Membranous glomerulonephritis pathophysiology: Difference between revisions
No edit summary |
Sunny Kumar (talk | contribs) |
||
| Line 28: | Line 28: | ||
OR | OR | ||
Membranous nephropathy (MN) is a common cause of nephrotic syndrome in adults | |||
==Pathophysiology== | ==Pathophysiology== | ||
MGN is caused by circulating [[immune complex]]. Current research indicates that the majority of the immune complexes are formed via binding of antibodies to antigens ''in situ'' to the glomerular basement membrane. The said antigens may be [[endogenous]] to (from) the basement membrane, or "planted" from systemic circulation. | MGN is caused by circulating [[immune complex]]. Current research indicates that the majority of the immune complexes are formed via binding of antibodies to antigens ''in situ'' to the glomerular basement membrane. The said antigens may be [[endogenous]] to (from) the basement membrane, or "planted" from systemic circulation. | ||
Revision as of 15:50, 2 May 2018
|
Membranous glomerulonephritis Microchapters |
|
Differentiating Membranous glomerulonephritis from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Membranous glomerulonephritis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Membranous glomerulonephritis pathophysiology |
|
Directions to Hospitals Treating Membranous glomerulonephritis |
|
Risk calculators and risk factors for Membranous glomerulonephritis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief:
Overview
The exact pathogenesis of [disease name] is not fully understood.
OR
It is thought that [disease name] is the result of / is mediated by / is produced by / is caused by either [hypothesis 1], [hypothesis 2], or [hypothesis 3].
OR
[Pathogen name] is usually transmitted via the [transmission route] route to the human host.
OR
Following transmission/ingestion, the [pathogen] uses the [entry site] to invade the [cell name] cell.
OR
[Disease or malignancy name] arises from [cell name]s, which are [cell type] cells that are normally involved in [function of cells].
OR
The progression to [disease name] usually involves the [molecular pathway].
OR
Membranous nephropathy (MN) is a common cause of nephrotic syndrome in adults
Pathophysiology
MGN is caused by circulating immune complex. Current research indicates that the majority of the immune complexes are formed via binding of antibodies to antigens in situ to the glomerular basement membrane. The said antigens may be endogenous to (from) the basement membrane, or "planted" from systemic circulation.
The immune complex serves as an activator that triggers a response from the C5b - C9 complements, which form a membrane attack complex (MAC) on the glomerular epithelial cells. This, in turn, stimulates release of proteases and oxidants by the mesangial and epithelial cells, damaging the capillary walls and causing them to become "leaky". In addition, the epithelial cells also seem to secrete an unknown mediator that reduces nephrin synthesis and distribution.
Morphology
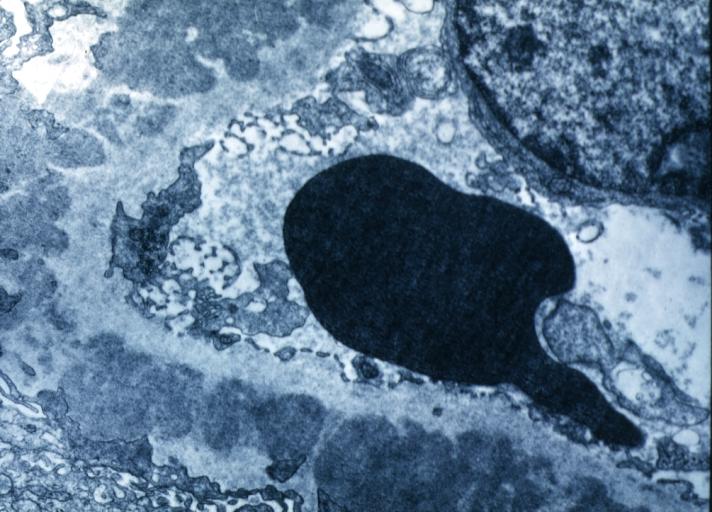
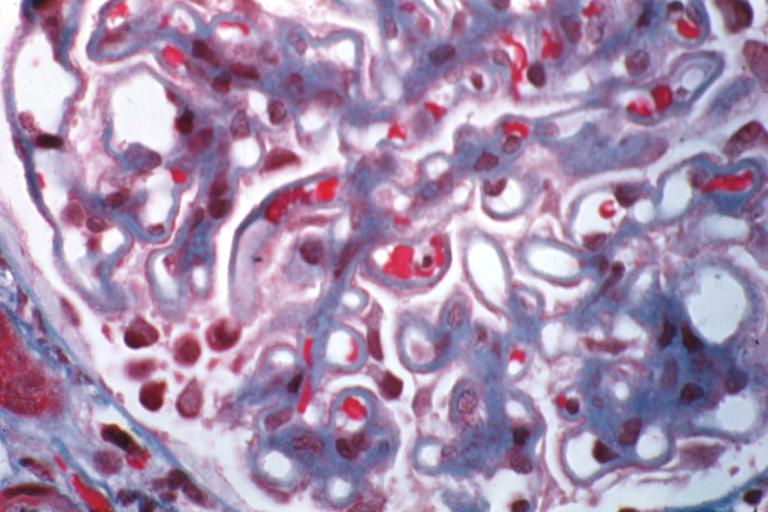
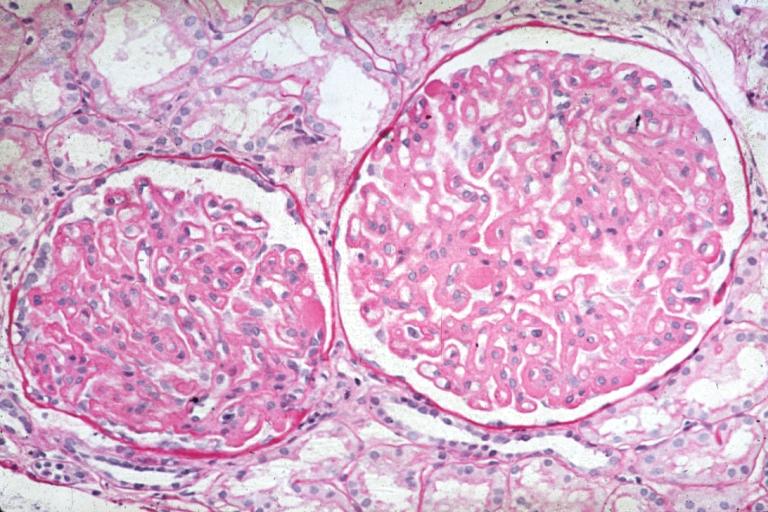
The defining point of MGN is the presence of subepithelial immunoglobulin-containing deposits along the glomerular basement membrane (GBM). By light microscopy, the basement membrane is observed to be diffusively thickened. Using Jones' stain, the GBM appears to have a "spiked" or "holey" appearance. On electron microscopy, subepithelial deposits that nestle against the glomerular basement membrane seems to be the cause of the thickening. Also, the podocytes lose their foot processes.
As the disease progresses, the deposits will eventually be cleared, leaving cavities in the basement membrane. These cavities will later be filled with basement membrane-like material, and if the disease continues even further, the glomeruli will become sclerosed and finally hyalinized.
Immunoflourescence microscopy will reveal typical granular deposition of immunoglobulins and complement along the basement membrane.
Pathological Findings
Pathogenesis
- The exact pathogenesis of [disease name] is not fully understood.
OR
- It is understood that [disease name] is the result of / is mediated by / is produced by / is caused by either [hypothesis 1], [hypothesis 2], or [hypothesis 3].
- [Pathogen name] is usually transmitted via the [transmission route] route to the human host.
- Following transmission/ingestion, the [pathogen] uses the [entry site] to invade the [cell name] cell.
- [Disease or malignancy name] arises from [cell name]s, which are [cell type] cells that are normally involved in [function of cells].
- The progression to [disease name] usually involves the [molecular pathway].
- The pathophysiology of [disease/malignancy] depends on the histological subtype.
Genetics
- [Disease name] is transmitted in [mode of genetic transmission] pattern.
- Genes involved in the pathogenesis of [disease name] include [gene1], [gene2], and [gene3].
- The development of [disease name] is the result of multiple genetic mutations.
Associated Conditions
Gross Pathology
- On gross pathology, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
Microscopic Pathology
- On microscopic histopathological analysis, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
References
-
Membranous Glomerulonephritis: Electron micrography. An excellent example to show thickened basement membrane and immune complexes.
-
Membranous Glomerulonephritis: Micro trichrome high mag excellent to show thickened capillary basement membranes
-
Membranous Glomerulonephritis: Micro PAS high mag excellent example of this lesion
-
Membranous Glomerulonephritis: Micro PAS med mag