|
|
| (100 intermediate revisions by 5 users not shown) |
| Line 1: |
Line 1: |
| {{Taxobox | color = lightgrey | | __NOTOC__ |
| | name = ''Listeria monocytogenes'' | | {{Listeriosis}} |
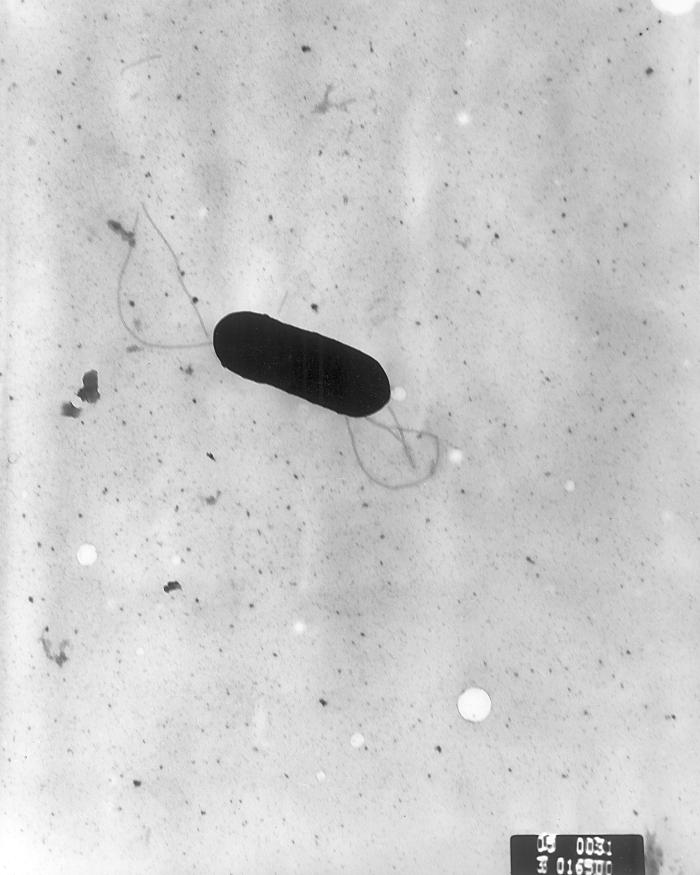
| | image = Listeria monocytogenes PHIL 2287 lores.jpg | | {{Taxobox |
| | | color = lightgrey <!-- Please read [[WP:Taxobox usage#Color]] before making any changes to the taxobox color. --> |
| | | name = ''Listeria'' |
| | | image =Listeria monocytogenes PHIL 2287 lores.jpg |
| | image_width = 240px | | | image_width = 240px |
| | regnum = [[Bacteria]] | | | image_caption = [[Scanning electron microscope|Scanning electron micrograph]] of ''Listeria monocytogenes''. |
| | | regnum = [[Bacterium|Bacteria]] |
| | divisio = [[Firmicutes]] | | | divisio = [[Firmicutes]] |
| | classis = [[Bacilli]] | | | classis = [[Bacilli]] |
| | ordo = [[Bacillales]] | | | ordo = [[Bacillales]] |
| | familia = [[Listeriaceae]] | | | familia = [[Listeriaceae]] |
| | genus = ''[[Listeria]]'' | | | genus = ''Listeria'' |
| | species = '''''L. monocytogenes''''' | | | genus_authority = [[Harvey Pirie|Pirie]] 1940 |
| | binomial = ''Listeria monocytogenes'' | | | subdivision_ranks = Species |
| | binomial_authority = Murray ''et al.'' (1926)
| | | subdivision = |
| | ''[[Listeria fleischmannii|L. fleischmannii]]''<br /> |
| | ''[[Listeria grayi|L. grayi]]''<br /> |
| | ''[[Listeria innocua|L. innocua]]''<br /> |
| | ''[[Listeria ivanovii|L. ivanovii]]''<br /> |
| | ''[[Listeria marthii|L. marthii]]''<br /> |
| | ''[[Listeria monocytogenes|L. monocytogenes]]''<br /> |
| | ''[[Listeria rocourtiae|L. rocourtiae]]''<br /> |
| | ''[[Listeria seeligeri|L. seeligeri]]''<br /> |
| | ''[[Listeria weihenstephanensis|L. weihenstephanensis]]''<br /> |
| | ''[[Listeria welshimeri|L. welshimeri]]'' |
| }} | | }} |
| __NOTOC__
| | {{About0|Listeriosis}} |
| {{SI}} | |
| | |
| {{Main|Listeriosis}}
| |
| | |
| {{CMG}}; {{AE}} {{JS}} | | {{CMG}}; {{AE}} {{JS}} |
|
| |
|
| ==Overview== | | ==Overview== |
| | Listeriosis is caused by the bacterium ''Listeria monocytogenes'', a flagellated, [[catalase-positive]], facultative [[intracellular]], [[anaerobe|anaerobic]], [[spore|nonsporulating]], [[Gram-positive]] [[bacillus]]. ''Listeria'' is commonly found in soil, water, vegetation and fecal material.<ref name=WHO>{{cite web | title = Risk assessment of Listeria monocytogenes in ready-to-eat foods | url = http://whqlibdoc.who.int/publications/2004/9241562625_part1.pdf }}</ref> |
|
| |
|
| '''''Listeria monocytogenes''''' is a [[Gram-positive]] [[bacterium]], in the division [[Firmicutes]], named for [[Joseph Lister]]. [[Motility|Motile]] via [[flagella]], ''L. monocytogenes'' can move within [[Eukaryote|eukaryotic]] cells by explosive [[polymerization]] of [[actin]] filaments (known as ''[[comet tails]]'' or ''[[actin rockets]]'').
| | ==Cause== |
| | | *Listeriosis is caused by the bacterium ''Listeria spp''. |
| Studies suggest that up to 10% of human [[gastrointestinal tract]]s may be colonized by ''L. monocytogenes''.
| | *''Listeria monocytogenes'' is the most common species associated with development of listeriosis. |
| | | *The genus ''Listeria'' contains ten species: |
| ==Clinical Manifestations== | | :*''L. fleischmannii'' |
| | | :*''L. grayi'' |
| '''''Listeria monocytogenes''''' is known for causing disease particularly in immunosuppressed patients, neonates, elderly, pregnant women and occasionally in healthy individuals. It has an [[incubation period]] which can range from a median of 24 hours, in ''Listeria''[[gastroenteritis]], to a median of 35 days, in ''Listeria'' invasive disease.
| | :*''L. innocua'' |
| The infection with ''Listeria monocytogenes'' is more common to occur during the summer and may present as a '''''self-limited febrile [[gastroenteritis]]''''', in normal adult hosts, after ingesting a high number of organisms in food, or as an '''''invasive disease'''''.
| | :*''L. ivanovii'' |
| | | :*''L. marthii'' |
| ===Febrile Gastroenteritis===
| | :*''L. monocytogenes'' |
| | | :*''L. rocourtiae'' |
| Febrile [[gastroenteritis]] accounts for less than 1% of reported bacterial food-born infections, occurring usually after ingestion of a large inoculum of bacteria from contaminated foods. It might present as:
| | :*''L. seeligeri'' |
| *fever
| | :*''L. weihenstephanensis'' |
| *watery diarrhea
| | :*''L. welshimeri'' |
| *[[nausea]]
| |
| *[[vomiting]]
| |
| *headache
| |
| *[[arthralgia|joint]] and [[myalgia|muscle pain]]
| |
| It generally lasts for 2 days and the patient experiences complete recovery from the symptoms. Some patients may be asymptomatic for the disease, whilst others, immunocompromised, pregnant women and elder patients, in rare cases, present with invasive infection.
| |
| | |
| ===Infection in Pregnancy===
| |
| Occurs more frequently during the third trimester of gestation, presenting most commonly with flu-like symptoms, such as:
| |
| *[[fever]]
| |
| *chills
| |
| *back pain
| |
| The infection may be mild and the diagnosis missed, if [[blood cultures]] are not obtained. Since [[bacteremia]], with no CNS involvement is common rule in pregnant women with [[listeriosis]], [[blood cultures]] should always be obtained in pregnant women who present with [[fever]], with no other alternative cause, such as [[UTI]] or [[pharyngitis]].
| |
| | |
| [[Listeriosis]], in pregnant women, can result in:
| |
| *fetal death
| |
| *premature birth
| |
| *infected newborns | |
| The newborn also has great risk of developing [[granulomatosis]] infantiseptica, a severe ''in utero'' infection resulting from transplacental transmission, in which infants may present with: | |
| *disseminated [[abscesses]] | |
| *[[granulomas]] in multiple internal organs ([[brain]], [[lungs]], [[liver]], [[spleen]] and [[kidneys]])
| |
| *papular or ulcerative skin lesions.
| |
| *most infants with this disease are stillborn or die soon after birth.
| |
| | |
| ===Sepsis of Unknown Origin===
| |
| Occurs in patients of all ages. Neonates usually tend to acquire the infection during or after birth. When this occurs during the first week of life, usually manifests as [[sepsis]], while after this first week, it tends to have more variable manifestations, such as [[meningitis]]. Early onset of sepsis is associated with higher neonatal mortality.
| |
| | |
| *''Listeria [[meningoencephalitis]]'' is more common in neonates after 3 days of age, as well as in immunocompromised and elderly adults. | |
| *Adults presenting ''Listeria [[sepsis]]'', are most commonly immunocompromised or elderly, and typically present with fever and chills. [[Septic shock]] can occur with [[brain]] and/or [[meningeal]] involvement, leading to [[meningoencephalitis]] or [[cerebritis]]. | |
| | |
| ===CNS Infection===
| |
| [[Central Nervous System]] [[infection]] most commonly manifests by [[meningoencephalitis]], while [[cerebritis]], which usually progresses into [[brain abscess]] and [[rhombencephalitis]], is a less common manifestation.
| |
| | |
| '''1. Meningoencephalitis''' | |
| Occurs more frequently in neonates after 3 days of age and in [[immunocompromised]] and elderly patients. The clinical presentation can range from mild fever and mental status changes, to a more aggressive course with [[coma]]. There may also be an [[encephalic]] component present,which will present with focal [[neurological]] signs, such as:
| |
| *[[Cranial nerve]] abnormalities | |
| *[[Ataxia]]
| |
| *Tremors
| |
| *[[Hemiplegia]]
| |
| *[[Deafness]]
| |
| *[[Seizures]]
| |
| | |
| '''2. Cerebritis''' | |
| Results from direct hematogenous invasion of [[cerebral]] [[parenchyma]], with or without [[meningeal]] involvement. It rarely progresses to [[brain abscess]], and may occur alongside [[meningitis]] in the same patient.
| |
| It may manifest with:
| |
| *[[Fever]]
| |
| *[[Headache]]
| |
| *[[Hemiplegia]] | |
| | |
| '''3. Rhombencephalitis''' | |
| Rare manifestation of CNS infection, which affects more commonly healthy individuals through the ingestion of ''Listeria'' contaminated food, often in outbreaks. Rhombencephalitis often follows a biphasic course, beginning with:
| |
| *[[Headache]]
| |
| | |
| *[[Fever]]
| |
| | |
| *[[Nausea]]
| |
| | |
| *[[Vomiting]]
| |
| | |
| Which, within several days is followed by:
| |
| *[[Cranial nerve]] [[palsies]]
| |
| | |
| *[[Ataxia]]
| |
| | |
| *[[Tremor]]
| |
| | |
| *Decreased [[consciousness]]
| |
| | |
| *[[Seizures]]
| |
| | |
| *[[Hemiparesis]]
| |
| | |
| *[[Respiratory failure]] | |
| | |
| Despite the fact of ''Listeria'' being the most common [[infectious]] cause of rhombencephalitis, it must be distinguished from other [[infectious]] etiologies, such as:
| |
| *''[[Herpes simplex]]'' [[encephalities]] | |
| *[[Tuberculosis]]
| |
| *[[Toxoplasmosis]]
| |
| *[[Cryptococcosis]]
| |
| *[[Lyme disease]]
| |
| *''[[Epstein-Barr virus]]'' | |
| *[[Brucellosis]]
| |
| *[[JC virus]]
| |
| There are also noninfectious conditions which may cause brainstem and/or cerebral lesions, such as:
| |
| *[[Multiple sclerosis]]
| |
| *[[Sarcoidosis]]
| |
| *Systemic [[rheumatic diseases]]
| |
| *[[Lymphoma]]
| |
| *[[Paraneoplastic syndrome]]
| |
|
| |
|
| The diagnosis of [[rhombencephalitis]] can be delayed by the fact that [[CSF]] analysis often reveals only mild abnormalities, and may be demonstrated by [[Magnetic resonance]].1
| | *Of note, ''Listeria dinitrificans'' was previously thought to be part of the ''Listeria'' genus, but it has been reclassified into the new genus ''[[Jonesia]]''.<ref name=collins>M. D. Collins, S. Wallbanks, D. J. Lane, J. Shah, R. Nietupskin, J. Smida, M. Dorsch and E. Stackebrandt. Phylogenetic Analysis of the Genus ''Listeria'' Based on Reverse Transcriptase Sequencing of 16S rRNA. International Journal of Systematic and Evolutionary Microbiology. April 1991 vol. 41 no. 2 240–246</ref> |
|
| |
|
| ===Focal infections=== | | ==Taxonomy== |
| Most focal infections have no specific characteristics, but do share a moat common host, the [[immunocompromised]] patients. These might include:
| | [[Bacteria]]; [[Firmicutes]]; [[Bacilli]]; [[Bacillales]]; [[Listeriaceae]]; [[Listeria]]; [[Listeria monocytogenes]]. |
| *[[Skin]] or [[eye]] [[infections]]
| |
|
| |
|
| *Oculoglandular syndrome, [[pneumonia]], [[empyema]], [[myocarditis]], [[lymphadenitis]], [[septic arthritis]], [[osteomyelitis]] and [[necrotizing fasciitis]]. | | ==Microbiological Characteristics== |
| | *''Listeria monocytogenes'' is a flagellated, [[catalase-positive]], facultative [[intracellular]], [[anaerobe|anaerobic]], [[spore|nonsporulating]], [[Gram-positive]] [[bacillus]]. |
|
| |
|
| *[[Brain|Brain abscess]] and [[spinal]] [[abscesses]], as well as [[cholecystitis]], resulting from hematogenous dissemination. | | ==Natural Reservoir== |
| *[[Acute hepatitis]], simulating [[viral hepatitis]], seen in patients with disseminated infections.
| | *In the environment, ''Listeria monocytogenes'' is commonly found in soil, water, vegetation and fecal material. |
| *[[Peritonitis]], seen in [[cirrhosis]] and continuous ambulatory peritoneal [[dialysis]] patients. | | *Animals may be asymptomatic carriers of ''Listeria''.<ref name=WHO>{{cite web | title = Risk assessment of Listeria monocytogenes in ready-to-eat foods | url = http://whqlibdoc.who.int/publications/2004/9241562625_part1.pdf }}</ref> |
| | *''L. monocytogenes'' has been associated with foods such as raw [[milk]], pasteurized fluid milk, [[cheese]]s (particularly soft-ripened varieties), [[ice cream]], raw [[vegetables]], fermented raw-meat sausages, raw and cooked [[poultry]], raw meats, and raw and smoked [[fish]].<ref name=Fleming_1985>Fleming, D. W., S. L. Cochi, K. L. MacDonald, J. Brondum, P. S. Hayes, B. D. Plikaytis, M. B. Holmes, A. Audurier, C. V. Broome, and A. L. Reingold. 1985. Pasteurized milk as a vehicle of infection in an outbreak of listeriosis. N. Engl. J. Med. 312:404-407.</ref> |
| | *''Listeria'' has the ability to grow at temperatures as low as 0°C, allows its multiplication in refrigerated foods. At refrigerated temperature such as 4°C, the amount of ferric iron in the environment promotes the growth of ''L. monocytogenes''.<ref name=Dworaczek_Kubo_Dykes_2002>Dykes, G. A., Dworaczek (Kubo), M. 2002. Influence of interactions between temperature, ferric ammonium citrate and glycine betaine on the growth of ''Listeria monocytogenes'' in a defined medium. Lett Appl Microbiol. 35(6):538-42.</ref> |
|
| |
|
| ==Diagnosis== | | ==Gallery== |
| The diagnosis of infection by ''[[Listeria monocytogenes]]'' may be suspected from the clinical findings, however due to the similarities with other [[infectious diseases]], it can be mistaken with those. Therefore, the diagnosis should be established by culture of the organism from [[blood culture|blood]] and [[CSF]]. In many reported cases, despite the presence of the disease, [[CSF]] cultures were negative, in which cases, blood cultures should orient the diagnosis, since these are more commonly positive than the first ones.<ref name="pmid8507761">{{cite journal| author=Armstrong RW, Fung PC| title=Brainstem encephalitis (rhombencephalitis) due to Listeria monocytogenes: case report and review. | journal=Clin Infect Dis | year= 1993 | volume= 16 | issue= 5 | pages= 689-702 | pmid=8507761 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8507761 }} </ref>
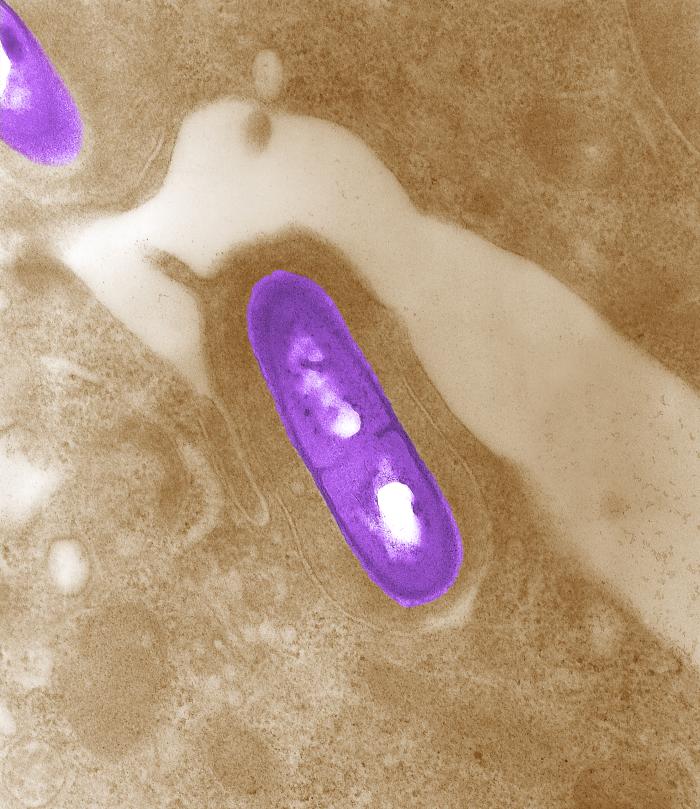
| | [[Image:Listeria2.jpg|thumb|none| Electron micrograph of a Listeria bacterium in tissue.<SMALL><SMALL>''[http://phil.cdc.gov/phil/ Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.]''<ref name="PHIL">{{Cite web | title = Public Health Image Library (PHIL), Centers for Disease Control and Prevention | url = http://phil.cdc.gov/phil/}}</ref></SMALL></SMALL>]] |
| | |
| *'''CSF analysis''' often shows:
| |
| **[[Pleocytosis]]
| |
| **More than 25 [[lymphocytes]] in [[CSF]] [[Differential blood count (patient information)|differential count]], without [[antibiotic]] therapy.
| |
| **Moderately elevated [[CSF]] [[protein]] concentration with reduced [[CSF]] [[glucose]] concentration.<ref name="pmid9772921">{{cite journal| author=Mylonakis E, Hohmann EL, Calderwood SB| title=Central nervous system infection with Listeria monocytogenes. 33 years' experience at a general hospital and review of 776 episodes from the literature. | journal=Medicine (Baltimore) | year= 1998 | volume= 77 | issue= 5 | pages= 313-36 | pmid=9772921 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9772921 }} </ref>
| |
| ** [[Gram stain]] of the [[CSF]] has very low [[sensitivity]] and even when organisms are seen, they may be misidentified. <ref name="pmid4998254">{{cite journal| author=Lavetter A, Leedom JM, Mathies AW, Ivler D, Wehrle PF| title=Meningitis due to Listeria monocytogenes. A review of 25 cases. | journal=N Engl J Med | year= 1971 | volume= 285 | issue= 11 | pages= 598-603 | pmid=4998254 | doi=10.1056/NEJM197109092851103 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=4998254 }} </ref> Therefore, ''Listeria monocytogenes'' should always be considered when similar organisms are growing in [[blood culture |blood]] or [[CFS]] cultures. The presumptive diagnosis of [[viral meningitis]] should also be carefully considered in [[immunocompromised]], chronically ill, or elderly patients, presenting with acute [[meningitis]] and a negative [[Gram stain]]. Due to the fact that [[rhombencephalitis]] patients [[CSF]] examination often reveals only mild abnormalities, its diagnosis is often delayed.
| |
| **A [[Polymerase chain reaction]] assay has been developed for the ''hly gene'' detection, which encodes for the ''listeriolysin O'', in [[CSF]] cultures. However, despite more [[Specificity|specific]] and more [[sensitivity|sensitive]], it is not commercially available yet.
| |
| *'''[[Stool cultures]]''' for ''Listeria'' are not indicated in systemic [[listeriosis]] patients, since routine culture media for enteric [[pathogens]] are not appropriate for the growth of ''Listeria''. However, in cases of outbreaks of [[listeriosis]] or individual patients with suspected ''Listeria'' [[gastroenteritis]], special selected media can be used. The special culture media may be suggested by a local [[microbiology]] laboratory, a state health department or the [[CDC]].
| |
| | |
| *'''Imaging studies'''
| |
| Although both MRI and CT scan may be used to help in the diagnosis of ''Listeria monocytogenes'' lesions, the MRI is a more [[sensitivity|sensitive]] method to detect ''Listeria'' lesions in the cerebellum, brainstem and cortex.<ref name="pmid8507761">{{cite journal| author=Armstrong RW, Fung PC| title=Brainstem encephalitis (rhombencephalitis) due to Listeria monocytogenes: case report and review. | journal=Clin Infect Dis | year= 1993 | volume= 16 | issue= 5 | pages= 689-702 | pmid=8507761 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8507761 }} </ref> On an [[MRI]], in the [[cerebral]] [[parenchyma]] there may be identified high-signal lesions on T2-weighted images and enhancing lesions on T1-weighted images, following administration of IV contrast.
| |
| Since MRI evidence of brainstem involvement coupled with proper clinical setting, is strongly suggestive of infection by ''Lysteria'', it is recommending the use of contrast [[MRI]] in all patients presenting with ''Listeria'' [[meningitis]], ''Listeria'' [[bacteremia]], [[CNS]] signs and symptoms or suspicion of intracranial [[listeriosis]].
| |
| | |
| ==Pathogenesis==
| |
| [[Infection]] by ''L. monocytogenes'' causes the disease [[listeriosis]]. The manifestations of listeriosis include [[septicemia]]<ref name=Gray_1966>Gray, M. L., and A. H. Killinger. 1966. Listeria monocytogenes and listeric infection. Bacteriol. Rev. 30:309-382.</ref>, [[meningitis]] (or [[meningoencephalitis]])<ref name=Gray_1966/>, [[encephalitis]]<ref name=Armstrong1993>Armstrong, R. W., and P. C. Fung. 1993. Brainstem encephalitis (Rhombencephalitis) due to Listeria monocytogenes: case report and review. Clin. Infect. Dis. 16:689-702.</ref>, corneal ulcer<ref name=Holland_1987>Holland, S., E. Alfonso, H. Gelender, D. Heidemann, A. Mendelsohn, S. Ullman, and D. Miller. 1987. Corneal ulcer due to Listeria monocytogenes. Cornea 6:144-146.</ref>, Pneumonia<ref name=whitelock_1989>Whitelock-Jones, L., J. Carswell, and K. C. Rassmussen. 1989. Listeria pneumonia. A case report. South African Medical Journal 75:188-189.</ref>, and [[uterus|intrauterine]] or [[cervix|cervical]] infections in pregnant women, which may result in [[miscarriage|spontaneous abortion]] (2nd/3rd trimester) or [[stillbirth]]. Surviving neonates of Fetomaternal Listeriosis may suffer granulomatosis infantiseptica - [[pyogenic]] [[granulomas]] distributed over the whole body, and may suffer from physical retardation. [[Influenza]]-like symptoms, including persistent fever, usually precede the onset of the aforementioned disorders. Gastrointestinal symptoms such as nausea, vomiting, and [[diarrhea]] may precede more serious forms of listeriosis or may be the only symptoms expressed. Gastrointestinal symptoms were epidemiologically associated with use of [[antacid]]s or [[cimetidine]]. The onset time to serious forms of listeriosis is unknown but may range from a few days to three weeks. The onset time to gastrointestinal symptoms is unknown but probably exceeds 12 hours. An early study suggeseted that ''L. monocytogenes'' was unique among [[Gram-positive]] bacteria in that it possessed [[lipopolysaccharide]]<ref name=Wexler_1979>Wexler, H., and J. D. Oppenheim. 1979. Isolation, characterization, and biological properties of an endotoxin-like material from the gram-positive organism Listeria monocytogenes. Infect. Immun. 23:845-857.</ref>, which served as an [[endotoxin]]. A later study did not support these findings<ref name=Maitra_1986> SHYAMAL K. MAITRA,RONALD NACHUM, AND FREDERICK C. PEARSON. 1986. Establishment of Beta-Hydroxy Fatty Acids as Chemical Marker Molecules for Bacterial Endotoxin by Gas Chromatography-Mass
| |
| Spectrometry. APPLIED AND ENVIRONMENTAL MICROBIOLOGY, Sept. 1986, p. 510-514</ref>.
| |
| | |
| The infective dose of ''L. monocytogenes'' varies with the strain and with the susceptibility of the victim. From cases contracted through raw or supposedly pasteurized milk, one may safely assume that in susceptible persons, fewer than 1,000 total organisms may cause disease. ''L. monocytogenes'' may invade the gastrointestinal epithelium. Once the bacterium enters the host's [[monocyte]]s, [[macrophage]]s, or [[polymorphonuclear leukocyte]]s, it becomes blood-borne (septicemic) and can grow. Its presence intracellularly in [[phagocytosis|phagocytic]] cells also permits access to the brain and probably transplacental migration to the fetus in pregnant women. The pathogenesis of ''L. monocytogenes'' centers on its ability to survive and multiply in phagocytic host cells.
| |
| | |
| == Treatment ==
| |
| When listeric meningitis occurs, the overall [[death|mortality]] may reach 70%; from septicemia 50%, from perinatal/neonatal infections greater than 80%. In infections during pregnancy, the mother usually survives. Reports of successful treatment with parenteral [[penicillin]] or [[ampicillin]] exist. [[Trimethoprim-sulfamethoxazole]] has been shown effective in patients allergic to penicillin.
| |
| | |
| Bacteriophage treatments have been developed by several companies. EBI Food Safety and Intralytix both have products suitable for treatment of the bacteria. The [[FDA]] of the United States approved a cocktail of six [[bacteriophage]]s from Intralytix, and a one type phage product from EBI Food Safety designed to kill the bacteria ''L. monocytogenes''. Uses would potentially include spraying it on fruits and ready-to-eat meat such as sliced ham and turkey.
| |
| | |
| === Gene Therapy ===
| |
| ''L. monocytogenes'' has been used in studies to deliver genes in vitro. However transfection efficiency remains poor.
| |
| | |
| ==Detection==
| |
| [[Image:LSA.jpg|left|thumb|200px|Colonies of typical ''Listeria monocytogenes'' as they appear when grown on Listeria selective [[agar]]]]
| |
| | |
| The methods for analysis of food are complex and time-consuming. The present [[Food and Drug Administration]] (FDA) method, revised in September, [[1990]], requires 24 and 48 hours of enrichment, followed by a variety of other tests. Total time to identification takes from 5 to 7 days, but the announcement of specific nonradiolabled [[DNA probes]] should soon allow a simpler and faster confirmation of suspect isolates.
| |
| | |
| Recombinant DNA technology may even permit 2-to-3 day positive analysis in the future. Currently, the FDA is collaborating in adapting its methodology to quantitate very low numbers of the organisms in foods.
| |
| | |
| Bio-Rad Laboratories (www.bio-rad.com) have come up with media called Rapid'L.Mono Medium which cut short time to 48 hours
| |
| | |
| ==Epidemiology==
| |
| Researchers have found ''L. monocytogenes'' in at least 37 [[mammal|mammalian species]], both domesticated and feral, as well as in at least 17 species of [[birds]] and possibly in some species of [[fish]] and [[shellfish]]. Laboratories can isolate ''L. monocytogenes'' from [[soil]], [[silage]], and other environmental sources. ''L. monocytogenes'' is quite hardy and resists the deleterious effects of freezing, drying, and heat remarkably well for a bacterium that does not form spores. Most ''L. monocytogenes'' are pathogenic to some degree.
| |
| | |
| ==Routes of infection==
| |
| ''L. monocytogenes'' has been associated with such foods as raw [[milk]], pasteurized fluid milk<ref name=Fleming_1985>Fleming, D. W., S. L. Cochi, K. L. MacDonald, J. Brondum, P. S. Hayes, B. D. Plikaytis, M. B. Holmes, A. Audurier, C. V. Broome, and A. L. Reingold. 1985. Pasteurized milk as a vehicle of infection in an outbreak of listeriosis. N. Engl. J. Med. 312:404-407.</ref>, [[cheese]]s (particularly soft-ripened varieties), [[ice cream]], raw [[vegetables]], fermented raw-meat [[sausage]]s, raw and cooked [[poultry]], raw meats (of all types), and raw and smoked [[fish]]. Its ability to grow at temperatures as low as 0°C permits multiplication in refrigerated foods. In refrigeration temperature such as 4°C the amount of ferric iron promotes the growth of ''L. monocytogenes''.<ref name=Dworaczek_Kubo_Dykes_2002>Dykes, G. A., Dworaczek (Kubo), M. 2002. Influence of interactions between temperature, ferric ammonium citrate and glycine betaine on the growth of ''Listeria monocytogenes'' in a defined medium. Lett Appl Microbiol. 35(6):538-42.</ref>
| |
| | |
| == Infectious Cycle ==
| |
| <!-- Image with unknown copyright status removed: [[Image:LifeCyclePortnoy02.gif|frame|Infectious Life Cycle]] -->
| |
| The primary site of infection is the intestinal epithelium where the bacteria invade non-phagocytic cells via the "zipper" mechanism. Uptake is stimulated by the binding of listerial internalins (Inl) to host cell adhesion factors such as E-[[cadherin]] or Met. This binding activates certain Rho-GTPases which subsequently bind and stabilize [[Wiskott Aldrich Syndrome Protein]] (WASp). WASp can then bind the [[Arp2/3 complex]] and serve as an [[actin]] nucleation point. Subsequent actin polymerization extends the cell membrane around the bacterium, eventually engulfing it. The net effect of internalin binding is to exploit the junction forming-apparatus of the host into internalizing the bacterium. Note that ''L. monocytogenes'' can also invade phagocytic cells (e.g. [[macrophages]]) but only requires internalins for invasion of non-phagocytic cells.
| |
| | |
| Following internalisation, the bacterium must escape from the vacuole/phagosome before fusion with a [[lysosome]] can occur. Two main virulence factors which allow the bacterium to escape are [[listeriolysin O]] (LLO - encoded by ''hly'') and [[phospholipase C]] B (''plc''B). Secretion of LLO and PlcB disrupts the vacuolar membrane and allows the bacterium to escape into the cytoplasm where it may proliferate.
| |
| | |
| Once in the cytoplasm, ''L. monocytogenes'' exploits host [[actin]] for the second time. ActA proteins associated with the old bacterial cell pole (being a bacilli, ''L. monocytogenes'' septates in the middle of the cell and thus has one new pole and one old pole) are capable of binding the [[Arp2/3 complex]] and thus induce actin nucleation at a specific area of the bacterial cell surface. Actin polymerization then propels the bacterium unidirectionally into the host cell membrane. The protrusion which is formed may then be internalised by a neighbouring cell, forming a double-membrane vacuole from which the bacterium must escape using LLO and PlcB.
| |
|
| |
|
| | [[Image:Listeria3.jpg|thumb|none| Electron micrograph of a Listeria bacterium in tissue.<SMALL><SMALL>''[http://phil.cdc.gov/phil/ Adapted from Public Health Image Library (PHIL), Centers for Disease Control and Prevention.]''<ref name="PHIL">{{Cite web | title = Public Health Image Library (PHIL), Centers for Disease Control and Prevention | url = http://phil.cdc.gov/phil/}}</ref></SMALL></SMALL>]] |
| ==References== | | ==References== |
| <!-- ---------------------------------------------------------------
| |
| See http://en.wikipedia.org/wiki/Wikipedia:Footnotes for a
| |
| discussion of different citation methods and how to generate
| |
| footnotes using the <ref> & </ref> tags and the {{Reflist}} template
| |
| -------------------------------------------------------------------- -->
| |
| {{Reflist|2}} | | {{Reflist|2}} |
|
| |
| ==External links==
| |
| * [http://vm.cfsan.fda.gov/~mow/chap6.html/ U.S. Food and Drug Administration. Foodborne Pathogenic Microorganisms and Natural Toxins Handbook: Listeria monocytogenes]
| |
|
| |
| [[Category:Listeriaceae]]
| |
| [[Category:Foodborne illnesses]]
| |
|
| |
|
| |
|
| |
| [[cs:Listeria monocytogenes]]
| |
| [[de:Listeria monocytogenes]]
| |
| [[es:Listeria monocytogenes]]
| |
| [[fr:Listeria monocytogenes]]
| |
| [[ko:리스테리아]]
| |
| [[nl:Listeria monocytogenes]]
| |
| [[pt:Listeria monocytogenes]]
| |
| [[ja:リステリア]]
| |
|
| |
| {{WH}}
| |
| {{WS}}
| |