Hyperoxaluria: Difference between revisions
No edit summary |
Irfan Dotani (talk | contribs) No edit summary |
||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{SI}} | |||
{{CMG}}; {{AE}} | |||
{{Infobox Disease | | {{Infobox Disease | | ||
Name = Hyperoxaluria | | Name = Hyperoxaluria | | ||
| Line 19: | Line 20: | ||
==Overview== | ==Overview== | ||
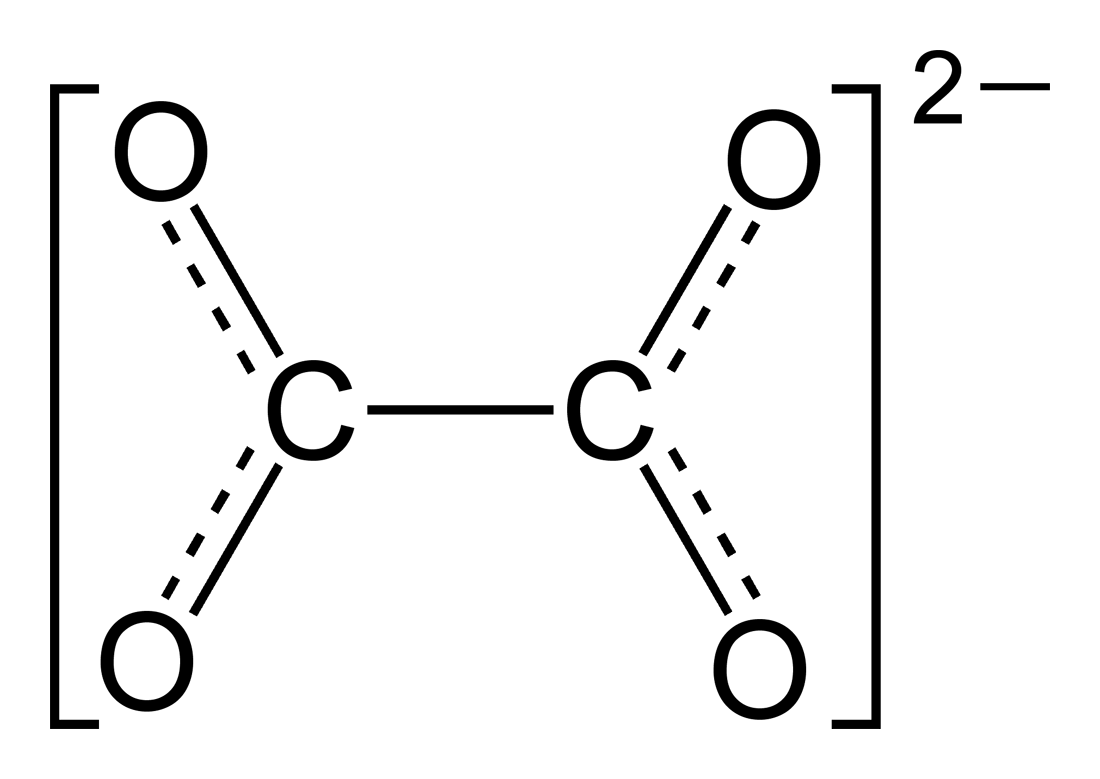
'''Hyperoxaluria''' is an excessive urinary excretion of [[oxalate]]. Individuals with hyperoxaluria often have [[calcium oxalate]] [[kidney stone]]s. It is sometimes called '''Bird's disease''', after [[Golding Bird]], who first described the condition. | '''Hyperoxaluria''' is an excessive urinary excretion of [[oxalate]]. Individuals with hyperoxaluria often have [[calcium oxalate]] [[kidney stone]]s. It is sometimes called '''Bird's disease''', after [[Golding Bird]], who first described the condition. | ||
==Historical Perspective== | |||
==Classification== | |||
===Types=== | |||
* Primary hyperoxaluria | |||
* Enteric hyperoxaluria | |||
* [[Idiopathic]] hyperoxaluria | |||
* [[Oxalate]] poisoning | |||
==Pathophysiology== | |||
===Controversy=== | |||
Perhaps the key difficulty in understanding pathogenesis of primary hyperoxaluria, or more specifically, why AGXT ends up in mitochondria instead of peroxisomes, stems from AGXT's somewhat peculiar evolution. Namely, prior to its current peroxysomal 'destiny', AGXT indeed used to be bound to mitochondria. AGXT's peroxisomal targeting sequence is uniquely specific for mammalian species, suggesting the presence of additional peroxisomal targeting information elsewhere in the AGT molecule. As AGXT was redirected to peroxisomes over the course of evolution, it is plausible that its current aberrant localization to mitochondria owes to some hidden molecular signature in AGXT's spatial configuration unmasked by PH1 mutations affecting the AGXT gene. <!--It is in this sense that we could conditionally understand PH1 as a sort of atavism acting on a molecular level. However, this should be taken as a metaphore with all the caveats of metaphoric thinking applied to science.--> | |||
==Causes== | ==Causes== | ||
Type I (PH1) is associated with [[AGXT]] protein, a key enzyme involved in breakdown of [[oxalate]]. PH1 is also an example of a protein mistargeting disease, wherein AGXT shows a trafficking defect: instead of being trafficked to [[peroxisome]]s, it is targeted to [[mitochondria]], where it is metabolically deficient despite being catalytically active. Type II is associated with [[GRHPR]].<ref name="urlPrimary hyperoxaluria - Genetics Home Reference">{{cite web |url=http://ghr.nlm.nih.gov/condition=primaryhyperoxaluria |title=Primary hyperoxaluria - Genetics Home Reference |format= |work= |accessdate=}}</ref> | Type I (PH1) is associated with [[AGXT]] protein, a key enzyme involved in breakdown of [[oxalate]]. PH1 is also an example of a protein mistargeting disease, wherein AGXT shows a trafficking defect: instead of being trafficked to [[peroxisome]]s, it is targeted to [[mitochondria]], where it is metabolically deficient despite being catalytically active. Type II is associated with [[GRHPR]].<ref name="urlPrimary hyperoxaluria - Genetics Home Reference">{{cite web |url=http://ghr.nlm.nih.gov/condition=primaryhyperoxaluria |title=Primary hyperoxaluria - Genetics Home Reference |format= |work= |accessdate=}}</ref> | ||
It is also a complication of [[jejunoileal bypass]], or in any patient who has lost much of the [[ileum]] with an intact [[Colon (anatomy)|colon]]. This is due to excessive absorption of oxalate from the colon.<ref>Surgery PreTest Self-Assessment and Review, Twelfth Edition</ref> | It is also a complication of [[jejunoileal bypass]], or in any patient who has lost much of the [[ileum]] with an intact [[Colon (anatomy)|colon]]. This is due to excessive absorption of oxalate from the colon.<ref>Surgery PreTest Self-Assessment and Review, Twelfth Edition</ref> | ||
==Differentiating Hyperoxaluria from Other Diseases== | |||
==Epidemiology and Demographics== | |||
==Risk Factors== | |||
==Screening== | |||
==Natural History, Complications, and Prognosis== | |||
==Diagnosis== | |||
===Diagnostic Criteria=== | |||
===History and Symptoms=== | |||
===Physical Examination=== | |||
===Laboratory Findings=== | |||
===Imaging Findings=== | |||
===Other Diagnostic Studies=== | |||
==Treatment== | ==Treatment== | ||
The main therapeutic approach to primary hyperoxaluria is still restricted to symptomatic treatment, i.e. [[kidney transplantation]] once the disease has already reached mature or terminal stages. However, through genomics and proteomics approaches, efforts are currently being made to elucidate the kinetics of AGXT folding which has a direct bearing on its targeting to appropriate subcellular localization. Secondary hyperoxaluria is much more common than primary hyperoxaluria, and should be treated by limiting dietary oxalate and providing calcium supplementation. A child with [[primary hyperoxaluria]] was treated with a liver and kidney transplant.<ref>[http://content.msn.co.in/News/National/NationalHT_090507_0902 India News & Business - MSN India: News, Business, Finance, Sports, Politics & more. - News<!-- Bot generated title -->]</ref> A favorable outcome is more likely if a kidney transplant is complemented by a liver transplant, given the disease originates in the liver. | The main therapeutic approach to primary hyperoxaluria is still restricted to symptomatic treatment, i.e. [[kidney transplantation]] once the disease has already reached mature or terminal stages. However, through genomics and proteomics approaches, efforts are currently being made to elucidate the kinetics of AGXT folding which has a direct bearing on its targeting to appropriate subcellular localization. Secondary hyperoxaluria is much more common than primary hyperoxaluria, and should be treated by limiting dietary oxalate and providing calcium supplementation. A child with [[primary hyperoxaluria]] was treated with a liver and kidney transplant.<ref>[http://content.msn.co.in/News/National/NationalHT_090507_0902 India News & Business - MSN India: News, Business, Finance, Sports, Politics & more. - News<!-- Bot generated title -->]</ref> A favorable outcome is more likely if a kidney transplant is complemented by a liver transplant, given the disease originates in the liver. | ||
===Medical Therapy=== | |||
== | ===Surgery=== | ||
===Prevention=== | |||
== | ==External links== | ||
* Primary | * [http://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=gene&part=ph1 GeneReviews/NIH/NCBI/UW entry on Primary Hyperoxaluria Type 1] | ||
==References== | ==References== | ||
{{reflist}} | {{reflist|2}} | ||
{{Inborn errors of carbohydrate metabolism}} | {{Inborn errors of carbohydrate metabolism}} | ||
{{Abnormal clinical and laboratory findings for urine}} | {{Abnormal clinical and laboratory findings for urine}} | ||
{{DEFAULTSORT:Hyperoxaluria}} | {{DEFAULTSORT:Hyperoxaluria}} | ||
[[Category: | |||
[[Category:Endocrinology]] | |||
{{WS}} | |||
{{WH}} | |||
Latest revision as of 19:35, 22 July 2016
|
WikiDoc Resources for Hyperoxaluria |
|
Articles |
|---|
|
Most recent articles on Hyperoxaluria Most cited articles on Hyperoxaluria |
|
Media |
|
Powerpoint slides on Hyperoxaluria |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Hyperoxaluria at Clinical Trials.gov Trial results on Hyperoxaluria Clinical Trials on Hyperoxaluria at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Hyperoxaluria NICE Guidance on Hyperoxaluria
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Hyperoxaluria Discussion groups on Hyperoxaluria Patient Handouts on Hyperoxaluria Directions to Hospitals Treating Hyperoxaluria Risk calculators and risk factors for Hyperoxaluria
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Hyperoxaluria |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief:
| Hyperoxaluria | |
 | |
|---|---|
| Oxalate | |
| ICD-10 | E74.8 |
| ICD-9 | 271.8 |
| DiseasesDB | 31642 |
| eMedicine | med/3027 |
| MeSH | D006959 |
Overview
Hyperoxaluria is an excessive urinary excretion of oxalate. Individuals with hyperoxaluria often have calcium oxalate kidney stones. It is sometimes called Bird's disease, after Golding Bird, who first described the condition.
Historical Perspective
Classification
Types
- Primary hyperoxaluria
- Enteric hyperoxaluria
- Idiopathic hyperoxaluria
- Oxalate poisoning
Pathophysiology
Controversy
Perhaps the key difficulty in understanding pathogenesis of primary hyperoxaluria, or more specifically, why AGXT ends up in mitochondria instead of peroxisomes, stems from AGXT's somewhat peculiar evolution. Namely, prior to its current peroxysomal 'destiny', AGXT indeed used to be bound to mitochondria. AGXT's peroxisomal targeting sequence is uniquely specific for mammalian species, suggesting the presence of additional peroxisomal targeting information elsewhere in the AGT molecule. As AGXT was redirected to peroxisomes over the course of evolution, it is plausible that its current aberrant localization to mitochondria owes to some hidden molecular signature in AGXT's spatial configuration unmasked by PH1 mutations affecting the AGXT gene.
Causes
Type I (PH1) is associated with AGXT protein, a key enzyme involved in breakdown of oxalate. PH1 is also an example of a protein mistargeting disease, wherein AGXT shows a trafficking defect: instead of being trafficked to peroxisomes, it is targeted to mitochondria, where it is metabolically deficient despite being catalytically active. Type II is associated with GRHPR.[1] It is also a complication of jejunoileal bypass, or in any patient who has lost much of the ileum with an intact colon. This is due to excessive absorption of oxalate from the colon.[2]
Differentiating Hyperoxaluria from Other Diseases
Epidemiology and Demographics
Risk Factors
Screening
Natural History, Complications, and Prognosis
Diagnosis
Diagnostic Criteria
History and Symptoms
Physical Examination
Laboratory Findings
Imaging Findings
Other Diagnostic Studies
Treatment
The main therapeutic approach to primary hyperoxaluria is still restricted to symptomatic treatment, i.e. kidney transplantation once the disease has already reached mature or terminal stages. However, through genomics and proteomics approaches, efforts are currently being made to elucidate the kinetics of AGXT folding which has a direct bearing on its targeting to appropriate subcellular localization. Secondary hyperoxaluria is much more common than primary hyperoxaluria, and should be treated by limiting dietary oxalate and providing calcium supplementation. A child with primary hyperoxaluria was treated with a liver and kidney transplant.[3] A favorable outcome is more likely if a kidney transplant is complemented by a liver transplant, given the disease originates in the liver.
Medical Therapy
Surgery
Prevention
External links
References
- ↑ "Primary hyperoxaluria - Genetics Home Reference".
- ↑ Surgery PreTest Self-Assessment and Review, Twelfth Edition
- ↑ India News & Business - MSN India: News, Business, Finance, Sports, Politics & more. - News