Indium oxyquinoline: Difference between revisions
m (Robot: Automated text replacement (-{{SIB}} + & -{{EH}} + & -{{EJ}} + & -{{Editor Help}} + & -{{Editor Join}} +)) |
No edit summary |
||
| Line 1: | Line 1: | ||
{{DrugProjectFormSinglePage | |||
|authorTag={{AV}} | |||
|genericName=INDIUM IN 111 OXYQUINOLINE | |||
|aOrAn=a | |||
|drugClass=Diagnostic Agent | |||
|indicationType=diagnosis | |||
|indication=radiolabeling [[autologous]] [[leukocytes]]. Indium In 111 oxyquinoline labeled leukocytes may be used as an adjunct in the detection of [[inflammation|inflammatory processes]] to which [[leukocytes]] migrate, such as those associated with [[abscesses]] or other [[infection]], following reinjection and detection by appropriate imaging procedures. | |||
|adverseReactions=[[hypersensitivity reaction]] | |||
== | <!--Black Box Warning--> | ||
|blackBoxWarningTitle=Title | |||
|blackBoxWarningBody=<i><span style="color:#FF0000;">ConditionName: </span></i> | |||
* Content | |||
<!--Adult Indications and Dosage--> | |||
<!--FDA-Labeled Indications and Dosage (Adult)--> | |||
|fdaLIADAdult======Radiolabeling autologous leukocytes===== | |||
*Indium In 111 oxyquinoline is indicated for radiolabeling [[autologous]] [[leukocytes]]. | |||
Indium In 111 | *Indium In 111 oxyquinoline labeled [[leukocytes]] may be used as an adjunct in the detection of inflammatory processes to which [[leukocytes]] migrate, such as those associated with abscesses or other [[infection]], following reinjection and detection by appropriate imaging procedures. The degree of accuracy may vary with labeling techniques and with the size, location and nature of the inflammatory process. | ||
*Indium In 111 oxyquinoline labeled leukocyte imaging is not the preferred technique for the initial evaluation of patients with a high clinical probability of an [[abscess]] in a known location. [[Ultrasound]] or [[computed tomography]] may provide a better anatomical delineation of the [[infection|infectious process]] and information may be obtained more quickly than with labeled [[leukocytes]]. If localization by these techniques is successful, labeled [[leukocytes]] should not be used as a confirmatory procedure. If localization or diagnosis by these methods fails or is ambiguous, indium In 111 oxyquinoline labeled leukocyte imaging may be appropriate. | |||
======Dosing Information====== | |||
*The recommended adult (70 kg) dose of indium In 111 oxyquinoline labeled [[autologous]] [[leukocytes]] is 7.4 to 18.5 MBq, 200-500 µCi. Indium In 111 oxyquinoline solution is intended for the [[radiolabel|radiolabeling]] of [[autologous]] [[leukocytes]]. The indium In 111 oxyquinoline labeled [[autologous]] [[leukocytes]] are administered intravenously. | |||
*Imaging is recommended at approximately 24 hours post injection. Typically, anterior and posterior views of the chest, abdomen and pelvis should be obtained with other views as required. | |||
*Aseptic procedures and a shielded syringe should be employed in the withdrawal of indium In 111 oxyquinoline from the vial. Similar procedures should be employed during the labeling procedure and the administration of the labeled [[leukocytes]] to the patient. The user should wear waterproof gloves during the entire procedure. The patient's dose should be measured by a suitable [[radioactivity]] calibration system immediately before administration. At this time, the leukocyte preparation should be checked for gross [[clumping]] and [[red blood cell]] contamination. | |||
<!--Off-Label Use and Dosage (Adult)--> | |||
<!--Guideline-Supported Use (Adult)--> | |||
|offLabelAdultGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of {{PAGENAME}} in adult patients. | |||
<!--Non–Guideline-Supported Use (Adult)--> | |||
|offLabelAdultNoGuideSupport=There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of {{PAGENAME}} in adult patients. | |||
<!--Pediatric Indications and Dosage--> | |||
<!--FDA-Labeled Indications and Dosage (Pediatric)--> | |||
|fdaLIADPed=There is limited information regarding <i>FDA-Labeled Use</i> of {{PAGENAME}} in pediatric patients. | |||
<!--Off-Label Use and Dosage (Pediatric)--> | |||
<!--Guideline-Supported Use (Pediatric)--> | |||
|offLabelPedGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of {{PAGENAME}} in pediatric patients. | |||
<!--Non–Guideline-Supported Use (Pediatric)--> | |||
|offLabelPedNoGuideSupport=There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of {{PAGENAME}} in pediatric patients. | |||
<!--Contraindications--> | |||
|contraindications=* None known. | |||
= | <!--Warnings--> | ||
|warnings=*The content of the vial of indium In 111 oxyquinoline solution is intended only for use in the preparation of indium In 111 oxyquinoline labeled [[autologous]] [[leukocytes]], and is not to be administered directly. [[Autologous]] [[leukocyte]] labeling is not recommended in [[leukopenia|leukopenic patients]] because of the small number of available [[leukocytes]]. | |||
*Due to radiation exposure, indium In 111 oxyquinoline labeled leukocytes could cause fetal harm when administered to pregnant women. If this radiopharmaceutical is used during [[pregnancy]], the patient should be informed of the potential hazard to the fetus. | |||
Indium In 111 oxyquinoline labeled leukocytes | *Indium In 111 oxyquinoline labeled [[autologous]] [[leukocytes]] should be used only when the benefit to be obtained exceeds the risks involved in children under eighteen years of age owing to the high [[radiation]] burden and the potential for delayed manifestation of long-term adverse effects. | ||
=====Precautions===== | |||
*[[Clumping]] of cells may produce focal accumulations of radioactivity in [[lungs]] which do not wash out in 24 hours and thus may lead to false positive results. This phenomenon can be detected by imaging the chest immediately after [[injection]]. | |||
*The normally high uptake of indium In 111 oxyquinoline labeled [[leukocytes]] by [[spleen]] and [[liver]] may mask inflammatory lesions in these organs. Labeled [[leukocytes]] have been observed to accumulate in the [[colon]] and [[accessory spleens]] of patients with or without disease. | |||
*[[Chemotaxis]] of [[granulocytes]] deteriorates during storage and loss of [[chemotaxis]] may cause false negative scans. The spontaneous release of indium In 111 has been reported to range from about 3% at one hour to 24% at 24 hours. The maximum amount of time recommended between drawing the blood and reinjection should not exceed 5 hours. It is recommended that the labeled cells be used within one hour of preparation, if possible and in no case more than three hours after preparation. | |||
*Plasma and red cell contamination impairs labeling efficiency of leukocytes. Hemolyzed blood in labeled [[leukocytes]] may produce heart pool activity and should be avoided. | |||
*Cell aggregates of various degrees have been reported. Cell labeling techniques and standing of cell preparation may be contributing factors. | |||
*[[Nuclear medicine]] procedures involving withdrawal and reinjection of blood have the potential for transmission of blood borne pathogens. Procedures should be implemented to avoid administration errors and viral contamination of personnel during blood product labeling. A system of checks similar to the ones used for administering [[blood transfusions]] should be routine. | |||
== | ======General====== | ||
*Strict aseptic techniques should be used to maintain [[sterility]] throughout the procedures for using this product. | |||
*Do not use after the expiration time and date (5 days after calibration time) stated on the label. | |||
*The contents of the vial are radioactive. Adequate shielding of the preparation must be maintained at all times. | |||
*Indium In 111 oxyquinoline, like other [[radioactive drugs]], must be handled with care and appropriate safety measures should be used to minimize [[radiation]] exposure to clinical personnel. Care should also be taken to minimize radiation exposure to the patient consistent with proper patient management. | |||
*[[Radiopharmaceuticals]] should be used only by physicians who are qualified by training and experience in the safe use and handling of [[radionuclides]] and whose experience and training have been approved by the appropriate governmental agency authorized to license the use of radio-nuclides. | |||
<!--Adverse Reactions--> | |||
= | <!--Clinical Trials Experience--> | ||
|clinicalTrials=*Sensitivity reactions ([[urticaria]]) have been reported. The presence of fever may mask pyrogenic reactions from indium In 111 oxyquinoline labeled [[leukocytes]]. The possibility of delayed adverse reactions has not been studied. | |||
<!--Postmarketing Experience--> | |||
|postmarketing=There is limited information regarding <i>Postmarketing Experience</i> of {{PAGENAME}} in the drug label. | |||
<!--Drug Interactions--> | |||
|drugInteractions=<!--Use in Specific Populations--> | |||
|FDAPregCat=C | |||
|useInPregnancyFDA=* Animal reproduction studies have not been conducted with Indium In 111 Oxyquinoline labeled [[leukocytes]]. It is also not known whether Indium In 111 Oxyquinoline labeled [[leukocytes]] can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. | |||
*However, Indium Nitrate, a closely related compound, was [[teratogenic]] and embryopathic in hamsters. Indium In 111 Oxyquinoline labeled [[leukocytes]] should be given to a pregnant woman only if clearly needed. | |||
*Ideally, examinations using radiopharmaceuticals, especially those elective in nature, in women of childbearing capability should be performed during the first few (approximately ten) days following the onset of menses. | |||
|useInPregnancyAUS=There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of {{PAGENAME}} in women who are pregnant. | |||
|useInLaborDelivery=There is no FDA guidance on use of {{PAGENAME}} during labor and delivery. | |||
|useInNursing=*It is reported that indium 111 is secreted in human milk following administration of indium In 111 labeled leukocytes. Therefore, formula feedings should be substituted for breast feedings. | |||
|useInPed=*Safety and effectiveness in pediatric patients below age 18 have not been established | |||
|useInGeri=*Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy. | |||
|useInGender=There is no FDA guidance on the use of {{PAGENAME}} with respect to specific gender populations. | |||
|useInRace=There is no FDA guidance on the use of {{PAGENAME}} with respect to specific racial populations. | |||
|useInRenalImpair=There is no FDA guidance on the use of {{PAGENAME}} in patients with [[renal impairment]]. | |||
|useInHepaticImpair=There is no FDA guidance on the use of {{PAGENAME}} in patients with [[hepatic impairment]]. | |||
|useInReproPotential=There is no FDA guidance on the use of {{PAGENAME}} in women of reproductive potentials and males. | |||
|useInImmunocomp=There is no FDA guidance one the use of {{PAGENAME}} in patients who are [[immunocompromised]]. | |||
<!--Administration and Monitoring--> | |||
|administration=*[[Intravenous]] | |||
|monitoring=*Image quality of radiolabeled [[leukocytes]] is indicative of efficacy | |||
<!--IV Compatibility--> | |||
|IVCompat=There is limited information regarding <i>IV Compatibility</i> of {{PAGENAME}} in the drug label. | |||
= | <!--Overdosage--> | ||
|overdose=There is limited information regarding <i>Chronic Overdose</i> of {{PAGENAME}} in the drug label. | |||
<!--Pharmacology--> | |||
<!--Drug box 2--> | |||
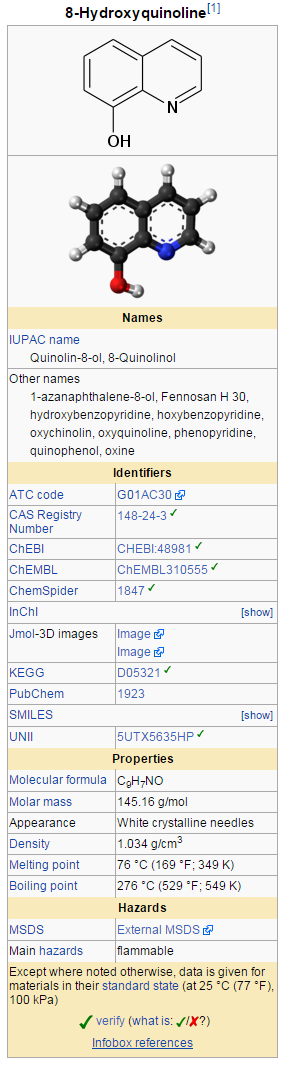
|drugBox=[[File:Oxyquinoline00.png|thumb|none|400px|This image is provided by the National Library of Medicine.]] | |||
<!--Mechanism of Action--> | |||
|mechAction=*Indium forms a saturated (1:3) complex with oxyquinoline. The complex is neutral and lipid-soluble, which enables it to penetrate the cell membrane. Within the cell, indium becomes firmly attached to cytoplasmic components; the liberated oxyquinoline is released by the cell. It is thought likely that the mechanism of labeling cells with indium In 111 oxyquinoline involves an exchange reaction between the oxyquinoline carrier and subcellular components which [[chelate]] indium more strongly than oxyquinoline. The low stability constant of the oxyquinoline complex, estimated at approximately 10, supports this theory. | |||
<!--Structure--> | |||
|structure=*Indium In 111 oxyquinoline (oxine) is a diagnostic radiopharmaceutical intended for radiolabeling autologous leukocytes. It is supplied as a sterile, non-pyrogenic, isotonic aqueous solution with a pH range of 6.5 to 7.5. Each mL of the solution contains 37 MBq, 1 mCi of indium In 111 [no carrier added, >1.85 GBq/µg indium (>50 mCi/µg indium)] at calibration time, 50 µg oxyquinoline, 100 µg polysorbate 80, and 6 mg of HEPES (N-2-hydroxyethyl-piperazine-N'-2-ethane sulfonic acid) buffer in 0.75% sodium chloride solution. The drug is intended for single use only and contains no [[bacteriostatic agent]]. The radionuclidic impurity limit for indium 114m is not greater than 37 kBq, 1 µCi of indium 114m per 37 MBq, 1 mCi of indium In 111 at the time of calibration. The radionuclidic composition at expiration time is not less than 99.75% of indium In 111 and not more than 0.25% of indium In 114m/114. | |||
Chemical name: Indium In 111 Oxyquinoline. | |||
= | |||
1. | |||
*The precise structure of the indium In 111 oxyquinoline complex is unknown at this time. The empirical formula is (C9H6NO)3 In 111. | |||
<!--Pharmacodynamics--> | |||
|PD=There is limited information regarding <i>Pharmacodynamics</i> of {{PAGENAME}} in the drug label. | |||
<!--Pharmacokinetics--> | |||
|PK=*Following the recommended leukocyte cell labeling procedure, approximately 77% of the added indium In 111 oxyquinoline is incorporated in the resulting cell pellet (which represents approximately 3-4 × 108 WBC). | |||
*Cell clumping can occur and was found in about one fifth of the [[leukocyte]] preparations examined. The presence of [[red blood cells]] or [[plasma]] will lead to reduced [[leukocyte]] labeling efficiency. [[Transferrin]] in plasma competes for indium In 111 oxyquinoline. | |||
*After injection of labeled leukocytes into normal volunteers, about 30% of the dose is taken up by [[spleen]] and 30% by [[liver]], reaching a plateau at 2-48 hours after injection. No significant clearance of [[radioactivity]] is observed at 72 hours in these two organs. Pulmonary uptake is 4-7.5% at 10 minutes but is lost rapidly; pulmonary [[radioactivity]] is usually visible in scans only up to about 4 hours after injection. | |||
*The human [[biodistribution]] studies in three normal subjects injected with indium In 111 oxyquinoline labeled leukocytes indicate a biexponential disappearance of indium In 111 from the blood when monitored for up to 72 hours. Between 9.5 to 24.4% of the injected dose remains in whole blood and clears with a biological half-time of 2.8 to 5.5 hours. The remainder (13-18%) clears from blood with a biological half-time of 64 to 116 hours. | |||
*Elimination from the body of injected indium In 111 oxyquinoline is probably mainly through decay to stable cadmium since only a negligible amount (less than 1%) of the dose is excreted in feces and urine in 24 hours. | |||
*Clearance from whole blood and biological distribution can vary considerably with the individual recipient, the condition of the injected cells and labeling techniques used. | |||
*Release of [[radioactivity]] from the labeled cells is about 3% at 1 hour and 24% at 24 hours. | |||
*Clearance from liver and spleen, for the purpose of calculating the radiation dose, is assumed to be equal to the physical half-life of indium In 111 (67.2 hours). | |||
<!--Nonclinical Toxicology--> | |||
|nonClinToxic======Carcinogenesis, Mutagenesis, Impairment of Fertility===== | |||
*Although earlier studies suggested that oxyquinoline (oxine) might have carcinogenic potential, recent studies have found no evidence of [[carcinogenicity]] in either rats or mice given oxyquinoline in feed at concentrations of 1,500 or 3,000 ppm for 103 weeks. | |||
*It has been reported that human [[lymphocytes]] labeled with recommended concentrations of indium In 111 oxyquinoline showed chromosome aberrations consisting of gaps, breaks and exchanges that appear to be [[radiation]] induced. At 555 kBq/107, 15 µCi/107 [[lymphocytes]] 93% of the cells were reported to be abnormal. The oncogenic potential of such [[lymphocytes]] has not been studied. It has been reported that the radiation dose to 108 leukocytes is 9 × 104 mGy (0.9 × 104 rads) from 18.5 MBq, 500 µCi. | |||
*Studies have not been performed to evaluate whether indium In 111 oxyquinoline affects [[fertility]] in male or female laboratory animals or humans. | |||
<!--Clinical Studies--> | |||
|clinicalStudies=There is limited information regarding <i>Clinical Studies</i> of {{PAGENAME}} in the drug label. | |||
<!--How Supplied--> | |||
|howSupplied=*Indium In 111 oxyquinoline solution is supplied in a vial as a single use only product containing 37 MBq, 1.0 mCi in 1.0 mL aqueous solution at the calibration date stated on the label. Vials are packaged in individual lead shields. | |||
NDC 17156-021-01 | |||
*The contents of the vial are radioactive and adequate shielding and handling precautions must be maintained. | |||
*This preparation is approved for use by persons licensed by the Illinois Emergency Management Agency pursuant to 32 IL. Adm. Code Section 330.260(a) and 335.4010 or equivalent licenses of the Nuclear Regulatory Commission or an Agreement State. | |||
<!--Patient Counseling Information--> | |||
|storage=*Indium In 111 oxyquinoline solution should be stored at room temperature (15-25°C, 59-77°F). | |||
*Indium In 111 oxyquinoline labeled [[autologous]] [[leukocytes]] should preferably be reinjected within one hour of labeling. The labeled cells may be stored at room temperature (15-25°C, 59-77°F) for up to three hours following completion of the cell labeling procedure. Reinjection of indium In 111 oxyquinoline labeled [[autologous]] [[leukocytes]] more than 5 hours after initial blood drawing is not recommended. | |||
*Sterile technique must be used throughout the collection, labeling and re-injection procedures. | |||
|fdaPatientInfo=There is limited information regarding <i>Patient Counseling Information</i> of {{PAGENAME}} in the drug label. | |||
<!--Precautions with Alcohol--> | |||
|alcohol=* Alcohol-{{PAGENAME}} interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | |||
<!--Brand Names--> | |||
|brandNames=<!--Look-Alike Drug Names--> | |||
|lookAlike=<!--Drug Shortage Status--> | |||
|drugShortage= | |||
}} | |||
{{PillImage | |||
|fileName=No image.jpg | |||
}} | |||
<!--Pill Image--> | |||
<!--Label Display Image--> | |||
{{LabelImage | |||
|fileName=Oxyquinoline01.png|This image is provided by the National Library of Medicine. | |||
}} | |||
{{LabelImage | |||
|fileName=Oxyquinoline02.png|This image is provided by the National Library of Medicine. | |||
}} | |||
<!--Category--> | |||
[[Category:Drug]] | |||
Latest revision as of 16:40, 2 April 2015
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Aparna Vuppala, M.B.B.S. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Indium oxyquinoline is a Diagnostic Agent that is FDA approved for the diagnosis of radiolabeling autologous leukocytes. Indium In 111 oxyquinoline labeled leukocytes may be used as an adjunct in the detection of inflammatory processes to which leukocytes migrate, such as those associated with abscesses or other infection, following reinjection and detection by appropriate imaging procedures.. Common adverse reactions include hypersensitivity reaction.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Radiolabeling autologous leukocytes
- Indium In 111 oxyquinoline is indicated for radiolabeling autologous leukocytes.
- Indium In 111 oxyquinoline labeled leukocytes may be used as an adjunct in the detection of inflammatory processes to which leukocytes migrate, such as those associated with abscesses or other infection, following reinjection and detection by appropriate imaging procedures. The degree of accuracy may vary with labeling techniques and with the size, location and nature of the inflammatory process.
- Indium In 111 oxyquinoline labeled leukocyte imaging is not the preferred technique for the initial evaluation of patients with a high clinical probability of an abscess in a known location. Ultrasound or computed tomography may provide a better anatomical delineation of the infectious process and information may be obtained more quickly than with labeled leukocytes. If localization by these techniques is successful, labeled leukocytes should not be used as a confirmatory procedure. If localization or diagnosis by these methods fails or is ambiguous, indium In 111 oxyquinoline labeled leukocyte imaging may be appropriate.
Dosing Information
- The recommended adult (70 kg) dose of indium In 111 oxyquinoline labeled autologous leukocytes is 7.4 to 18.5 MBq, 200-500 µCi. Indium In 111 oxyquinoline solution is intended for the radiolabeling of autologous leukocytes. The indium In 111 oxyquinoline labeled autologous leukocytes are administered intravenously.
- Imaging is recommended at approximately 24 hours post injection. Typically, anterior and posterior views of the chest, abdomen and pelvis should be obtained with other views as required.
- Aseptic procedures and a shielded syringe should be employed in the withdrawal of indium In 111 oxyquinoline from the vial. Similar procedures should be employed during the labeling procedure and the administration of the labeled leukocytes to the patient. The user should wear waterproof gloves during the entire procedure. The patient's dose should be measured by a suitable radioactivity calibration system immediately before administration. At this time, the leukocyte preparation should be checked for gross clumping and red blood cell contamination.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Indium oxyquinoline in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Indium oxyquinoline in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding FDA-Labeled Use of Indium oxyquinoline in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Indium oxyquinoline in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Indium oxyquinoline in pediatric patients.
Contraindications
- None known.
Warnings
- The content of the vial of indium In 111 oxyquinoline solution is intended only for use in the preparation of indium In 111 oxyquinoline labeled autologous leukocytes, and is not to be administered directly. Autologous leukocyte labeling is not recommended in leukopenic patients because of the small number of available leukocytes.
- Due to radiation exposure, indium In 111 oxyquinoline labeled leukocytes could cause fetal harm when administered to pregnant women. If this radiopharmaceutical is used during pregnancy, the patient should be informed of the potential hazard to the fetus.
- Indium In 111 oxyquinoline labeled autologous leukocytes should be used only when the benefit to be obtained exceeds the risks involved in children under eighteen years of age owing to the high radiation burden and the potential for delayed manifestation of long-term adverse effects.
Precautions
- Clumping of cells may produce focal accumulations of radioactivity in lungs which do not wash out in 24 hours and thus may lead to false positive results. This phenomenon can be detected by imaging the chest immediately after injection.
- The normally high uptake of indium In 111 oxyquinoline labeled leukocytes by spleen and liver may mask inflammatory lesions in these organs. Labeled leukocytes have been observed to accumulate in the colon and accessory spleens of patients with or without disease.
- Chemotaxis of granulocytes deteriorates during storage and loss of chemotaxis may cause false negative scans. The spontaneous release of indium In 111 has been reported to range from about 3% at one hour to 24% at 24 hours. The maximum amount of time recommended between drawing the blood and reinjection should not exceed 5 hours. It is recommended that the labeled cells be used within one hour of preparation, if possible and in no case more than three hours after preparation.
- Plasma and red cell contamination impairs labeling efficiency of leukocytes. Hemolyzed blood in labeled leukocytes may produce heart pool activity and should be avoided.
- Cell aggregates of various degrees have been reported. Cell labeling techniques and standing of cell preparation may be contributing factors.
- Nuclear medicine procedures involving withdrawal and reinjection of blood have the potential for transmission of blood borne pathogens. Procedures should be implemented to avoid administration errors and viral contamination of personnel during blood product labeling. A system of checks similar to the ones used for administering blood transfusions should be routine.
General
- Strict aseptic techniques should be used to maintain sterility throughout the procedures for using this product.
- Do not use after the expiration time and date (5 days after calibration time) stated on the label.
- The contents of the vial are radioactive. Adequate shielding of the preparation must be maintained at all times.
- Indium In 111 oxyquinoline, like other radioactive drugs, must be handled with care and appropriate safety measures should be used to minimize radiation exposure to clinical personnel. Care should also be taken to minimize radiation exposure to the patient consistent with proper patient management.
- Radiopharmaceuticals should be used only by physicians who are qualified by training and experience in the safe use and handling of radionuclides and whose experience and training have been approved by the appropriate governmental agency authorized to license the use of radio-nuclides.
Adverse Reactions
Clinical Trials Experience
- Sensitivity reactions (urticaria) have been reported. The presence of fever may mask pyrogenic reactions from indium In 111 oxyquinoline labeled leukocytes. The possibility of delayed adverse reactions has not been studied.
Postmarketing Experience
There is limited information regarding Postmarketing Experience of Indium oxyquinoline in the drug label.
Drug Interactions
There is limited information regarding Indium oxyquinoline Drug Interactions in the drug label.
Use in Specific Populations
Pregnancy
- Animal reproduction studies have not been conducted with Indium In 111 Oxyquinoline labeled leukocytes. It is also not known whether Indium In 111 Oxyquinoline labeled leukocytes can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity.
- However, Indium Nitrate, a closely related compound, was teratogenic and embryopathic in hamsters. Indium In 111 Oxyquinoline labeled leukocytes should be given to a pregnant woman only if clearly needed.
- Ideally, examinations using radiopharmaceuticals, especially those elective in nature, in women of childbearing capability should be performed during the first few (approximately ten) days following the onset of menses.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Indium oxyquinoline in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Indium oxyquinoline during labor and delivery.
Nursing Mothers
- It is reported that indium 111 is secreted in human milk following administration of indium In 111 labeled leukocytes. Therefore, formula feedings should be substituted for breast feedings.
Pediatric Use
- Safety and effectiveness in pediatric patients below age 18 have not been established
Geriatic Use
- Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Gender
There is no FDA guidance on the use of Indium oxyquinoline with respect to specific gender populations.
Race
There is no FDA guidance on the use of Indium oxyquinoline with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Indium oxyquinoline in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Indium oxyquinoline in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Indium oxyquinoline in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Indium oxyquinoline in patients who are immunocompromised.
Administration and Monitoring
Administration
Monitoring
- Image quality of radiolabeled leukocytes is indicative of efficacy
IV Compatibility
There is limited information regarding IV Compatibility of Indium oxyquinoline in the drug label.
Overdosage
There is limited information regarding Chronic Overdose of Indium oxyquinoline in the drug label.
Pharmacology
Mechanism of Action
- Indium forms a saturated (1:3) complex with oxyquinoline. The complex is neutral and lipid-soluble, which enables it to penetrate the cell membrane. Within the cell, indium becomes firmly attached to cytoplasmic components; the liberated oxyquinoline is released by the cell. It is thought likely that the mechanism of labeling cells with indium In 111 oxyquinoline involves an exchange reaction between the oxyquinoline carrier and subcellular components which chelate indium more strongly than oxyquinoline. The low stability constant of the oxyquinoline complex, estimated at approximately 10, supports this theory.
Structure
- Indium In 111 oxyquinoline (oxine) is a diagnostic radiopharmaceutical intended for radiolabeling autologous leukocytes. It is supplied as a sterile, non-pyrogenic, isotonic aqueous solution with a pH range of 6.5 to 7.5. Each mL of the solution contains 37 MBq, 1 mCi of indium In 111 [no carrier added, >1.85 GBq/µg indium (>50 mCi/µg indium)] at calibration time, 50 µg oxyquinoline, 100 µg polysorbate 80, and 6 mg of HEPES (N-2-hydroxyethyl-piperazine-N'-2-ethane sulfonic acid) buffer in 0.75% sodium chloride solution. The drug is intended for single use only and contains no bacteriostatic agent. The radionuclidic impurity limit for indium 114m is not greater than 37 kBq, 1 µCi of indium 114m per 37 MBq, 1 mCi of indium In 111 at the time of calibration. The radionuclidic composition at expiration time is not less than 99.75% of indium In 111 and not more than 0.25% of indium In 114m/114.
Chemical name: Indium In 111 Oxyquinoline.
- The precise structure of the indium In 111 oxyquinoline complex is unknown at this time. The empirical formula is (C9H6NO)3 In 111.
Pharmacodynamics
There is limited information regarding Pharmacodynamics of Indium oxyquinoline in the drug label.
Pharmacokinetics
- Following the recommended leukocyte cell labeling procedure, approximately 77% of the added indium In 111 oxyquinoline is incorporated in the resulting cell pellet (which represents approximately 3-4 × 108 WBC).
- Cell clumping can occur and was found in about one fifth of the leukocyte preparations examined. The presence of red blood cells or plasma will lead to reduced leukocyte labeling efficiency. Transferrin in plasma competes for indium In 111 oxyquinoline.
- After injection of labeled leukocytes into normal volunteers, about 30% of the dose is taken up by spleen and 30% by liver, reaching a plateau at 2-48 hours after injection. No significant clearance of radioactivity is observed at 72 hours in these two organs. Pulmonary uptake is 4-7.5% at 10 minutes but is lost rapidly; pulmonary radioactivity is usually visible in scans only up to about 4 hours after injection.
- The human biodistribution studies in three normal subjects injected with indium In 111 oxyquinoline labeled leukocytes indicate a biexponential disappearance of indium In 111 from the blood when monitored for up to 72 hours. Between 9.5 to 24.4% of the injected dose remains in whole blood and clears with a biological half-time of 2.8 to 5.5 hours. The remainder (13-18%) clears from blood with a biological half-time of 64 to 116 hours.
- Elimination from the body of injected indium In 111 oxyquinoline is probably mainly through decay to stable cadmium since only a negligible amount (less than 1%) of the dose is excreted in feces and urine in 24 hours.
- Clearance from whole blood and biological distribution can vary considerably with the individual recipient, the condition of the injected cells and labeling techniques used.
- Release of radioactivity from the labeled cells is about 3% at 1 hour and 24% at 24 hours.
- Clearance from liver and spleen, for the purpose of calculating the radiation dose, is assumed to be equal to the physical half-life of indium In 111 (67.2 hours).
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Although earlier studies suggested that oxyquinoline (oxine) might have carcinogenic potential, recent studies have found no evidence of carcinogenicity in either rats or mice given oxyquinoline in feed at concentrations of 1,500 or 3,000 ppm for 103 weeks.
- It has been reported that human lymphocytes labeled with recommended concentrations of indium In 111 oxyquinoline showed chromosome aberrations consisting of gaps, breaks and exchanges that appear to be radiation induced. At 555 kBq/107, 15 µCi/107 lymphocytes 93% of the cells were reported to be abnormal. The oncogenic potential of such lymphocytes has not been studied. It has been reported that the radiation dose to 108 leukocytes is 9 × 104 mGy (0.9 × 104 rads) from 18.5 MBq, 500 µCi.
- Studies have not been performed to evaluate whether indium In 111 oxyquinoline affects fertility in male or female laboratory animals or humans.
Clinical Studies
There is limited information regarding Clinical Studies of Indium oxyquinoline in the drug label.
How Supplied
- Indium In 111 oxyquinoline solution is supplied in a vial as a single use only product containing 37 MBq, 1.0 mCi in 1.0 mL aqueous solution at the calibration date stated on the label. Vials are packaged in individual lead shields.
NDC 17156-021-01
- The contents of the vial are radioactive and adequate shielding and handling precautions must be maintained.
- This preparation is approved for use by persons licensed by the Illinois Emergency Management Agency pursuant to 32 IL. Adm. Code Section 330.260(a) and 335.4010 or equivalent licenses of the Nuclear Regulatory Commission or an Agreement State.
Storage
- Indium In 111 oxyquinoline solution should be stored at room temperature (15-25°C, 59-77°F).
- Indium In 111 oxyquinoline labeled autologous leukocytes should preferably be reinjected within one hour of labeling. The labeled cells may be stored at room temperature (15-25°C, 59-77°F) for up to three hours following completion of the cell labeling procedure. Reinjection of indium In 111 oxyquinoline labeled autologous leukocytes more than 5 hours after initial blood drawing is not recommended.
- Sterile technique must be used throughout the collection, labeling and re-injection procedures.
Images
Drug Images
{{#ask: Page Name::Indium oxyquinoline |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Indium oxyquinoline |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Patient Counseling Information of Indium oxyquinoline in the drug label.
Precautions with Alcohol
- Alcohol-Indium oxyquinoline interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
There is limited information regarding Indium oxyquinoline Brand Names in the drug label.
Look-Alike Drug Names
There is limited information regarding Indium oxyquinoline Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Page Name=Indium oxyquinoline
|Pill Name=No image.jpg
|Drug Name=
|Pill Ingred=|+sep=;
|Pill Imprint=
|Pill Dosage={{{dosageValue}}} {{{dosageUnit}}}
|Pill Color=|+sep=;
|Pill Shape=
|Pill Size (mm)=
|Pill Scoring=
|Pill Image=
|Drug Author=
|NDC=
}}
{{#subobject:
|Label Page=Indium oxyquinoline |Label Name=Oxyquinoline01.png
}}
{{#subobject:
|Label Page=Indium oxyquinoline |Label Name=Oxyquinoline02.png
}}