Insulin glargine: Difference between revisions
No edit summary |
No edit summary |
||
| Line 657: | Line 657: | ||
:*If you are using a new vial, remove the protective cap. Do not remove the stopper. | :*If you are using a new vial, remove the protective cap. Do not remove the stopper. | ||
: [[File:{{PAGENAME}}15.png|thumb|none|600px|This image is provided by the National Library of Medicine. | |||
: [[File:{{PAGENAME}}15.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | |||
:*Wipe the top of the vial with an alcohol swab. You do not have to shake the vial of LANTUS before use. | :*Wipe the top of the vial with an alcohol swab. You do not have to shake the vial of LANTUS before use. | ||
: [[File:{{PAGENAME}}16.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | |||
:*Use a new needle and syringe every time you give an injection. Use disposable syringes and needles only once. Throw them away properly. Never share needles and syringes. | :*Use a new needle and syringe every time you give an injection. Use disposable syringes and needles only once. Throw them away properly. Never share needles and syringes. | ||
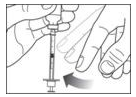
:*Draw air into the syringe equal to your insulin dose. Put the needle through the rubber top of the vial and push the plunger to inject the air into the vial. | :*Draw air into the syringe equal to your insulin dose. Put the needle through the rubber top of the vial and push the plunger to inject the air into the vial. | ||
: [[File:{{PAGENAME}} | : [[File:{{PAGENAME}}17.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | ||
: [[File:{{PAGENAME}}18.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | |||
:*Leave the syringe in the vial and turn both upside down. Hold the syringe and vial firmly in one hand. | :*Leave the syringe in the vial and turn both upside down. Hold the syringe and vial firmly in one hand. | ||
:*Make sure the tip of the needle is in the insulin. With your free hand, pull the plunger to withdraw the correct dose into the syringe. | :*Make sure the tip of the needle is in the insulin. With your free hand, pull the plunger to withdraw the correct dose into the syringe. | ||
: [[File:{{PAGENAME}}19.png|thumb|none|600px|This image is provided by the National Library of Medicine. | : [[File:{{PAGENAME}}19.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | ||
:*Before you take the needle out of the vial, check the syringe for air bubbles. If bubbles are in the syringe, hold the syringe straight up and tap the side of the syringe until the bubbles float to the top. Push the bubbles out with the plunger and draw insulin back in until you have the correct dose. | :*Before you take the needle out of the vial, check the syringe for air bubbles. If bubbles are in the syringe, hold the syringe straight up and tap the side of the syringe until the bubbles float to the top. Push the bubbles out with the plunger and draw insulin back in until you have the correct dose. | ||
: [[File:{{PAGENAME}}20.png|thumb|none|600px|This image is provided by the National Library of Medicine. | : [[File:{{PAGENAME}}20.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | ||
:*Remove the needle from the vial. Do not let the needle touch anything. You are now ready to inject. | :*Remove the needle from the vial. Do not let the needle touch anything. You are now ready to inject. | ||
| Line 689: | Line 693: | ||
:*Use alcohol or soap and water to clean the injection site. The injection site should be dry before you inject. | :*Use alcohol or soap and water to clean the injection site. The injection site should be dry before you inject. | ||
: [[File:{{PAGENAME}}21.png|thumb|none|600px|This image is provided by the National Library of Medicine. | |||
: [[File:{{PAGENAME}}21.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | |||
:*Pinch the skin. Stick the needle in the way your healthcare provider showed you. Release the skin. | :*Pinch the skin. Stick the needle in the way your healthcare provider showed you. Release the skin. | ||
:*Slowly push in the plunger of the syringe all the way, making sure you have injected all the insulin. Leave the needle in the skin for about 10 seconds. | :*Slowly push in the plunger of the syringe all the way, making sure you have injected all the insulin. Leave the needle in the skin for about 10 seconds. | ||
: [[File:{{PAGENAME}}22.png|thumb|none|600px|This image is provided by the National Library of Medicine. | |||
: [[File:{{PAGENAME}}22.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | |||
:*Pull the needle straight out and gently press on the spot where you injected yourself for several seconds. Do not rub the area. | :*Pull the needle straight out and gently press on the spot where you injected yourself for several seconds. Do not rub the area. | ||
Revision as of 16:45, 31 July 2014
{{DrugProjectFormSinglePage |authorTag=
Vignesh Ponnusamy, M.B.B.S. [1]
|genericName=
Insulin Glargine
|aOrAn=
a
|drugClass=
recombinant insulin analog
|indication=
type 1 diabetes mellitus and type 2 diabetes mellitus
|hasBlackBoxWarning=
|adverseReactions= hypoglycemia, allergic reactions, injection site reactions, lipodystrophy, pruritus, rash, edema and weight gain
|blackBoxWarningTitle= Title
|blackBoxWarningBody= ConditionName:
- Content
|fdaLIADAdult=
- Lantus is indicated to improve glycemic control in adults and pediatric patients with type 1 diabetes mellitus and in adults with type 2 diabetes mellitus.
- Important limitations of use:
- Lantus is not recommended for the treatment of diabetic ketoacidosis. intravenous short-acting insulin is the preferred treatment for this condition.
- LANTUS is a recombinant human insulin analog for once daily subcutaneous administration with potency that is approximately the same as the potency of human insulin. LANTUS exhibits a relatively constant glucose-lowering profile over 24 hours that permits once-daily dosing.
- LANTUS may be administered at any time during the day. LANTUS should be administered subcutaneously once a day at the same time every day. The dose of LANTUS must be individualized based on clinical response. Blood glucose monitoring is essential in all patients receiving insulin therapy.
- Patients adjusting the amount or timing of dosing with LANTUS, should only do so under medical supervision with appropriate glucose monitoring [see Warnings and Precautions (5.1).]
- In patients with type 1 diabetes, LANTUS must be used in regimens with short-acting insulin.
- The intended duration of activity of LANTUS is dependent on injection into subcutaneous tissue [see Clinical pharmacology (12.2)]. LANTUS should not be administered intravenously or via an insulin pump. Intravenous administration of the usual subcutaneous dose could result in severe hypoglycemia [see Warnings and Precautions (5.3)].
- As with all insulins, injection sites should be rotated within the same region (abdomen, thigh, or deltoid) from one injection to the next to reduce the risk of lipodystrophy [See Adverse Reactions (6.1)].
- In clinical studies, there was no clinically relevant difference in insulin glargine absorption after abdominal, deltoid, or thigh subcutaneous administration. As for all insulins, the rate of absorption, and consequently the onset and duration of action, may be affected by exercise and other variables, such as stress, intercurrent illness, or changes in co-administered drugs or meal patterns.
- Initiation of LANTUS therapy
- The recommended starting dose of LANTUS in patients with type 1 diabetes should be approximately one-third of the total daily insulin requirements. Short-acting, premeal insulin should be used to satisfy the remainder of the daily insulin requirements.
- The recommended starting dose of LANTUS in patients with type 2 diabetes who are not currently treated with insulin is 10 units (or 0.2 Units/kg) once daily, which should subsequently be adjusted to the patient's needs.
- The dose of LANTUS should be adjusted according to blood glucose measurements. The dosage of LANTUS should be individualized under the supervision of a healthcare provider in accordance with the needs of the patient.
- Converting to LANTUS from other insulin therapies
- If changing from a treatment regimen with an intermediate-or long-acting insulin to a regimen with LANTUS, the amount and timing of shorter-acting insulins and doses of any oral anti-diabetic drugs may need to be adjusted.
- If transferring patients from once-daily NPH insulin to once-daily LANTUS, the recommended initial LANTUS dose is the same as the dose of NPH that is being discontinued.
- If transferring patients from twice-daily NPH insulin to once-daily LANTUS, the recommended initial LANTUS dose is 80% of the total NPH dose that is being discontinued. This dose reduction will lower the likelihood of hypoglycemia [see Warnings and Precautions (5.3)].
- Dosage Forms And Strengths
- LANTUS solution for injection 100 Units per mL is available as:
- 10 mL Vial (1000 Units/10 mL)
- 3 mL SoloStar® disposable insulin device (300 Units/3 mL)
- LANTUS solution for injection 100 Units per mL is available as:
|offLabelAdultGuideSupport=
Condition1
- Developed by:
- Class of Recommendation:
- Strength of Evidence:
- Dosing Information
- Dosage
Condition2
There is limited information regarding Off-Label Guideline-Supported Use of Insulin glargine in adult patients.
|offLabelAdultNoGuideSupport=
Condition1
- Dosing Information
- Dosage
Condition2
There is limited information regarding Off-Label Non–Guideline-Supported Use of Insulin glargine in adult patients.
|fdaLIADPed=
Condition1
- Dosing Information
- Dosage
Condition2
There is limited information regarding FDA-Labeled Use of Insulin glargine in pediatric patients.
|offLabelPedGuideSupport=
Condition1
- Developed by:
- Class of Recommendation:
- Strength of Evidence:
- Dosing Information
- Dosage
Condition2
There is limited information regarding Off-Label Guideline-Supported Use of Insulin glargine in pediatric patients.
|offLabelPedNoGuideSupport=
Condition1
- Dosing Information
- Dosage
Condition2
There is limited information regarding Off-Label Non–Guideline-Supported Use of Insulin glargine in pediatric patients.
|contraindications=
- Condition1
|warnings=
- Description
Precautions
- Description
- Hypoglycemia
- Hypoglycemia is the most common adverse reaction of insulin, including LANTUS. The risk of hypoglycemia increases with intensive glycemic control. Patients must be educated to recognize and manage hypoglycemia. Severe hypoglycemia can lead to unconsciousness or convulsions and may result in temporary or permanent impairment of brain function or death. Severe hypoglycemia requiring the assistance of another person or parenteral glucose infusion or glucagon administration has been observed in clinical trials with insulin, including trials with LANTUS.
- The timing of hypoglycemia usually reflects the time-action profile of the administered insulin formulations. Other factors such as changes in food intake (e.g., amount of food or timing of meals), exercise, and concomitant medications may also alter the risk of hypoglycemia [See Drug Interactions (7)].
- The prolonged effect of subcutaneous LANTUS may delay recovery from hypoglycemia. Patients being switched from twice daily NPH insulin to once-daily LANTUS should have their initial LANTUS dose reduced by 20% from the previous total daily NPH dose to reduce the risk of hypoglycemia.
- As with all insulins, use caution in patients with hypoglycemia unawareness and in patients who may be predisposed to hypoglycemia (e.g., the pediatric population and patients who fast or have erratic food intake). The patient's ability to concentrate and react may be impaired as a result of hypoglycemia. This may present a risk in situations where these abilities are especially important, such as driving or operating other machinery.
- Early warning symptoms of hypoglycemia may be different or less pronounced under certain conditions, such as longstanding diabetes, diabetic neuropathy, use of medications such as beta-blockers, or intensified glycemic control. These situations may result in severe hypoglycemia (and, possibly, loss of consciousness) prior to the patient's awareness of hypoglycemia.
- Hypersensitivity and allergic reactions
- Severe, life-threatening, generalized allergy, including anaphylaxis, can occur with insulin products, including LANTUS.
|clinicalTrials=
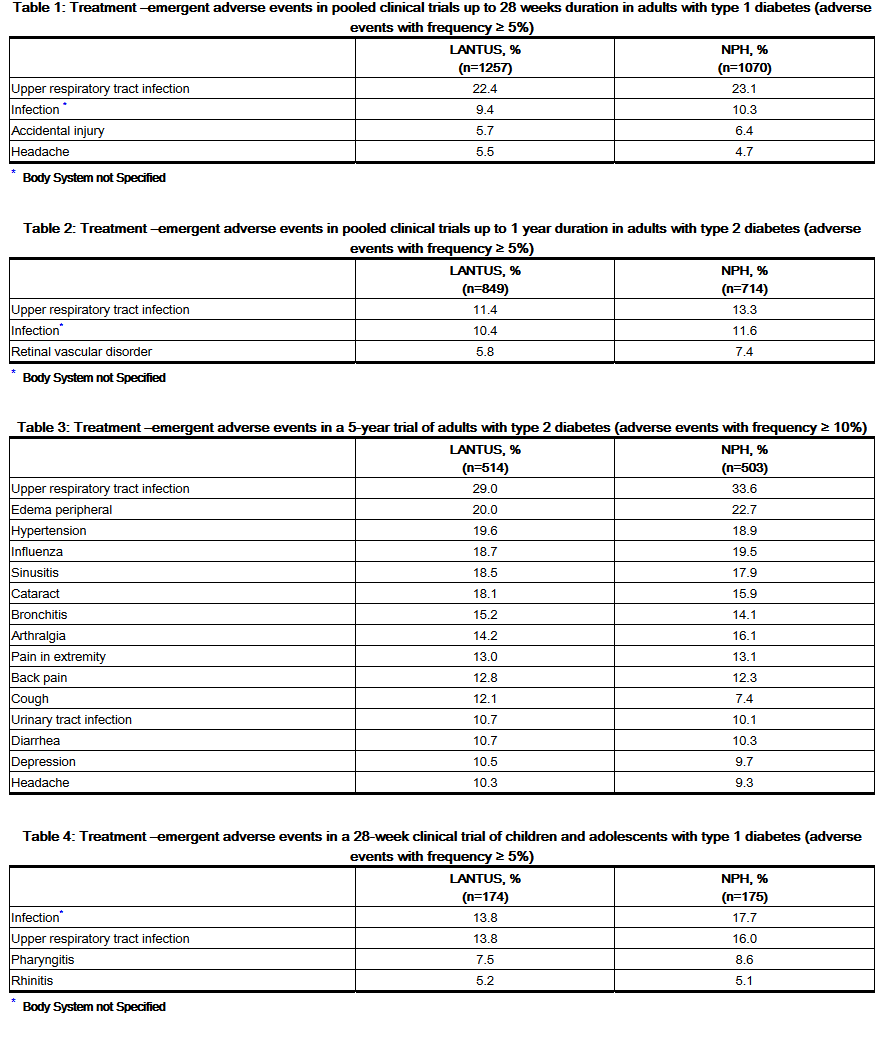
- Because clinical trials are conducted under widely varying designs, the adverse reaction rates reported in one clinical trial may not be easily compared to those rates reported in another clinical trial, and may not reflect the rates actually observed in clinical practice.
- The frequencies of treatment-emergent adverse events during LANTUS clinical trials in patients with type 1 diabetes mellitus and type 2 diabetes mellitus are listed in the tables below.
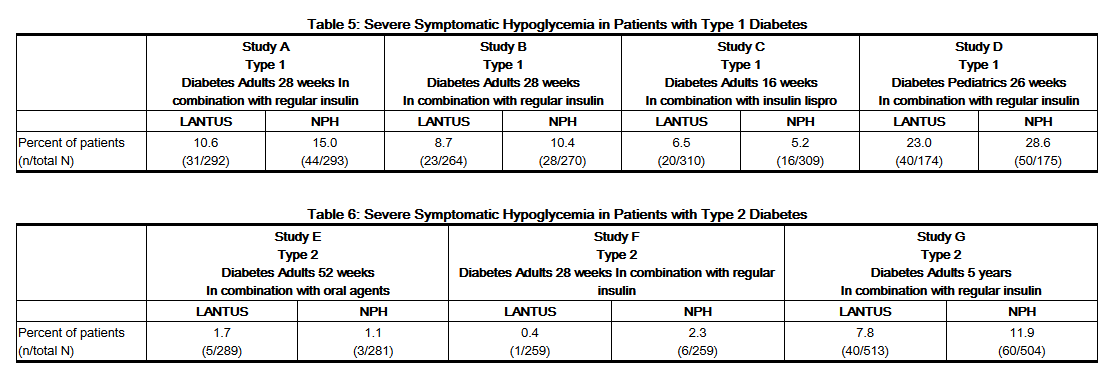
- Severe Hypoglycemia
- Hypoglycemia is the most commonly observed adverse reaction in patients using insulin, including LANTUS [See Warnings and Precautions (5.3)]. Tables 5, and 6 and 7 summarize the incidence of severe hypoglycemia in the LANTUS individual clinical trials. Severe symptomatic hypoglycemia was defined as an event with symptoms consistent with hypoglycemia requiring the assistance of another person and associated with either a blood glucose below 50 mg/dL (≤56 mg/dL in the 5-year trial and ≤36 mg/dL in the ORIGIN trial) or prompt recovery after oral carbohydrate, intravenous glucose or glucagon administration.
- The proportion of patients experiencing severe symptomatic hypoglycemia in the LANTUS clinical trials [See Clinical Studies (14)] in adults with type 1 diabetes and type 2 diabetes were comparable for all treatment regimens (see Tables 5 and 6). In the pediatric phase 3 clinical trial, children and adolescents with type 1 diabetes had a higher incidence of severe symptomatic hypoglycemia in the two treatment groups compared to the adult trials with type 1 diabetes.
Table 7 displays the proportion of patients experiencing severe symptomatic hypoglycemia in the Lantus and Standard Care groups in the ORIGIN Trial.
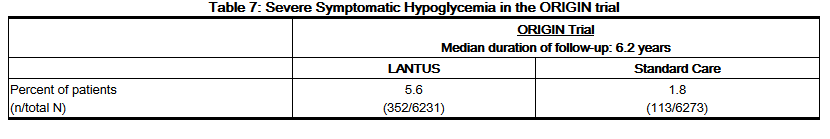
- Retinopathy
- Retinopathy was evaluated in the LANTUS clinical studies by analysis of reported retinal adverse events and fundus photography. The numbers of retinal adverse events reported for LANTUS and NPH insulin treatment groups were similar for patients with type 1 and type 2 diabetes.
- LANTUS was compared to NPH insulin in a 5-year randomized clinical trial that evaluated the progression of retinopathy as assessed with fundus photography using a grading protocol derived from the Early Treatment Diabetic Retinopathy Scale (ETDRS). Patients had type 2 diabetes (mean age 55 yrs) with no (86%) or mild (14%) retinopathy at baseline. Mean baseline HbA1c was 8.4%. The primary outcome was progression by 3 or more steps on the ETDRS scale at study endpoint. :*Patients with pre-specified post-baseline eye procedures (pan-retinal photocoagulation for proliferative or severe nonproliferative diabetic retinopathy, local photocoagulation for new vessels, and vitrectomy for diabetic retinopathy) were also considered as 3-step progressors regardless of actual change in ETDRS score from baseline. Retinopathy graders were blinded to treatment group assignment. The results for the primary endpoint are shown in Table 8 for both the per-protocol and Intent-to-Treat populations, and indicate similarity of Lantus to NPH in the progression of diabetic retinopathy as assessed by this outcome.
- Insulin initiation and intensification of glucose control
- Intensification or rapid improvement in glucose control has been associated with a transitory, reversible ophthalmologic refraction disorder, worsening of diabetic retinopathy, and acute painful peripheral neuropathy. However, long-term glycemic control decreases the risk of diabetic retinopathy and neuropathy.
- Lipodystrophy
- Long-term use of insulin, including LANTUS, can cause lipodystrophy at the site of repeated insulin injections. Lipodystrophy includes lipohypertrophy (thickening of adipose tissue) and lipoatrophy (thinning of adipose tissue), and may affect insulin absorption. Rotate insulin injection or infusion sites within the same region to reduce the risk of lipodystrophy. [See Dosage and Administration (2.1)].
- Weight gain
- Weight gain can occur with insulin therapy, including LANTUS, and has been attributed to the anabolic effects of insulin and the decrease in glucosuria.
- Peripheral Edema
- Insulin, including LANTUS, may cause sodium retention and edema, particularly if previously poor metabolic control is improved by intensified insulin therapy.
- Allergic Reactions
- Local Allergy
- As with any insulin therapy, patients taking LANTUS may experience injection site reactions, including redness, pain, itching, urticaria, edema, and inflammation. In clinical studies in adult patients, there was a higher incidence of treatment-emergent injection site pain in LANTUS-treated patients (2.7%) compared to NPH insulin-treated patients (0.7%). The reports of pain at the injection site did not result in discontinuation of therapy.
- Rotation of the injection site within a given area from one injection to the next may help to reduce or prevent these reactions. In some instances, these reactions may be related to factors other than insulin, such as irritants in a skin cleansing agent or poor injection technique. Most minor reactions to insulin usually resolve in a few days to a few weeks.
- Local Allergy
- Systemic Allergy
- Severe, life-threatening, generalized allergy, including anaphylaxis, generalized skin reactions, angioedema, bronchospasm, hypotension, and shock may occur with any insulin, including LANTUS and may be life threatening.
- Systemic Allergy
- Antibody production
- All insulin products can elicit the formation of insulin antibodies. The presence of such insulin antibodies may increase or decrease the efficacy of insulin and may require adjustment of the insulin dose. In phase 3 clinical trials of LANTUS, increases in titers of antibodies to insulin were observed in NPH insulin and insulin glargine treatment groups with similar incidences.
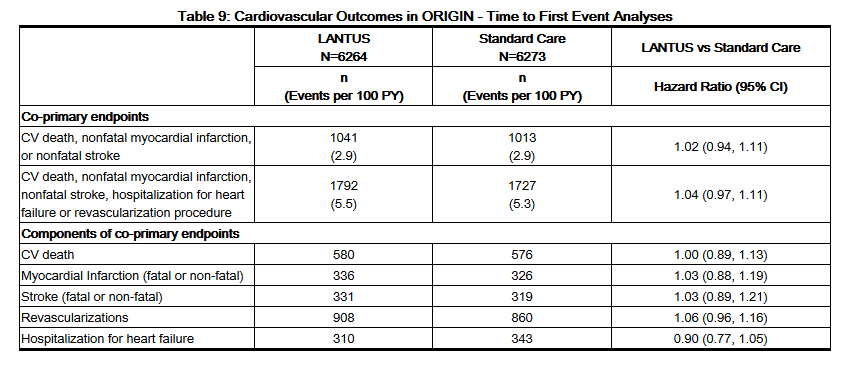
- Cardiovascular Safety
- The Outcome Reduction with Initial Glargine Intervention trial (i.e., ORIGIN) was an open-label, randomized, 2-by-2, factorial design study. One intervention in ORIGIN compared the effect of LANTUS to standard care on major adverse cardiovascular outcomes in 12,537 participants ≥ 50 years of age with abnormal glucose levels [i.e., impaired fasting glucose (IFG) and/or impaired glucose tolerance (IGT)] or early type 2 diabetes mellitus and established cardiovascular (i.e., CV) disease or CV risk factors at baseline.
- The objective of the trial was to demonstrate that LANTUS use could significantly lower the risk of major cardiovascular outcomes compared to standard care. Two co-primary composite cardiovascular endpoints were used in ORIGIN. The first co-primary endpoint was the time to first occurrence of a major adverse cardiovascular event defined as the composite of CV death, nonfatal myocardial infarction and nonfatal stroke. The second co-primary endpoint was the time to the first occurrence of CV death or nonfatal myocardial infarction or nonfatal stroke or revascularization procedure or hospitalization for heart failure.
- Participants were randomized to either LANTUS (N=6264) titrated to a goal fasting plasma glucose of ≤ 95 mg/dL or to standard care (N=6273). Anthropometric and disease characteristics were balanced at baseline. The mean age was 64 years and 8% of participants were 75 years of age or older. The majority of participants were male (65%). Fifty nine percent were Caucasian, 25% were Latin, 10% were Asian and 3% were Black. The median baseline BMI was 29 kg/m2. Approximately 12% of participants had abnormal glucose levels (IGT and/or IFG) at baseline and 88% had type 2 diabetes. For patients with type 2 diabetes, 59% were treated with a single oral antidiabetic drug, 23% had known diabetes but were on no antidiabetic drug and 6% were newly diagnosed during the screening procedure. The mean HbA1c (SD) at baseline was 6.5% (1.0). Fifty nine percent of participants had had a prior cardiovascular event and 39% had documented coronary artery disease or other cardiovascular risk factors.
- Vital status was available for 99.9% and 99.8% of participants randomized to LANTUS and standard care respectively at end of trial. The median duration of follow-up was 6.2 years [range: 8 days to 7.9 years]. The mean HbA1c (SD) at the end of the trial was 6.5% (1.1) and 6.8% (1.2) in the LANTUS and standard care group respectively. The median dose of LANTUS at end of trial was 0.45 U/kg. Eighty-one percent of patients randomized to LANTUS were using LANTUS at end of the study. The mean change in body weight from baseline to the last treatment visit was 2.2 kg greater in the LANTUS group than in the standard care group.
- Overall, the incidence of major adverse cardiovascular outcomes was similar between groups (see Table 9). All-cause mortality was also similar between groups.
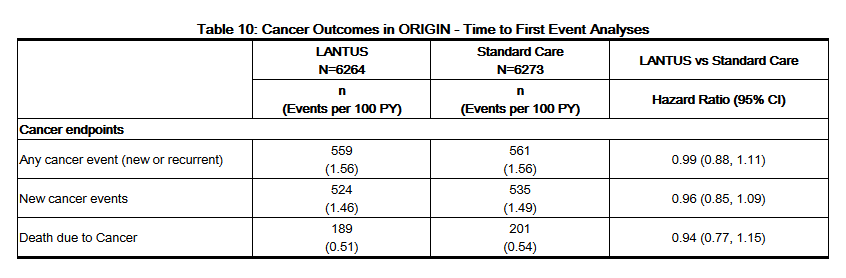
- Cancer
- In the ORIGIN trial, the overall incidence of cancer (all types combined) or death from cancer (Table 10) was similar between treatment groups.
|postmarketing=
- The following adverse reactions have been identified during post-approval use of LANTUS.
- Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to estimate reliably their frequency or establish a causal relationship to drug exposure.
- Medication errors have been reported in which other insulins, particularly short-acting insulins, have been accidentally administered instead of LANTUS [See Patient Counseling Information (17)]. To avoid medication errors between LANTUS and other insulins, patients should be instructed to always verify the insulin label before each injection.
|drugInteractions=
- A number of drugs affect glucose metabolism and may require insulin dose adjustment and particularly close monitoring.
- The following are examples of drugs that may increase the blood-glucose-lowering effect of insulins including LANTUS and, therefore, increase the susceptibility to hypoglycemia: oral anti-diabetic products, pramlintide, angiotensin converting enzyme (ACE) inhibitors, disopyramide, fibrates, fluoxetine, monoamine oxidase inhibitors, propoxyphene, pentoxifylline, salicylates, somatostatin analogs, and sulfonamide antibiotics.
- The following are examples of drugs that may reduce the blood-glucose-lowering effect of insulins including LANTUS: corticosteroids, niacin, danazol, diuretics, sympathomimetic agents (e.g., epinephrine, albuterol, terbutaline), glucagon, isoniazid, phenothiazine derivatives, somatropin, thyroid hormones, estrogens, progestogens (e.g., in oral contraceptives), protease inhibitors and atypical antipsychotic medications (e.g. olanzapine and clozapine).
- Beta-blockers, clonidine, lithium salts, and alcohol may either potentiate or weaken the blood-glucose-lowering effect of insulin. Pentamidine may cause hypoglycemia, which may sometimes be followed by hyperglycemia.
- The signs of hypoglycemia may be reduced or absent in patients taking sympatholytic drugs such as beta-blockers, clonidine, guanethidine, and reserpine.
|useInPregnancyFDA=
- Pregnancy Category C
- Subcutaneous reproduction and teratology studies have been performed with insulin glargine and regular human insulin in rats and Himalayan rabbits. Insulin glargine was given to female rats before mating, during mating, and throughout pregnancy at doses up to 0.36 mg/kg/day, which is approximately 7 times the recommended human subcutaneous starting dose of 10 Units/day (0.008 mg/kg/day), based on mg/m2. In rabbits, doses of 0.072 mg/kg/day, which is approximately 2 times the recommended human subcutaneous starting dose of 10 Units/day (0.008 mg/kg/day), based on mg/m2, were administered during organogenesis. The effects of insulin glargine did not generally differ from those observed with regular human insulin in rats or rabbits. However, in rabbits, five fetuses from two litters of the high-dose group exhibited dilation of the cerebral ventricles. Fertility and early embryonic development appeared normal.
- There are no well-controlled clinical studies of the use of LANTUS in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. It is essential for patients with diabetes or a history of gestational diabetes to maintain good metabolic control before conception and throughout pregnancy. Insulin requirements may decrease during the first trimester, generally increase during the second and third trimesters, and rapidly decline after delivery. Careful monitoring of glucose control is essential in these patients.
|useInPregnancyAUS=
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Insulin glargine in women who are pregnant.
|useInLaborDelivery= There is no FDA guidance on use of Insulin glargine during labor and delivery.
|useInNursing=
- It is unknown whether insulin glargine is excreted in human milk. Because many drugs, including human insulin, are excreted in human milk, caution should be exercised when LANTUS is administered to a nursing woman. Use of LANTUS is compatible with breastfeeding, but women with diabetes who are lactating may require adjustments of their insulin doses.
|useInPed=
- The safety and effectiveness of subcutaneous injections of LANTUS have been established in pediatric patients (age 6 to 15 years) with type 1 diabetes [see Clinical Studies (14)]. LANTUS has not been studied in pediatric patients younger than 6 years of age with type 1 diabetes. LANTUS has not been studied in pediatric patients with type 2 diabetes.
- Based on the results of a study in pediatric patients, the dose recommendation when switching to LANTUS is the same as that described for adults [see Dosage and Administration (2.3) and Clinical Studies (14)]. As in adults, the dosage of LANTUS must be individualized in pediatric patients based on metabolic needs and frequent monitoring of blood glucose.
|useInGeri=
- In controlled clinical studies comparing LANTUS to NPH insulin, 593 of 3890 patients (15%) with type 1 and type 2 diabetes were ≥65 years of age and 80 (2%) patients were ≥75 years of age. The only difference in safety or effectiveness in the subpopulation of patients ≥65 years of age compared to the entire study population was a higher incidence of cardiovascular events typically seen in an older population in both LANTUS and NPH insulin-treated patients.
- Nevertheless, caution should be exercised when LANTUS is administered to geriatric patients. In elderly patients with diabetes, the initial dosing, dose increments, and maintenance dosage should be conservative to avoid hypoglycemic reactions. Hypoglycemia may be difficult to recognize in the elderly [See Warnings and Precautions (5.3)].
|useInGender= There is no FDA guidance on the use of Insulin glargine with respect to specific gender populations.
|useInRace= There is no FDA guidance on the use of Insulin glargine with respect to specific racial populations.
|useInRenalImpair= There is no FDA guidance on the use of Insulin glargine in patients with renal impairment.
|useInHepaticImpair= There is no FDA guidance on the use of Insulin glargine in patients with hepatic impairment.
|useInReproPotential= There is no FDA guidance on the use of Insulin glargine in women of reproductive potentials and males.
|useInImmunocomp= There is no FDA guidance one the use of Insulin glargine in patients who are immunocompromised.
|administration=
- Subcutaneous
|monitoring=
- Careful glucose monitoring and dose adjustments of insulin, including LANTUS, may be necessary in patients with renal impairment and also in hepatic impairment.
Certain drugs may affect glucose metabolism, requiring insulin dose adjustment and close monitoring of blood glucose.
|IVCompat=
There is limited information regarding IV Compatibility of Insulin glargine in the drug label.
|overdose=
Acute Overdose
- An excess of insulin relative to food intake, energy expenditure, or both may lead to severe and sometimes prolonged and life-threatening hypoglycemia. Mild episodes of hypoglycemia can usually be treated with oral carbohydrates. Adjustments in drug dosage, meal patterns, or exercise may be needed.
- More severe episodes of hypoglycemia with coma, seizure, or neurologic impairment may be treated with intramuscular/subcutaneous glucagon or concentrated intravenous glucose. After apparent clinical recovery from hypoglycemia, continued observation and additional carbohydrate intake may be necessary to avoid recurrence of hypoglycemia.
Chronic Overdose
There is limited information regarding Chronic Overdose of Insulin glargine in the drug label.
|drugBox=
Insulin glargine
| |
| Systematic (IUPAC) name | |
| Recombinant human insulin | |
| Identifiers | |
| CAS number | |
| ATC code | A10 |
| PubChem | ? |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 6063 g/mol |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | ? |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
C(US) |
| Legal status |
POM(UK) [[Prescription drug|Template:Unicode-only]](US) |
| Routes | Subcutaneous |
|mechAction=
- The primary activity of insulin, including insulin glargine, is regulation of glucose metabolism. Insulin and its analogs lower blood glucose by stimulating peripheral glucose uptake, especially by skeletal muscle and fat, and by inhibiting hepatic glucose production. Insulin inhibits lipolysis and proteolysis, and enhances protein synthesis.
|structure=
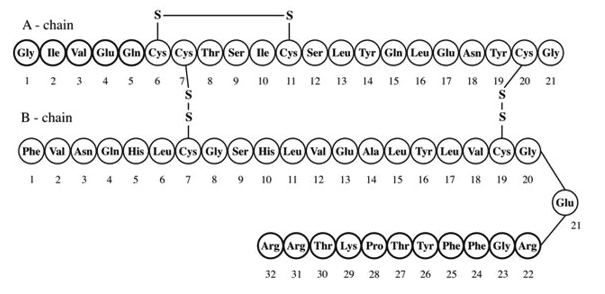
- LANTUS (insulin glargine [rDNA origin] injection) is a sterile solution of insulin glargine for use as a subcutaneous injection. Insulin glargine is a recombinant human insulin analog that is a long-acting (up to 24-hour duration of action), parenteral blood-glucose-lowering agent. LANTUS is produced by recombinant DNA technology utilizing a non-pathogenic laboratory strain of Escherichia coli (K12) as the production organism. Insulin glargine differs from human insulin in that the amino acid asparagine at position A21 is replaced by glycine and two arginines are added to the C-terminus of the B-chain. Chemically, insulin glargine is 21A-Gly-30Ba-L-Arg-30Bb-L-Arg-human insulin and has the empirical formula C267H404N72O78S6 and a molecular weight of 6063. Insulin glargine has the following structural formula:
- LANTUS consists of insulin glargine dissolved in a clear aqueous fluid. Each milliliter of LANTUS (insulin glargine injection) contains 100 Units (3.6378 mg) insulin glargine.
- The 10 mL vial presentation contains the following inactive ingredients per mL: 30 mcg zinc, 2.7 mg m-cresol, 20 mg glycerol 85%, 20 mcg polysorbate 20, and water for injection.
- The 3 mL cartridge presentation contains the following inactive ingredients per mL: 30 mcg zinc, 2.7 mg m-cresol, 20 mg glycerol 85%, and water for injection.
- The pH is adjusted by addition of aqueous solutions of hydrochloric acid and sodium hydroxide. LANTUS has a pH of approximately 4.
|PD=
- Insulin glargine is a human insulin analog that has been designed to have low aqueous solubility at neutral pH. At pH 4, as in the LANTUS injection solution, insulin glargine is completely soluble. After injection into the subcutaneous tissue, the acidic solution is neutralized, leading to formation of microprecipitates from which small amounts of insulin glargine are slowly released, resulting in a relatively constant concentration/time profile over 24 hours with no pronounced peak. This profile allows once-daily dosing as a basal insulin.
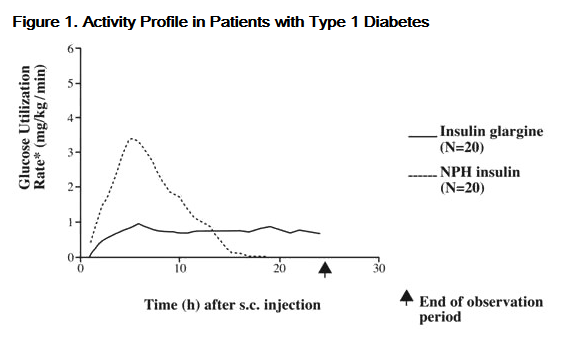
- In clinical studies, the glucose-lowering effect on a molar basis (i.e., when given at the same doses) of intravenous insulin glargine is approximately the same as that for human insulin. In euglycemic clamp studies in healthy subjects or in patients with type 1 diabetes, the onset of action of subcutaneous insulin glargine was slower than NPH insulin. The effect profile of insulin glargine was relatively constant with no pronounced peak and the duration of its effect was prolonged compared to NPH insulin. Figure 1 shows results from a study in patients with type 1 diabetes conducted for a maximum of 24 hours after the injection. The median time between injection and the end of pharmacological effect was 14.5 hours (range: 9.5 to 19.3 hours) for NPH insulin, and 24 hours (range: 10.8 to >24.0 hours) (24 hours was the end of the observation period) for insulin glargine.
- Determined as amount of glucose infused to maintain constant plasma glucose levels (hourly mean values); indicative of insulin activity.
- The longer duration of action (up to 24 hours) of LANTUS is directly related to its slower rate of absorption and supports once-daily subcutaneous administration. The time course of action of insulins, including LANTUS, may vary between individuals and within the same individual.
|PK=
- Absorption and Bioavailability
- After subcutaneous injection of insulin glargine in healthy subjects and in patients with diabetes, the insulin serum concentrations indicated a slower, more prolonged absorption and a relatively constant concentration/time profile over 24 hours with no pronounced peak in comparison to NPH insulin. Serum insulin concentrations were thus consistent with the time profile of the pharmacodynamic activity of insulin glargine.
- After subcutaneous injection of 0.3 Units/kg insulin glargine in patients with type 1 diabetes, a relatively constant concentration/time profile has been demonstrated. The duration of action after abdominal, deltoid, or thigh subcutaneous administration was similar.
- Metabolism
- A metabolism study in humans indicates that insulin glargine is partly metabolized at the carboxyl terminus of the B chain in the subcutaneous depot to form two active metabolites with in vitro activity similar to that of insulin, M1 (21A-Gly-insulin) and M2 (21A-Gly-des-30B-Thr-insulin). Unchanged drug and these degradation products are also present in the circulation.
- Special Populations
- Age, Race, and Gender
- Information on the effect of age, race, and gender on the pharmacokinetics of LANTUS is not available. However, in controlled clinical trials in adults (n=3890) and a controlled clinical trial in pediatric patients (n=349), subgroup analyses based on age, race, and gender did not show differences in safety and efficacy between insulin glargine and NPH insulin.
- Age, Race, and Gender
- Smoking
- The effect of smoking on the pharmacokinetics/pharmacodynamics of LANTUS has not been studied.
- Smoking
- Pregnancy
- The effect of pregnancy on the pharmacokinetics and pharmacodynamics of LANTUS has not been studied [see Use in Specific Populations (8.1)].
- Pregnancy
- Obesity
- In controlled clinical trials, which included patients with Body Mass Index (BMI) up to and including 49.6 kg/m2, subgroup analyses based on BMI did not show differences in safety and efficacy between insulin glargine and NPH insulin.
- Obesity
- Renal Impairment
- The effect of renal impairment on the pharmacokinetics of LANTUS has not been studied. However, some studies with human insulin have shown increased circulating levels of insulin in patients with renal failure. Careful glucose monitoring and dose adjustments of insulin, including LANTUS, may be necessary in patients with renal impairment.
- Renal Impairment
- Hepatic Impairment
- The effect of hepatic impairment on the pharmacokinetics of LANTUS has not been studied. However, some studies with human insulin have shown increased circulating levels of insulin in patients with liver failure. Careful glucose monitoring and dose adjustments of insulin, including LANTUS, may be necessary in patients with hepatic impairment.
- Hepatic Impairment
|nonClinToxic=
- Carcinogenesis, Mutagenesis, Impairment of Fertility
- In mice and rats, standard two-year carcinogenicity studies with insulin glargine were performed at doses up to 0.455 mg/kg, which was for the rat approximately 10 times and for the mouse approximately 5 times the recommended human subcutaneous starting dose of 10 Units/day (0.008 mg/kg/day), based on mg/m2. The findings in female mice were not conclusive due to excessive mortality in all dose groups during the study. Histiocytomas were found at injection sites in male rats (statistically significant) and male mice (not statistically significant) in acid vehicle containing groups. These tumors were not found in female animals, in saline control, or insulin comparator groups using a different vehicle. The relevance of these findings to humans is unknown.
- Insulin glargine was not mutagenic in tests for detection of gene mutations in bacteria and mammalian cells (Ames- and HGPRT-test) and in tests for detection of chromosomal aberrations (cytogenetics in vitro in V79 cells and in vivo in Chinese hamsters).
- In a combined fertility and prenatal and postnatal study in male and female rats at subcutaneous doses up to 0.36 mg/kg/day, which was approximately 7 times the recommended human subcutaneous starting dose of 10 Units/day (0.008 mg/kg/day), based on mg/m2, maternal toxicity due to dose-dependent hypoglycemia, including some deaths, was observed. Consequently, a reduction of the rearing rate occurred in the high-dose group only. Similar effects were observed with NPH insulin.
|clinicalStudies=
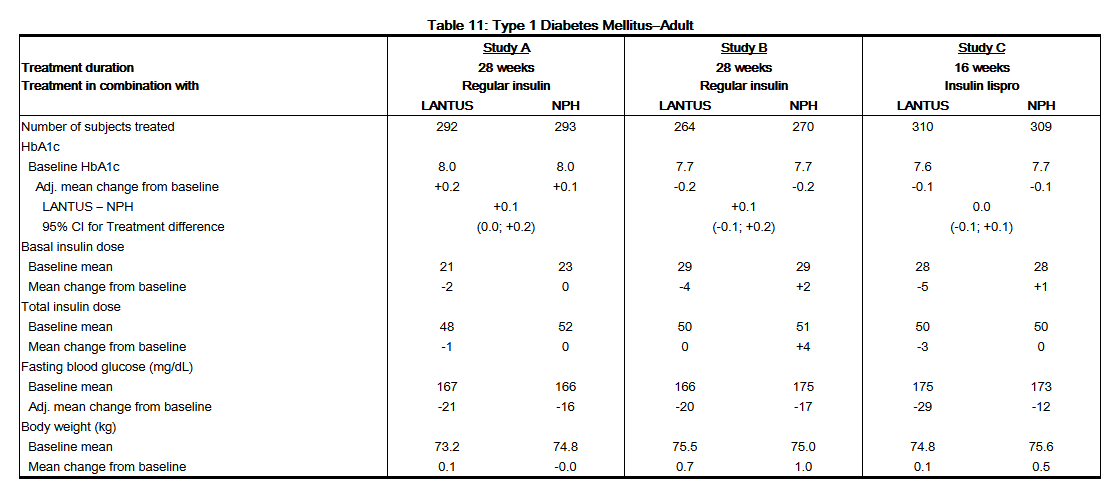
- The safety and effectiveness of LANTUS given once-daily at bedtime was compared to that of once-daily and twice-daily NPH insulin in open-label, randomized, active-controlled, parallel studies of 2,327 adult patients and 349 pediatric patients with type 1 diabetes mellitus and 1,563 adult patients with type 2 diabetes mellitus (see Tables 9–11), In general, the reduction in glycated hemoglobin (HbA1c) with LANTUS was similar to that with NPH insulin. The overall rates of hypoglycemia did not differ between patients with diabetes treated with LANTUS compared to NPH insulin [See Adverse Reactions (6.1)].
- Type 1 Diabetes-Adult (see Table 11).
- In two clinical studies (Studies A and B), patients with type 1 diabetes (Study A; n=585, Study B; n=534) were randomized to 28 weeks of basal-bolus treatment with LANTUS or NPH insulin. Regular human insulin was administered before each meal. LANTUS was administered at bedtime. NPH insulin was administered once daily at bedtime or in the morning and at bedtime when used twice daily.
- In another clinical study (Study C), patients with type 1 diabetes (n=619) were randomized to 16 weeks of basal-bolus treatment with LANTUS or NPH insulin. Insulin lispro was used before each meal. LANTUS was administered once daily at bedtime and NPH insulin was administered once or twice daily.
- In these 3 studies, LANTUS and NPH insulin had similar effects on HbA1c (Table 11) with a similar overall rate of hypoglycemia.
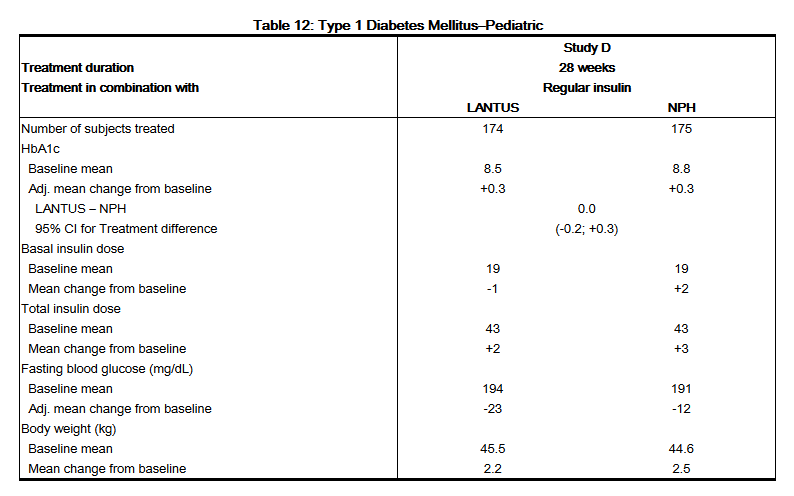
- Type 1 Diabetes–Pediatric (see Table 12).
- In a randomized, controlled clinical study (Study D), pediatric patients (age range 6 to 15 years) with type 1 diabetes (n=349) were treated for 28 weeks with a basal-bolus insulin regimen where regular human insulin was used before each meal. LANTUS was administered once daily at bedtime and NPH insulin was administered once or twice daily. Similar effects on HbA1c (Table 12) and the incidence of hypoglycemia were observed in both treatment groups.
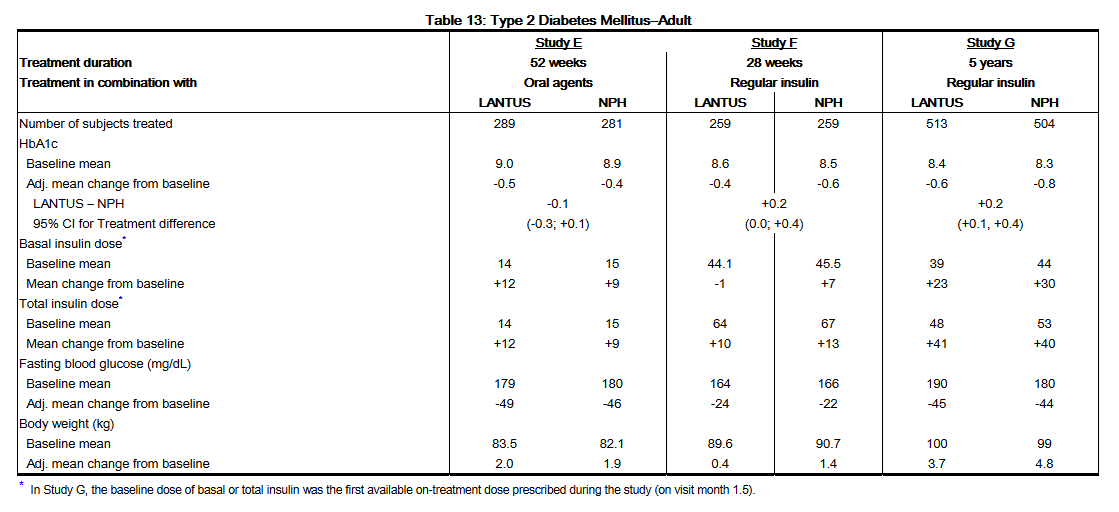
- Type 2 Diabetes–Adult (see Table 13).
- In a randomized, controlled clinical study (Study E) (n=570), LANTUS was evaluated for 52 weeks in combination with oral anti-diabetic medications (a sulfonylurea, metformin, acarbose, or combinations of these drugs). LANTUS administered once daily at bedtime was as effective as NPH insulin administered once daily at bedtime in reducing HbA1c and fasting glucose (Table 13). The rate of hypoglycemia was similar in LANTUS and NPH insulin treated patients.
- In a randomized, controlled clinical study (Study F), in patients with type 2 diabetes not using oral anti-diabetic medications (n=518), a basal-bolus regimen of LANTUS once daily at bedtime or NPH insulin administered once or twice daily was evaluated for 28 weeks. Regular human insulin was used before meals, as needed. LANTUS had similar effectiveness as either once- or twice-daily NPH insulin in reducing HbA1c and fasting glucose (Table 13) with a similar incidence of hypoglycemia.
- In a randomized, controlled clinical study (Study G), patients with type 2 diabetes were randomized to 5 years of treatment with once-daily LANTUS or twice-daily NPH insulin. For patients not previously treated with insulin, the starting dose of LANTUS or NPH insulin was 10 units daily. Patients who were already treated with NPH insulin either continued on the same total daily NPH insulin dose or started LANTUS at a dose that was 80% of the total previous NPH insulin dose. The primary endpoint for this study was a comparison of the progression of diabetic retinopathy by 3 or more steps on the Early Treatment Diabetic Retinopathy Study (ETDRS) scale. HbA1c change from baseline was a secondary endpoint. Similar glycemic control in the 2 treatment groups was desired in order to not confound the interpretation of the retinal data. Patients or study personnel used an algorithm to adjust the LANTUS and NPH insulin doses to a target fasting plasma glucose ≤100 mg/dL. After the LANTUS or NPH insulin dose was adjusted, other anti-diabetic agents, including pre-meal insulin were to be adjusted or added. The LANTUS group had a smaller mean reduction from baseline in HbA1c compared to the NPH insulin group, which may be explained by the lower daily basal insulin doses in the LANTUS group (Table 13). Both treatment groups had a similar incidence of reported symptomatic hypoglycemia. The incidences of severe symptomatic hypoglycemia are given in Table 6.
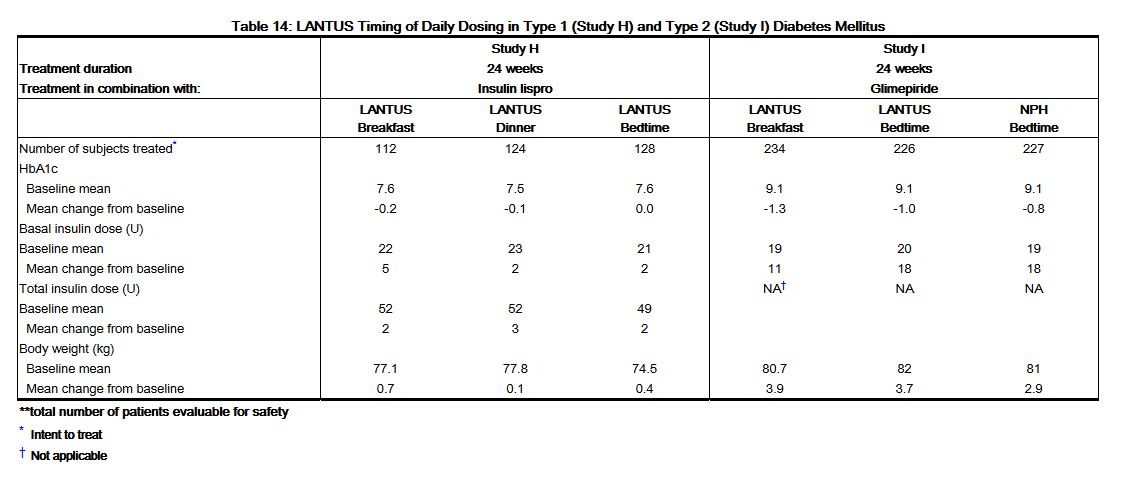
- LANTUS Timing of Daily Dosing (see Table 14).
- The safety and efficacy of LANTUS administered pre-breakfast, pre-dinner, or at bedtime were evaluated in a randomized, controlled clinical study in patients with type 1 diabetes (study H, n=378). Patients were also treated with insulin lispro at mealtime. LANTUS administered at different times of the day resulted in similar reductions in HbA1c compared to that with bedtime administration (see Table 14). In these patients, data are available from 8-point home glucose monitoring. The maximum mean blood glucose was observed just prior to injection of LANTUS regardless of time of administration.
- In this study, 5% of patients in the LANTUS-breakfast arm discontinued treatment because of lack of efficacy. No patients in the other two arms discontinued for this reason. The safety and efficacy of LANTUS administered pre-breakfast or at bedtime were also evaluated in a randomized, active-controlled clinical study (Study I, n=697) in patients with type 2 diabetes not adequately controlled on oral anti-diabetic therapy. All patients in this study also received glimepiride 3 mg daily. LANTUS given before breakfast was at least as effective in lowering HbA1c as LANTUS given at bedtime or NPH insulin given at bedtime (see Table 14).
|howSupplied=
- LANTUS solution for injection 100 units per mL (U-100) is available as:
- [[File:Insulin glargine13.png|thumb|none|600px|This image is provided by the National Library of Medicine.
Needles are not included in the packs.
BD Ultra-Fine™ needles to be used in conjunction with SoloStar are sold separately and are manufactured by BD.
- Storage
- LANTUS should not be stored in the freezer and should not be allowed to freeze. Discard LANTUS if it has been frozen.
- Unopened Vial/ SoloStar disposable insulin device:
- Unopened LANTUS vials, cartridge systems and SoloStar device should be stored in a refrigerator, 36°F – 46°F (2°C – 8°C). Discard after the expiration date.
- Open (In-Use) Vial:
- Vials must be discarded 28 days after being opened. If refrigeration is not possible, the open vial can be kept unrefrigerated for up to 28 days away from direct heat and light, as long as the temperature is not greater than 86°F (30°C).
- Open (In-Use) Vial:
- Open (In-Use) SoloStar disposable insulin device:
- The opened (in-use) SoloStar should NOT be refrigerated but should be kept at room temperature (below 86°F [30°C]) away from direct heat and light. The opened (in-use) SoloStar device must be discarded 28 days after being opened.
- Open (In-Use) SoloStar disposable insulin device:
- These storage conditions are summarized in the following table:
- [[File:Insulin glargine14.png|thumb|none|600px|This image is provided by the National Library of Medicine.
- Preparation and handling
- Parenteral drug products should be inspected visually prior to administration whenever the solution and the container permit. LANTUS must only be used if the solution is clear and colorless with no particles visible.
- Mixing and diluting: LANTUS must NOT be diluted or mixed with any other insulin or solution [See Warnings and Precautions (5.2)].
- Vial: The syringes must not contain any other medicinal product or residue.
- SoloStar: If SoloStar disposable insulin device, malfunctions, LANTUS may be drawn from the cartridge system or from SoloStar into a U-100 syringe and injected.
|fdaPatientInfo=
Instructions for patients
- Patients should be informed that changes to insulin regimens must be made cautiously and only under medical supervision.
- Patients should be informed about the potential side effects of insulin therapy, including lipodystrophy (and the need to rotate injection sites within the same body region), weight gain, allergic reactions, and hypoglycemia. Patients should be informed that the ability to concentrate and react may be impaired as a result of hypoglycemia. This may present a risk in situations where these abilities are especially important, such as driving or operating other machinery. Patients who have frequent hypoglycemia or reduced or absent warning signs of hypoglycemia should be advised to use caution when driving or operating machinery.
- Accidental mix-ups between LANTUS and other insulins, particularly short-acting insulins, have been reported. To avoid medication errors between LANTUS and other insulins, patients should be instructed to always check the insulin label before each injection.
- LANTUS must only be used if the solution is clear and colorless with no particles visible. Patients must be advised that LANTUS must NOT be diluted or mixed with any other insulin or solution.
- Patients should be advised not to share disposable or reusable insulin devices or needles with other patients, because doing so carries a risk for transmission of blood-borne pathogens.
- Patients should be instructed on self-management procedures including glucose monitoring, proper injection technique, and management of hypoglycemia and hyperglycemia. Patients must be instructed on handling of special situations such as intercurrent conditions (illness, stress, or emotional disturbances), an inadequate or skipped insulin dose, inadvertent administration of an increased insulin dose, inadequate food intake, and skipped meals.
- Patients with diabetes should be advised to inform their health care professional if they are pregnant or are contemplating pregnancy.
- Refer patients to the LANTUS "Patient Information" for additional information.
FDA approved patient labeling
See attached document at end of Full Prescribing Information.
sanofi-aventis U.S. LLC
Bridgewater, NJ 08807
A SANOFI COMPANY
©2013 sanofi-aventis U.S. LLC
Patient Information
====LANTUS® 10 mL vial (1000 units per vial) 100 units per mL (U-100) (insulin glargine [recombinant DNA origin] injection)====
- What is the most important information I should know about LANTUS?
- What is LANTUS?
- Who should NOT take LANTUS?
- How should I use LANTUS?
- What kind of syringe should I use?
- Mixing with LANTUS
- Instructions for Use
- How do I draw the insulin into the syringe?
- How do I inject LANTUS?
- What can affect how much insulin I need?
- What are the possible side effects of LANTUS and other insulins?
- How should I store LANTUS?
- General Information about LANTUS
- Read this "Patient Information" that comes with LANTUS (LAN-tus) before you start using it and each time you get a refill because there may be new information. This leaflet does not take the place of talking with your healthcare provider about your condition or treatment. If you have questions about LANTUS or about diabetes, talk with your healthcare provider.
- What is the most important information I should know about LANTUS?
- Do not change the insulin you are using without talking to your healthcare provider. Any change of insulin should be made cautiously and only under medical supervision. Changes in insulin strength, manufacturer, type (for example: Regular, NPH, analogs), species (beef, pork, beef-pork, human) or method of manufacture (recombinant DNA versus animal source insulin) may need a change in the dose. This dose change may be needed right away or later on during the first several weeks or months on the new insulin. Doses of oral anti-diabetic medicines may also need to change, if your insulin is changed.
- You must test your blood sugar levels while using an insulin, such as LANTUS. Your healthcare provider will tell you how often you should test your blood sugar level, and what to do if it is high or low.
- Do NOT dilute or mix LANTUS with any other insulin or solution. It will not work and you may lose blood sugar control, which could be serious.
- LANTUS comes as U-100 insulin and contains 100 units of LANTUS per milliliter (mL). One milliliter of U-100 insulin contains 100 units of insulin. (1 mL = 1 cc).
- What is Diabetes?
- Your body needs insulin to turn sugar (glucose) into energy. If your body does not make enough insulin, you need to take more insulin so you will not have too much sugar in your blood.
- Insulin injections are important in keeping your diabetes under control. But the way you live, your diet, careful checking of your blood sugar levels, exercise, and planned physical activity, all work with your insulin to help you control your diabetes.
- What is LANTUS?
- LANTUS (insulin glargine [recombinant DNA origin]) is a long-acting insulin. Because LANTUS is made by recombinant DNA technology (rDNA) and is chemically different from the insulin made by the human body, it is called an insulin analog. LANTUS is used to treat patients with diabetes for the control of high blood sugar. It is used once a day to lower blood sugar.
- LANTUS is a clear, colorless, sterile solution for injection under the skin (subcutaneously).
- The active ingredient in LANTUS is insulin glargine. The concentration of insulin glargine is 100 units per milliliter (mL), or U-100. LANTUS also contains zinc, metacresol, glycerol, polysorbate 20 and water for injection as inactive ingredients. Hydrochloric acid and/or sodium hydroxide may be added to adjust the pH.
- You need a prescription to get LANTUS. Always be sure you receive the right insulin from the pharmacy.
- Who should NOT take LANTUS?
- Do not take LANTUS if you are allergic to insulin glargine or any of the inactive ingredients in LANTUS. Check with your healthcare provider if you are not sure.
- Before starting LANTUS, tell your healthcare provider about all your medical conditions including if you:
- have liver or kidney problems. Your dose may need to be adjusted.
- are pregnant or plan to become pregnant. It is not known if LANTUS may harm your unborn baby. It is very important to maintain control of your blood sugar :**levels during pregnancy. Your healthcare provider will decide which insulin is best for you during your pregnancy.
- Before starting LANTUS, tell your healthcare provider about all your medical conditions including if you:
are breast-feeding or plan to breast-feed. It is not known whether LANTUS passes into your milk. Many medicines, including insulin, pass into human milk, and could affect your baby. Talk to your healthcare provider about the best way to feed your baby. about all the medicines you take including prescription and non-prescription medicines, vitamins, and herbal supplements.
- if you take any other medicines, especially ones commonly called TZDs (thiazolidinediones).
- if you have heart failure or other heart problems. If you have heart failure, it may get worse while you take TZDs with Lantus.
- How should I use LANTUS?
- See the "Instructions for Use" including the "How do I draw the insulin into the syringe?" section for additional information.
- Follow the instructions given by your healthcare provider about the type or types of insulin you are using. Do not make any changes with your insulin unless you have talked to your healthcare provider. Your insulin needs may change because of illness, stress, other medicines, or changes in diet or activity level. :**Talk to your healthcare provider about how to adjust your insulin dose.
- You may take LANTUS at any time during the day but you must take it at the same time every day.
- Only use LANTUS that is clear and colorless. If your LANTUS is cloudy or slightly colored, return it to your pharmacy for a replacement.
- Follow your healthcare provider's instructions for testing your blood sugar.
- Inject LANTUS under your skin (subcutaneously) in your upper arm, abdomen (stomach area), or thigh (upper leg). Never inject it into a vein or muscle.
- Change (rotate) injection sites within the same body area.
- What kind of syringe should I use?
- Always use a syringe that is marked for U-100 insulin. If you use other than U-100 insulin syringe, you may get the wrong dose of insulin causing serious problems for you, such as a blood sugar level that is too low or too high. Always use a new needle and syringe each time you give LANTUS injection.
- NEEDLES AND SYRINGES MUST NOT BE SHARED.
- Disposable syringes and needles should be used only once. Used syringe and needle should be placed in sharps containers (such as red biohazard containers), hard plastic containers (such as detergent bottles), or metal containers (such as an empty coffee can). Such containers should be sealed and disposed of properly.
- Mixing with LANTUS
- Do NOT dilute or mix LANTUS with any other insulin or solution. It will not work as intended and you may lose blood sugar control, which could be serious.
Instructions for Use
- How do I draw the insulin into the syringe?
- The syringe must be new and does not contain any other medicine.
- Do not mix LANTUS with any other type of insulin.
- Follow these steps:
- Wash your hands with soap and water or with alcohol.
- Check the insulin to make sure it is clear and colorless. Do not use the insulin after the expiration date stamped on the label, if it is colored or cloudy, or if you see particles in the solution.
- If you are using a new vial, remove the protective cap. Do not remove the stopper.
- Wipe the top of the vial with an alcohol swab. You do not have to shake the vial of LANTUS before use.

This image is provided by the National Library of Medicine. - Use a new needle and syringe every time you give an injection. Use disposable syringes and needles only once. Throw them away properly. Never share needles and syringes.
- Draw air into the syringe equal to your insulin dose. Put the needle through the rubber top of the vial and push the plunger to inject the air into the vial.
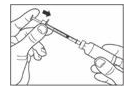
This image is provided by the National Library of Medicine. - Leave the syringe in the vial and turn both upside down. Hold the syringe and vial firmly in one hand.
- Make sure the tip of the needle is in the insulin. With your free hand, pull the plunger to withdraw the correct dose into the syringe.
- Before you take the needle out of the vial, check the syringe for air bubbles. If bubbles are in the syringe, hold the syringe straight up and tap the side of the syringe until the bubbles float to the top. Push the bubbles out with the plunger and draw insulin back in until you have the correct dose.
- Remove the needle from the vial. Do not let the needle touch anything. You are now ready to inject.
- How do I inject LANTUS?
- Inject LANTUS under your skin. Take LANTUS as prescribed by your healthcare provider.
- Follow these steps:
- Decide on an injection area - either upper arm, thigh or abdomen. Injection sites within an injection area must be different from one injection to the next.
- Use alcohol or soap and water to clean the injection site. The injection site should be dry before you inject.
- Pinch the skin. Stick the needle in the way your healthcare provider showed you. Release the skin.
- Slowly push in the plunger of the syringe all the way, making sure you have injected all the insulin. Leave the needle in the skin for about 10 seconds.
- Pull the needle straight out and gently press on the spot where you injected yourself for several seconds. Do not rub the area.
- Follow your healthcare provider's instructions for throwing away the used needle and syringe. Do not recap the used needle. Used needle and syringe should be placed in sharps containers (such as red biohazard containers), hard plastic containers (such as detergent bottles), or metal containers (such as an empty coffee can). Such containers should be sealed and disposed of properly.
|alcohol=
- Alcohol-Insulin glargine interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
|brandNames=
- ®[1]
|lookAlike=
- A® — B®[2]
|drugShortage=
}}
{{#subobject:
|Page Name=Insulin glargine |Pill Name=No image.jpg |Drug Name= |Pill Ingred=|+sep=; |Pill Imprint= |Pill Dosage= |Pill Color=|+sep=; |Pill Shape= |Pill Size (mm)= |Pill Scoring= |Pill Image= |Drug Author= |NDC=
}}
{{#subobject:
|Label Page=Insulin glargine |Label Name=Insulin glargine11.png
}}
{{#subobject:
|Label Page=Insulin glargine |Label Name=Insulin glargine11.png
}}
- ↑ Empty citation (help)
- ↑ "http://www.ismp.org". External link in
|title=(help)