Lactose intolerance: Difference between revisions
Varun Kumar (talk | contribs) No edit summary |
Varun Kumar (talk | contribs) mNo edit summary |
||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
{{Infobox_Disease | {{Infobox_Disease | ||
| Name = Lactose intolerance | | Name = Lactose intolerance | ||
| Line 20: | Line 21: | ||
{{CMG}}; '''Associate Editor-In-Chief:''' {{CZ}} | {{CMG}}; '''Associate Editor-In-Chief:''' {{CZ}} | ||
==Overview== | ==Overview== | ||
Revision as of 19:41, 29 July 2011
| Lactose intolerance | |
 | |
|---|---|
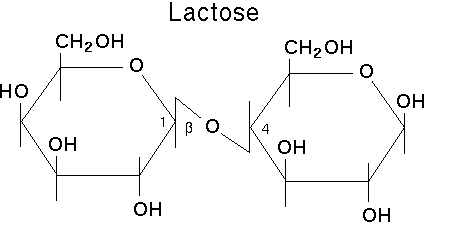
| Lactose, a disaccharide of β-D-galactose & β-D-glucose, that is normally split by lactase. | |
| ICD-10 | E73 |
| ICD-9 | 271.3 |
| OMIM | 223100 150220 |
| DiseasesDB | 7238 |
| MedlinePlus | 000276 |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [7]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [8]
Overview
Lactose intolerance (or hypolactasia) is the term used to describe a decline in the level of lactase, an enzyme needed for proper metabolization of lactose (a sugar that is a constituent of milk and other dairy products), in human beings. Although an estimated 70%[1] of adult humans are considered lactose intolerant, it is uncommon in healthy northern westerners and a few others groups.
There are three major types of lactose intolerance[2]:
- Primary lactose intolerance. Environmentally induced by weaning in non dairy consuming societies[3]. In most Asian and African cultures, mother's milk is the only commonly available milk and so milk consumption beyond infancy is not commonplace, therefore children become weaned, which is the same weaning process for all mammals (domesticated and wild). However societies such as the japanese where milk consumption has been on the increase, demonstrate that notwithstanding the genetic predisposition to lactose intolerance, they now present lower prevalence of lactose intolerance[4]. For any given individual the degree of weaning is probably genetically influenced.
- Secondary lactose intolerance. Environmentally induced, resulting from certain gastrointestinal diseases, including exposure to intestinal parasites such as giardia[5][6]. In such cases the production of lactase may be permanently disrupted.[9] + (Wiser 2000, Pennardt 2006).
- Congenital lactase deficiency present at birth and diagnosed in early infancy.
Without lactase, the lactose disaccharide in many dairy products remains uncleaved and can not be absorbed through the intestinal wall into the bloodstream, so remains in the intestines. Enteral bacteria adapt to the relative abundance of this undigested sugar and their operons quickly switch over to lactose metabolism, which produces copious amounts of gas by fermentation.
This also causes a range of unpleasant abdominal symptoms, including stomach cramps, bloating, flatulence and diarrhea. As with other unabsorbed sugars (mannitol), the lactose raises the osmotic pressure of the colon contents, preventing the colon from reabsorbing water and hence causing a laxative effect to add to the excessive gas production.
Lactase Biology
The gene is expressed and the enzyme synthesized if at least one of the two genes are present. Only when both gene expressions are affected is lactase enzyme synthesis reduced, which in turn reduces lactose digestion.[7]. Lactose tolerance(lactase persistence) is the dominant allele. Lactose intolerance is an autosomal recessive trait.
The normal mammalian condition is for the young of a species to experience reduced lactose (milk sugar) production at the end of the weaning period (a species-specific length of time). In non dairy consuming societies, lactase production usually drops about 90% during the first four years of life, although the exact drop over time varies widely. However, certain human populations have a mutation on chromosome 2 which results in a bypass of the common shutdown in lactase production, making it possible for members of these populations to continue consumption of fresh milk and other dairy products throughout their lives.
Pathological lactose intolerance can occur due to Coeliac disease, which damages the villi in the small intestine that produce lactase. This lactose intolerance is temporary. Lactose intolerance associated with coeliac disease ceases after the patient has been on a gluten-free diet long enough for the villi to recover.
Certain people who report problems with consuming lactose are not actually lactose intolerant. In a study of 323 Sicilian adults, Carroccio et al. (1998) found only 4% were both lactose intolerant and lactose maldigesters, while 32.2% were lactose maldigesters but did not test as lactose intolerant. However, Burgio et al. (1984) found that 72% of 100 Sicilians were lactose intolerant in their study and 106 of 208 northern Italians (i.e., 51%) were lactose intolerant.
Lactose intolerance by group
Most Japanese can consume 200 ml (8 fl oz) of milk without severe symptoms (McGee 2004; Swagerty et al, 2002).[4]
| Human groups | Individuals Examined | Percent Intolerant | Allele frequency |
| Dutch | N/A | 1%[8] | N/A |
| Swedes | N/A | 2%[9] | 0.14 |
| Europeans in Australia | 160 | 4%[9] | 0.20 |
| White people of Northern European and Scandinavian descent | N/A | 5%[3][10] | N/A |
| Danes | N/A | 5%[11] | N/A |
| British | 5–15%[12] | N/A | |
| Swiss | N/A | 10%[9] | 0.316 |
| White Americans | 245 | 12%[9] | 0.346 |
| Tuareg | N/A | 13%[12] | N/A |
| Germans | N/A | 15%[12] | N/A |
| Austrians | N/A | 15–20%[12] | N/A |
| Eastern Slavs (Russians, Belarusians, Ukrainians) | N/A | 15%[13] | N/A |
| Northern French | N/A | 17%[12] | N/A |
| Finns | 134 | 18%[9] | 0.424 |
| Central Italians | 65 | 19%[14] | N/A |
| Indian Children | N/A | 20%[3][10] | N/A |
| African Tutsi | N/A | 20%[9] | 0.447 |
| African Fulani | N/A | 23%[9] | 0.48 |
| Bedouins | N/A | 25%[12] | N/A |
| Northern Indians | N/A | 27%[15] | N/A |
| African American Children | N/A | 45%[3] | N/A |
| Indian Adults | 150 | 50%[3][10][16] | N/A |
| Southern Italians | 51 | 41%[14] | N/A |
| Saami (in Russia and Finland) | N/A | 25–60%[17] | N/A |
| Northern Italians | 89 | 52%[14] | N/A |
| North American Hispanics | N/A | 53%[12] | N/A |
| Balkans | N/A | 55%[12] | N/A |
| Mexican American Males | N/A | 55%[3][10] | N/A |
| Cretans | N/A | 56%[3] | N/A |
| African Maasai | 21 | 62%[18] | N/A |
| Southern French | N/A | 65%[12] | N/A |
| Greek Cypriots | N/A | 66%[3][10] | N/A |
| North American Jews | N/A | 68.8%[3][10] | N/A |
| Southern Indians | N/A | 70%[15] | N/A |
| Sicilians | 100 | 71%[19][20] | N/A |
| South Americans | N/A | 65–75%[12] | N/A |
| Rural Mexicans | N/A | 73.8%[3][10] | N/A |
| African Americans | 20 | 75%[9] | 0.87 |
| Kazakhs from northwest Xinjiang | 195 | 76.4% [21] | |
| Lebanese | 75 | 78%[22] | N/A |
| Central Asians | N/A | 80%[12] | N/A |
| Alaskan Eskimo | N/A | 80%[3][10] | N/A |
| Australian Aborigines | 44 | 85%[9] | 0.922 |
| Inner Mongolians | 198 | 87.9%[21] | |
| African Bantu | 59 | 89%[9] | 0.943 |
| Asian Americans | N/A | 90%[3][10] | N/A |
| Northeastern Han Chinese | 248 | 92.3%[21] | |
| Chinese | 71 | 93%[9] | 0.964 |
| Southeast Asians | N/A | 98%[3][10] | N/A |
| Thais | 134 | 98%[9] | 0.99 |
| Native Americans | 24 | 100%[9] | 1.00 |
The statistical significance varies greatly depending on number of people sampled.
Lactose intolerance levels also increase with age. At ages 2 - 3 yrs., 6 yrs., and 9 - 10 yrs., the amount of lactose intolerance is, respectively:
- 6% to 15% in white Americans and northern Europeans
- 18%, 30%, and 47% in Mexican Americans
- 25%, 45%, and 60% in black South Africans
- approximately 30%, 80%, and 85% in Chinese and Japanese
- 30–55%, 90%, and >90% in Mestizos of Peru[23][24]
Chinese and Japanese populations typically lose between 80 and 90 percent of their ability to digest lactose within three to four years of weaning.
Ashkenazi Jews can keep 20 - 30 percent of their ability to digest lactose for many years.[25] Of the 10% of the Northern European population that develops lactose intolerance, the development of lactose intolerance is a gradual process spread out over as many as 20 years.[26]
Diagnosis
The differential diagnosis must distinguish lactose intolerance from milk allergy, which is an abnormal immune response (usually) to milk proteins.
Since lactose intolerance is the normal state for most adults on a worldwide scale, and not considered a disease condition, diagnosis is not necessarily required. However, when confirmation is necessary, different tests are suggested:
Hydrogen Breath Test
After an overnight fast, 50 grams of lactose (in a solution with water) are swallowed. If the lactose cannot be digested, enteric bacteria metabolize it and produce hydrogen. This can be detected in the air the patient exhales. The test takes about 2 to 3 hours. A medical condition with similar symptoms is fructose malabsorption.
In conjunction, measuring the blood glucose level every 10 - 15 minutes after ingestion will show a "flat curve" in individuals with lactose malabsorption, while the lactase persistent will have a significant "top", with an elevation of typically 50 to 100% within 1 - 2 hours.
Stool acidity
Required for a clinical diagnosis.[27]
Intestinal biopsy
An intestinal biopsy can confirm lactose intolerance following discovery of elevated hydrogen in the hydrogen breath test[28].
Informal test
Done on someone by having the person follow these steps:
- Drink 2-4 cups of milk on an empty stomach.
- For 48 hours abstain from consuming alcohol or any food or medication (may reduce bacterial activity and falsify results) containing dairy in the forms of lactose, whey, or milk solids.
- Monitor for signs of intestinal discomfort, nausea, vomiting or severe headache / migraine.
- In presence of these symptoms, lactose intolerance is to be suspected and one should seek medical advice.
History of diagnosis
The ancient Greek physician Hippocrates (460-370 B.C.) first noted gastrointestinal upset and skin problems in some who consumed milk;[29] patients experiencing the former symptom may likely have been suffering from lactose intolerance. However, it was only in the last few decades that the syndrome was more widely described by modern medical science.
The condition was first recognized in the 1950s and 1960s when various organizations like the United Nations began to engage in systematic famine-relief efforts in countries outside Europe for the first time. Holzel et al (1959) and Durand (1959) produced two of the earliest studies of lactose intolerance. As anecdotes of embarrassing dairy-induced discomfort piled up, the First World donor countries could no longer ascribe the reports to spoilage in transit or inappropriate food preparation at the recipient end in the Third World.
Since the first nations to industrialize and develop modern scientific medicine were dominated by people of Western and Northern European descent, adult dairy consumption was long taken for granted. Westerners for some time did not recognize that the majority of the human ethno-genetic groups could not consume dairy products during adulthood. Although there had been regular contact between Europeans and non-Europeans throughout history, the notion that large-scale medical studies should be representative of the ethnic diversity of the human populations (as well as all genders and ages) did not become well-established until after the American Civil Rights Movement.
Since then, the relationship between lactase and lactose has been thoroughly investigated in food science due to the growing market for dairy products among non-Europeans.
Originally it was hypothesised that gut bacteria such as E. coli produced the lactase enzyme needed to cleave lactose into its constituent monosaccharides and thus become metabolisable and digestible by humans. Some form of human-bacteria symbiosis was proposed as a means of producing lactase in the human digestive tract. Genetics and protein analysis techniques by the early 1970s revealed this to be untrue; humans produce their own lactase enzyme natively in intestine cells.
According to Heyman (2006), approximately 70% of the global population cannot tolerate lactose in adulthood. Thus, some argue that the terminology should be reversed — lactose intolerance should be seen as the norm, and the minority groups should be labeled as having lactase persistence. A counter argument to this is that the cultures that don't generally consume unmodified milk products have little need to discuss their intolerance to it, leaving the cultures for which lactose intolerance is a significant dietary issue to define its terminology.
History of genetic prevalence
Lactose intolerance has been studied as an aid in understanding ancient diets and population movement in prehistoric societies. Milking an animal vastly increases the efficiency of raising it in regards to the calories that can be extracted compared to consumption of its meat alone. It is not surprising then, that consuming milk products became an important part of the agricultural way of life in the Neolithic.
Given that at this time the majority of the population of all areas was lactose intolerant, it is believed that most of the milk was used to make mature cheeses (mostly lactose free). This also corresponds to the amount of lactose in the milk; horse milk has a great deal of lactose, and goat's milk has very little. Roman authors also remark that the people of northern Europe, particularly Britain and Germany drank unprocessed milk (as opposed to the Romans who made cheese). This corresponds very closely with modern European distributions of lactose intolerance, where the people of Britain, Germany and Scandinavia have a good tolerance, and those of southern Europe, especially Italy, have a poorer tolerance.[10]
In east Asia, historical sources also attest that the Chinese did not consume milk, whereas the nomads that lived on the borders did. Again, this reflects modern distributions of intolerance. China is particularly notable as a place of poor tolerance, whereas in Mongolia and the Asian steppes horse milk is drunk regularly. Here they even make an alcoholic beverage, called Kumis, from horse milk (although the fermentation process reduces the amount of lactose present). This tolerance is thought to be advantageous as the nomads do not settle down long enough to process mature cheese or may find themselves regularly going through brief periods of starvation; and given that their prime source of income is generated through horses, to ignore their milk as a source of calories would be greatly detrimental.
The African Fulani have a nomadic origin and their culture once completely revolved around cow, goat, and sheep herding. Dairy products were once a large source of nutrition for them. As might be expected if lactase persistence evolved in response to dairy product consumption, they are particularly tolerant to lactose (about 77% of the population). Many Fulani still live in Guinea-Conakry, Burkina Faso, Mali, Nigeria, Niger, Cameroon, and Chad.
There is some debate on exactly where and when the mutation(s) occurred. Some argue for separate mutation events in Sweden (which has one of the lowest levels of lactose intolerance in the world) and the Arabian Peninsula around 4000 BC. However, others argue for a single mutation event in the Middle East at about 4500 BC which then subsequently radiated. Some sources suggest a third and more recent mutation in the East African Tutsi. Whatever the precise origin in time and place, most modern Western Europeans and people of European ancestry show the effects of this mutation (that is, they are able to safely consume milk products all their lives) while most modern East Asians, sub-Saharan Africans and native peoples of the Americas and Pacific Islands do not (making them lactose intolerant as adults)[11].
The Maasai ability to consume dairy without exhibiting symptoms may be due to a different genetic mutation than westeners[30]"
A thorough scientific overview of genetic polymorphisms of intestinal lactase activity in adult hypolactasia, is in chapter 76 of OMMBID.[31] A noncoding variation in the MCM6 gene has been strongly associated with adult type hypolactasia.[32]
Managing lactose intolerance
For persons living in societies where the diet contains relatively little dairy, lactose intolerance is not considered a condition that requires treatment. However, those living among societies that are largely lactose-tolerant may find lactose intolerance troublesome. Although there are still no methodologies to reinstate lactase production, some individuals have reported their intolerance to vary over time (depending on health status and pregnancy[33]). Lactose intolerance is not usually an all-or-nothing condition: the reduction in lactase production, and hence, the amount of lactose that can be tolerated varies from person to person. Since lactose intolerance poses no further threat to a person's health, managing the condition consists in minimizing the occurrence and severity of symptoms.
Berdanier and Hargrove recognise 4 general principals:
- Avoidance of dietary lactose,
- Substitution to maintain nutrient intake,
- Regulation of calcium intake,
- Use of enzyme substitute.
Avoiding lactose-containing products
Since each individual's tolerance to lactose varies, according to the US National Institute of Health, "Dietary control of lactose intolerance depends on people learning through trial and error how much lactose they can handle."[12]. Label reading is essential as commercial terminology varies according to language and region[28].
Lactose is present in 2 large food categories: Conventional dairy products, and as a food additive (in dairy and non dairy products).
Dairy products
Lactose is a water soluble molecule. In the curdling process lactose is found in the water portion along with whey and casein, but is not found in the fat portion. Therefore fat percentage and the curdling process have a certain impact on which foods may be tolerated. Conversely, low fat dairy foods often have various dairy derivatives such as milk solids added to them to enhance sweetness. Any dairy product which is "fat reduced" or "fat free" generally have a slightly higher lactose percentage.
Milk. Human milk has the highest lactose percentage at around 9%. Unprocessed cow milk has 4.7% lactose. Unprocessed milk from other mammals contains similar lactose percentages (goat milk 4.1%[34], buffalo 4.86%[35], yak 4.93%[36], sheep milk 4.6% [37]).
Butter. The butter making process by definition separates milk's water components from the fat components. Lactose, being a water soluble molecule, will not be present in the butter unless milk solids are added to the ingredients.
Yogurt and kefir. People can be more tolerant of traditionally made yogurt than milk because it contains some lactase produced by the bacterial cultures used to make the yogurt. However, many commercial brands contain additional milk solids (lactose). Read labels.
Cheeses. Traditionally made hard cheese (such as Swiss cheese) and soft ripened cheeses may create less reaction than the equivalent amount of milk because of the processes involved. Fermentation and fat content contribute to lesser amounts of lactose. Traditionally made Swiss or Cheddar might contain 10% of the lactose found in whole milk. In addition, the traditional aging methods of cheese (over 2 yrs) reduces their lactose content to practically nothing[13]. Commercial cheese brands are generally manufactured by modern processes that do not have the same lactose reducing properties. And "aged" cheeses are usually aged for very short periods, and usually no laws mandate what qualifies as an aged cheese. One must read labels carefully.
Buttermilk, sour cream and ice cream, like yogurt, if made the traditional way, will generally be quite tolerable, but most modern brands add milk solids. [38] Consult labels [39].
Examples of lactose levels in foods. As scientific consensus has not been reached concerning lactose percentage analysis methods [40] (non-hydrated form or the mono-hydrated form), and considering that dairy content varies greatly according to labeling practices, geography and manufacturing processes, lactose numbers may not be very reliable. The following are examples of lactose levels in foods which commonly set off symptoms [14]. These quantities are to be treated as guidelines only. Read the labels to be sure.
Dairy product Lactose Content Yogurt, plain, low-fat, 240 mL 5 g Milk, reduced fat, 240 mL 11 g Swiss cheese, 28 g 1 g Ice cream, 120 mL 6 g Cottage cheese, 120 mL 2–3 g
Lactose in non dairy products
Lactose (also present when labels state whey, milk solids, modified milk ingredients, etc) as a commercial food additive is used for its texture, flavor and adhesive qualities, and is found in foods such as processed meats[41] (sausages/hot dogs, sliced meats, Pâtés), margarines[42], sliced breads[43][44], breakfast cereals, dried fruit, processed foods, medications, preprepared meals, meal replacement (powders and bars), protein supplements (powders and bars).
Kosher products labeled pareve are mostly free of milk, however if a "D" is present next to the circled K, the food contains milk solids[41].
Alternative products
Milk. The dairy industry has created quality low-lactose or lactose-free products to replace regular dairy. Lactose-free milk can be produced by passing milk over lactase enzyme bound to an inert carrier: once the molecule is cleaved, there are no lactose ill-effects. A form is available with reduced amounts of lactose (typically 30% of normal), and alternatively with almost 0%. Finland has had "HYLA" (acronym for hydrolysed lactose) products available for many years, even though the number of lactose intolerant people there is relatively small. These low-lactose level cow's milk products, ranging from ice cream to cheese, use a Valio patented chromatographic separation method to remove lactose. The ultra-pasteurization process, combined with aseptic packaging ensures a long shelf-life. Recently, the range of low-lactose products available in Finland has been augmented with milk and other dairy products (such as ice cream, butter, and buttermilk) that contain no lactose at all. The remaining about 20% of lactose in HYLA products is taken care of enzymatically. These typically cost 2 - 4 times more than equivalent products containing lactose. Valio also markets these products in Sweden.
Plant based milks and derivatives are the only ones to be 100% lactose free (soy milk, almond milk, oat milk, rice milk, Hemp milk, Peanut milk[45].
Alternatively, a bacterium such as L. acidophilus may be added, which affects the lactose in milk the same way it affects the lactose in yogurt (see above).
Lactase supplementation
When lactose avoidance is not possible, or on occasions when a person chooses to consume such items, then enzymatic lactase supplements may be used.[46][47]
Lactase enzymes similar to the those produced in the small intestines of humans are produced industrially by fungi of the genus aspergillus. The enzyme, β-galactosidase, is available in tablet form in a variety of doses, in many countries without a prescription. It functions well only in high-acid environments, such as that found in the human gut due to the addition of gastric juices from the stomach. Unfortunately, too much acid can denature it,[48] and it therefore should not be taken on an empty stomach. Also, the enzyme is ineffective if it does not reach the small intestine by the time the problematic food does. Lactose-sensitive individuals should experiment with both timing and dosage to fit their particular need. But supplements such as these may not be able to provide the accurate amount of lactase needed to adequately digest the lactose contained in dairy products, which may lead to symptoms similar to the existing lactose intolerance.
While essentially the same process as normal intestinal lactose digestion, direct treatment of milk employs a different variety of industrially produced lactase. This enzyme, produced by yeast from the genus kluyveromyces, takes much longer to act, must be thoroughly mixed throughout the product, and is destroyed by even mildly acidic environments. It therefore has been much less popular as a consumer product (sold, where available, as a liquid) than the aspergillus-produced tablets, despite its predictable effectiveness. Its main use is in producing the lactose-free or lactose-reduced dairy products sold in supermarkets.
Enzymatic lactase suplementation may have an advantage over avoiding dairy products, in that alternative provision does not need to be made to provide sufficient calcium intake, especially in children.[49]
Rehabituation to dairy products
For some people having Secondary lactose intolerance and who are otherwise healthy, it may be possible to train bacteria in the large intestine to break down lactose more effectively[15] by consuming small quantities of dairy products several times a day over a couple of weeks. Adding dairy to diets of people who are sick may cause complications and even worsen the disease itself, especially if the dairy intake is not discovered in time as the real cause of the symptoms.
Nutritional Concerns
Primary Lactose Intolerance
Populations where Primary lactose intolerance are the norm have demonstrated similar health levels to westeners (outside of malnutrition issues, see History of Genetic Prevalence subsection above) or better health (Japan).
Secondary lactose intolerance
While secondary lactose intolerance does not inherently affect an individual's nutritional needs, according to mainstream media and "accepted" doctrines in western European and north American countries, dairy is an essential part of a healthy diet. Dairy products are relatively good and accessible sources of calcium and potassium and many contries mandate that milk be fortified with vitamin A and vitamin D. Consequently, in dairy consuming societies, dairy is often a main source of these nutrients; and, for lacto-vegetarians, a main source of vitamin B12. Individuals who reduce or eliminate consumption of dairy must obtain these nutrients elsewhere. Asian populations for whom dairy is not part of their food culture do not have present decreased health and sometimes present above average health, like Japan.
Plant based milk substitutes are not naturally rich in calcium, potassium, or vitamins A or D (and, like all non-animal products, contain no vitamin B12). However, prominent brands are often voluntarily fortified with many of these nutrients; one should read the label to be certain.
An increasing number of calcium-fortified breakfast foods, such as orange juice, bread, and dry cereal, have been appearing on supermarket shelves. Many fruits and vegetables are rich in potassium and vitamin A; animal products like meat and eggs are rich in vitamin B12, and the human body itself produces some vitamin D from exposure to direct sunlight. Finally, a dietitian or physician may recommend a vitamin or mineral supplement to make up for any remaining nutritional shortfall.
Lactose reduced dairy products have the same nutritional content as their full-lactose counterparts, but their taste and appearance may differ slightly.
Congenital lactase deficiency
Before the 20th century, infants with this disease could not survive. Now parents need only supply lactose-free milk and dairy products and the child will then have the same nutritional concerns as people with Secondary lactose intolerance.
References
- ↑ Kretchmer N. Lactose and lactase: a historical perspective. Gastroenterology, 1971;61, 805–813
- ↑ B. Heyman. Lactose Intolerance in Infants, Children, and Adolescents. PEDIATRICS Vol. 118 No. 3 September 2006, pp. 1279-1286 (doi:10.1542/peds.2006-1721)
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 Identification of a variant associated with adult-type hypolactasia, Enattah NS, Sahi T, Savilahti E, Terwilliger JD, Peltonen L, Jarvela I, Nat Genet. 2002 Feb;30(2):233–7
- ↑ 4.0 4.1 Studies on the etiology of milk intolerance in Japanese adults, Yoshida Y, Sasaki G, Goto S, Yanagiya S, Takashina K, Gastroenterol Jpn.;10(1):29–34, 1975
- ↑ "Intestinal Protozoa" Mark Wiser 2000
- ↑ "Giardiasis" Andre Pennardt February 22, 2006
- ↑ [1] Soy Nutrition
- ↑ Genetics of lactose digestion in humans., Flatz, G. , Advances in Human Genetics, 1987
- ↑ 9.00 9.01 9.02 9.03 9.04 9.05 9.06 9.07 9.08 9.09 9.10 9.11 9.12 Lactose and Lactase, Norman Kretchmer, Scientific American, October, 1972
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 10.6 10.7 10.8 10.9 Lactose Intolerance: The Molecular Explanation, UC Davis Nutritional Genomics website
- ↑ Anne Charlotte Jäger, "Laktose-intolerans: Gentest for laktose-intolerans - hurtig og billig diagnostik", DSKB-NYT, no. 1, February 2006.
- ↑ 12.00 12.01 12.02 12.03 12.04 12.05 12.06 12.07 12.08 12.09 12.10 Michael de Vrese, Anna Stegelmann, Bernd Richter, Susanne Fenselau, Christiane Laue and Jürgen Schrezenmeir,"Probiotics—compensation for lactase insufficiency", American Journal of Clinical Nutrition, Vol. 73, No. 2, 421S-429s, February 2001.
- ↑ Prevalence of the lactase deficiency among the population of the northwestern region of Russia
- ↑ 14.0 14.1 14.2 Primary adult lactose malabsorption in Italy: regional differences in prevalence and relationship to lactose intolerance and milk consumption, LT Cavalli-Sforza, A Strata, A Barone and L Cucurachi, American Journal of Clinical Nutrition, Vol 45, 748–754, 1987
- ↑ 15.0 15.1 Lactose intolerance in North and South Indians, Tandon RK, Joshi YK, Singh DS, Narendranathan M, Balakrishnan V, Lal K., Am J Clin Nutr 1981;35:943–6, 1981.
- ↑ Lactose malabsorption in apparently healthy adults in northern India, assessed using lactose hydrogen breath test, Rana SV, Bhasin DK, Naik N, Indian Journal of Gastroenterology, Volume 23, Issue 2, p. 78, 2004
- ↑ A. Kozlov, D. Lisitsyn, "Hypolactasia in Saami subpopulations of Russia and Finland", Anthropologischer Anzeiger, 55(3-4):281–287, 1997.
- ↑ Lactose malabsorption among Masai children of East Africa, RT Jackson, MC Latham, Am J Clin Nutr. 1979 Apr;32(4):779–82.
- ↑ Prevalence of primary adult lactose malabsorption and awareness of milk intolerance in Italy, G Roberto Burgio, Gebhard Flatz, Cristiana Barbera, Rosario Patan, Attilio Boner, Cinzia Cajozzo, and Sibylle D Flaiz, The American Journal of Clinical Nutrition 39: pp 100–104, January 1984.
- ↑ Lactose Intolerance, Tuula H. Vesa, Philippe Marteau, and Riitta Korpela, Journal of the American College of Nutrition, Vol. 19, No. 90002, 165S-175S (2000)
- ↑ 21.0 21.1 21.2 Prevalence of primary adult lactose malabsorption in three populations of northern China, Wang YG, Yan YS, Xu JJ, Du RF, Flatz SD, Kühnau W, Flatz G., Hum Genet. 1984;67(1):103-6.
- ↑ Lactose intolerance in the Lebanese population and in “Mediterranean lymphoma”, Salah M. Nasrallah, The American Journal of Clinical Nutrition 32 , pp. 1994–1996, October, 1979.
- ↑ Genetics and epidemiology of adult-type hypolactasia, Sahi T., Scand J Gastroenterol Suppl ;29:202:7–20, 1994
- ↑ Lactose malabsorption in Mexican-American children, Woteki CE, Weser E, Young EA, Am J Clin Nutr;29:19–24, 1976
- ↑ Genetics of lactase persistence and lactose intolerance, Swallow DM., Annu Rev Genet ;37:197 - 219, 2003.
- ↑ Systemic lactose intolerance: a new perspective on an old problem, S B Matthews, J P Waud, A G Roberts and A K Campbell, Postgraduate Medical Journal;81:167 - 173, 2005.
- ↑ http://digestive.niddk.nih.gov/ddiseases/pubs/lactoseintolerance/#diagnosed
- ↑ 28.0 28.1 Berdanier, Hargrove, Nutrition and Gene Expression. CRC Press. 1993. ISBN 0849369614
- ↑ Milk Intolerance: Lactose Intolerance and Cow's Milk Protein Allergy, J. Wilson, Newborn and Infant Nursing Reviews, Volume 5, Issue 4, Pages 203-207, Dec. 2005
- ↑ Swaminathan, Nikhil. Adaptation to Digesting Milk Is "Strongest Signal of Selection EverDecember 11, 2006, Scientific American.com.
- ↑ Charles Scriver, Beaudet, A.L., Valle, D., Sly, W.S., Vogelstein, B., Childs, B., Kinzler, K.W. (Accessed 2007). The Online Metabolic and Molecular Bases of Inherited Disease. New York: McGraw-Hill. - Summaries of 255 chapters, full text through many universities. There is also the OMMBID blog.
- ↑ Enattah N, Sahi T, Savilahti E, Terwilliger J, Peltonen L, Järvelä I (2002). "Identification of a variant associated with adult-type hypolactasia". Nat Genet. 30 (2): 233–7. PMID 11788828.
- ↑ Lactose Intolerance. Roy, Barakat, Nwakakwa, Shojamanesh, Khurana, July 5, 2006 About 44% of lactose intolerant women regain the ability to digest lactose during pregnancy. This might be caused by slow intestinal transit and intestinal flora changes during pregnancy.
- ↑ http://www.goatworld.com/articles/goatmilk/colostrum.shtml
- ↑ [http://bjas.hit.bg/07/693A.htm%7C Peeva. Composition of buffalo milk. Sources of specific effects on the separate components. 2001. Bulg. J. Agric. Sci., 7: 329-335
- ↑ http://jag.igr.poznan.pl/2004-Volume-45/2/pdf/2004_Volume_45_2-215-224.pdf
- ↑ http://en.wikipedia.org/wiki/Goat_milk
- ↑ [2] University of Guelph, Dept. of Food Science, Dairy Science and Technology
- ↑ [3] Reger, Combs, Coulter and Koch. A Comparison of Dry Sweet Cream Buttermilk and Non-Fat Dry Milk Solids in Breadmaking. Journal of Dairy Science Vol. 34 No. 2 136-144
- ↑ Goat Milk Composition
- ↑ 41.0 41.1 [4] General guidelines for milk allergy, Oregon Health & Science University
- ↑ http://www.gov.ns.ca/JUST/REGULATIONS/regs/marge.htm Margarine Regulations
- ↑ [5] Enriched White Bread in Canada The Canadian Celiac Association
- ↑ [6] Influence of Nonfat Dry Milk Solids on the Nutritive Value of Bread. Journal of Dairy Science Vol. 29 No. 12 821-829
- ↑ http://en.wikipedia.org/wiki/Plant_milk
- ↑ Montalto M, Curigliano V, Santoro L, Vastola M, Cammarota G, Manna R, Gasbarrini A, Gasbarrini G (2006). "Management and treatment of lactose malabsorption". World J Gastroenterol. 12 (2): 187–91. PMID 16482616.
- ↑ He M, Yang Y, Bian L, Cui H (1999). "[Effect of exogenous lactase on the absorption of lactose and its intolerance symptoms]". Wei Sheng Yan Jiu. 28 (5): 309–11. PMID 12712706.
- ↑ O'Connell S, Walsh G (2006). "Physicochemical characteristics of commercial lactases relevant to their application in the alleviation of lactose intolerance". Appl Biochem Biotechnol. 134 (2): 179–91. PMID 16943638.
- ↑ Heyman M (2006). "Lactose intolerance in infants, children, and adolescents". Pediatrics. 118 (3): 1279–86. PMID 16951027 doi:10.1542/peds.2006-1721.
See also
Additional Reading
- Durand, P. "Lactosurie et saccharosurie", In: BibI. Paediat. IV. Carbohydrate Metabolism in Children, edited by E. Rossi, E. Gautier, and J. W. Weber. Basel: S. Karger, 1959, pp. 496–502.
- Holzel, A., V. Schwarz and K. W. Sutcliffe, "Defective lactose absorption causing malnutrition in infancy", The Lancet 1: 1126, 1959.
- Carroccio, Montalto, Cavera, Notarbatolo (1998). "Lactose Intolerance and Self-Reported Milk Intolerance: Relationship with Lactose Maldigestion and Nutrient Intake". Journal of the American College of Nutrition. 17 (6): 631–636.
- McGee, Harold (2004). "Milk after infancy: dealing with lactose". On Food and Cooking (Revised Edition). Scribner. pp. pp 14&ndash, 15. ISBN 0-684-80001-2.
- Patel YT, Minocha A (2000). "Lactose intolerance: diagnosis and management". Compr Ther. 26 (4): 246–50. PMID 11126094.
- Rusynyk RA, Still CD (2001). "Lactose intolerance" (PDF). J Am Osteopath Assoc. 101 (4 Suppl Pt 1): S10–2. PMID 11392211.
- Swagerty DL Jr, Walling AD, Klein RM (2002). "Lactose intolerance". Am Fam Physician. 65 (9): 1845–50. PMID 12018807.
External links
- Milk allergy 'caused by Stone Age genes'
- United States National Institutes of Health page regarding lactose intolerance
- Types, symptoms, causes, treatments, and prevalence of Lactose Intolerance
- Study Detects Recent Instance of Human Evolution (Finding that lactose tolerance is a recent change)
- Scientific American: African Adaptation to Digesting Milk Is "Strongest Signal of Selection Ever" (East African cattle herding communities rapidly and independently evolved ability to digest lactose)
- Dairy Substitutes
- University of Alabama powerpoint slides of Dr. Bindon for Nutritional Anthropology course; includes a global map of regional and population-based lactose intolerance estimates
Template:SIB Template:Gastroenterology Template:Endocrine, nutritional and metabolic pathology
bg:Лактозна толерантност de:Laktoseintoleranz id:Lactose intolerance is:Mjólkuróþol he:רגישות ללקטוז nl:Lactose-intolerantie no:Laktoseintoleranse fi:Laktoosi-intoleranssi sv:Laktosintolerans uk:Непереносимість лактози