Lymphoplasmacytic lymphoma MRI
|
Lymphoplasmacytic lymphoma Microchapters |
|
Differentiating Lymphoplasmacytic Lymphoma from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Lymphoplasmacytic lymphoma MRI On the Web |
|
American Roentgen Ray Society Images of Lymphoplasmacytic lymphoma MRI |
|
Risk calculators and risk factors for Lymphoplasmacytic lymphoma MRI |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sara Mohsin, M.D.[2]
Overview
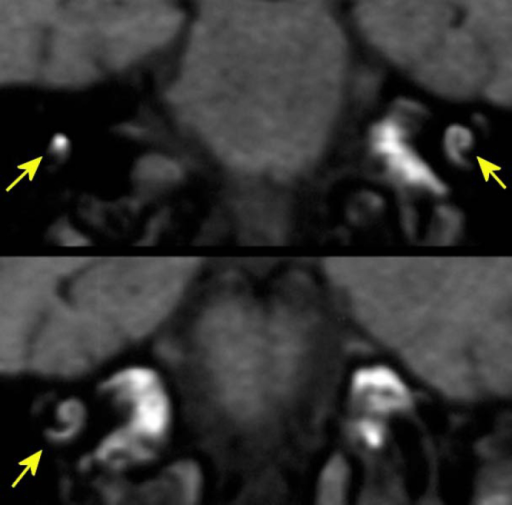
There are no specific MRI findings associated with Waldenström macroglobulinemia.
MRI
There are no specific MRI findings associated with Waldenström macroglobulinemia. However, MRI of the brain, spinal cord and orbits is important when assessing for hyperviscosity in the presence of high IgM paraprotein in the blood especially important when diagnosing Bing-Neel syndrome.[1][2][3]
 |
 |
 |
References
- ↑ O'Neil DS, Francescone MA, Khan K, Bachir A, O'Connor OA, Sawas A (2018). "A Case of Bing-Neel Syndrome Successfully Treated with Ibrutinib". Case Rep Hematol. 2018: 8573105. doi:10.1155/2018/8573105. PMC 6136466. PMID 30228918.
- ↑ Minnema MC, Kimby E, D'Sa S, Fornecker LM, Poulain S, Snijders TJ; et al. (2017). "Guideline for the diagnosis, treatment and response criteria for Bing-Neel syndrome". Haematologica. 102 (1): 43–51. doi:10.3324/haematol.2016.147728. PMC 5210231. PMID 27758817.
- ↑ Tallant A, Selig D, Wanko SO, Roswarski J (2018). "First-line ibrutinib for Bing-Neel syndrome". BMJ Case Rep. 2018. doi:10.1136/bcr-2018-226102. PMID 30279255.