel C, Paynter J, Knoll M et al.| title=Usefulness of color Doppler proximal isovelocity surface area method in quantitating valvular regurgitation. | journal=J Am Soc Echocardiogr | year= 1997 | volume= 10 | issue= 2 | pages= 159-68 | pmid=9083972 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9083972 }} </ref> | |||
=== M Mode Echocardiography === | === M Mode Echocardiography === | ||
| Line 23: | Line 36: | ||
|[[Image:MItral Valve Prolapse.jpg|thumb|450px|left|MItral Valve Prolapse.jpg M Mode]] | |[[Image:MItral Valve Prolapse.jpg|thumb|450px|left|MItral Valve Prolapse.jpg M Mode]] | ||
|- | |- | ||
|} | |||
==2008 and Incorporated 2006 ACC/AHA Guidelines for the Management of Patients with Valvular Heart Disease (DO NOT EDIT) <ref name="pmid18820172">{{cite journal |author=Bonow RO, Carabello BA, Chatterjee K, ''et al.'' |title=2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons |journal=Circulation |volume=118 |issue=15 |pages=e523–661 |year=2008 |month=October |pmid=18820172 |doi=10.1161/CIRCULATIONAHA.108.190748 |url=}}</ref>== | |||
===Asymptomatic Patients (DO NOT EDIT) <ref name="pmid18820172">{{cite journal |author=Bonow RO, Carabello BA, Chatterjee K, ''et al.'' |title=2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons |journal=Circulation |volume=118 |issue=15 |pages=e523–661 |year=2008 |month=October |pmid=18820172 |doi=10.1161/CIRCULATIONAHA.108.190748 |url=}}</ref>=== | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightGreen"|[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I]] | |||
|- | |||
| bgcolor="LightGreen"|<nowiki>"</nowiki>'''1.''' [[Echocardiography]] is indicated for the diagnosis of [[MVP]] and assessment of [[MR]], leaflet morphology, and ventricular compensation in asymptomatic patients with physical signs of [[MVP]]. ([[ACC AHA guidelines classification scheme#Level of Evidence|''Level of Evidence: B'']])<nowiki>"</nowiki> | |||
|} | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightCoral"|[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class III]] | |||
|- | |||
| bgcolor="LightCoral"|<nowiki>"</nowiki>'''1.''' [[Echocardiography]] is not indicated to exclude [[MVP]] in asymptomatic patients with ill-defined symptoms in the absence of a constellation of clinical symptoms or physical findings suggestive of [[MVP]] or a positive family history. ([[ACC AHA guidelines classification scheme#Level of Evidence|''Level of Evidence: B'']])<nowiki>"</nowiki> | |||
|- | |||
| bgcolor="LightCoral"|<nowiki>"</nowiki>'''2.''' Routine repetition of [[echocardiography]] is not indicated for the asymptomatic patient who has [[MVP]] and no [[MR]] or [[MVP]] and mild [[MR]] with no changes in clinical signs or symptoms. ([[ACC AHA guidelines classification scheme#Level of Evidence|''Level of Evidence: C'']])<nowiki>"</nowiki> | |||
|} | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LemonChiffon"|[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class IIa]] | |||
|- | |||
| bgcolor="LemonChiffon"|<nowiki>"</nowiki>'''1.''' [[Echocardiography]] can effectively exclude [[MVP]] in asymptomatic patients who have been diagnosed without clinical evidence to support the diagnosis. ([[ACC AHA guidelines classification scheme#Level of Evidence|''Level of Evidence: C'']])<nowiki>"</nowiki> | |||
|- | |||
| bgcolor="LemonChiffon"|<nowiki>"</nowiki>'''2.''' [[Echocardiography]] can be effective for risk stratification in asymptomatic patients with physical signs of [[MVP]] or known [[MVP]]. ([[ACC AHA guidelines classification scheme#Level of Evidence|''Level of Evidence: C'']])<nowiki>"</nowiki> | |||
|} | |} | ||
Latest revision as of 02:34, 8 November 2013
|
Mitral valve prolapse Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Mitral valve prolapse echocardiography On the Web |
|
American Roentgen Ray Society Images of Mitral valve prolapse echocardiography |
|
Risk calculators and risk factors for Mitral valve prolapse echocardiography |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Two- and three-dimensional echocardiography are valuable in the diagnosis of MVP as they allow visualization of the mitral leaflets relative to the mitral annulus. This allows measurement of the leaflet thickness and their displacement relative to the annulus. Thickening of the mitral leaflets >5 mm and leaflet displacement >2 mm indicates classic mitral valve prolapse.
Echocardiography
2D Echo features
To diagnose mitral valve prolapse on 2D echocardiography, the following criteria should be fulfilled:[1]
- Movement of either leaflet more than 2 mm superiorly into the left atrium during systole in the parasternal long axis view with leaflet thickness of at least 5 mm
- Movement of the point of co-aptation behind the annular plane in the apical 4 chamber view.
Other findings on echo include enlarged LA size thick and redundant leaflets and chordae, chordal elongation, and annular dilatation. Reduced tensile strength leads to progressive elongation or rupture of chordae that usually appear as flail segments.[2]
Doppler
Doppler echocardiography is important in detecting the severity of the mitral valve prolapse. Color flow mapping and CW doppler show predominantly late systolic mitral regurgitation. Severe mitral regurgitation is usually condsidered in the presence of one ore more of the following findings: [2]
- Vena contracta width >0.7 cm
- Large central mitral regurgitation jet (area >40% of left atrium)
- Pulmonary vein reversal
- Effective regurgitant orifice >40 mm2
- Regurgitant fraction >50%
- Regurgitant volume >60 cc
The proximal isovelocity surface area (PISA) method is also used to determine severity of mitral valve prolapse. PISA can usually be detected in almost all severe cases of mitral regurgitation but in only half of cases of mild regurgitation. [3]
M Mode Echocardiography
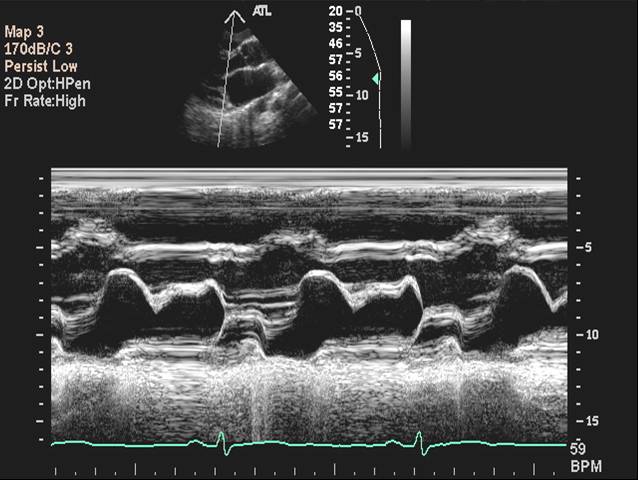 |
2008 and Incorporated 2006 ACC/AHA Guidelines for the Management of Patients with Valvular Heart Disease (DO NOT EDIT) [4]
Asymptomatic Patients (DO NOT EDIT) [4]
| Class I |
| "1. Echocardiography is indicated for the diagnosis of MVP and assessment of MR, leaflet morphology, and ventricular compensation in asymptomatic patients with physical signs of MVP. (Level of Evidence: B)" |
| Class III |
| "1. Echocardiography is not indicated to exclude MVP in asymptomatic patients with ill-defined symptoms in the absence of a constellation of clinical symptoms or physical findings suggestive of MVP or a positive family history. (Level of Evidence: B)" |
| "2. Routine repetition of echocardiography is not indicated for the asymptomatic patient who has MVP and no MR or MVP and mild MR with no changes in clinical signs or symptoms. (Level of Evidence: C)" |
| Class IIa |
| "1. Echocardiography can effectively exclude MVP in asymptomatic patients who have been diagnosed without clinical evidence to support the diagnosis. (Level of Evidence: C)" |
| "2. Echocardiography can be effective for risk stratification in asymptomatic patients with physical signs of MVP or known MVP. (Level of Evidence: C)" |
References
- ↑ Perloff JK, Child JS (1989). "Mitral valve prolapse. Evolution and refinement of diagnostic techniques". Circulation. 80 (3): 710–1. PMID 2670319.
- ↑ 2.0 2.1 Guy TS, Hill AC (2012). "Mitral valve prolapse". Annu Rev Med. 63: 277–92. doi:10.1146/annurev-med-022811-091602. PMID 22248324.
- ↑ Yamachika S, Reid CL, Savani D, Meckel C, Paynter J, Knoll M; et al. (1997). "Usefulness of color Doppler proximal isovelocity surface area method in quantitating valvular regurgitation". J Am Soc Echocardiogr. 10 (2): 159–68. PMID 9083972.
- ↑ 4.0 4.1 Bonow RO, Carabello BA, Chatterjee K; et al. (2008). "2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons". Circulation. 118 (15): e523–661. doi:10.1161/CIRCULATIONAHA.108.190748. PMID 18820172. Unknown parameter
|month=ignored (help)