Hypercholesterolemia NCEP ATP III guidelines: Difference between revisions
Rim Halaby (talk | contribs) (Rim Halaby moved page Hypercholesterolemia NCEP ATP III guidelines to High cholesterol medical therapy) |
Gerald Chi (talk | contribs) mNo edit summary |
||
| Line 1: | Line 1: | ||
# | {{Hypercholesterolemia}} | ||
'''Editor-In-Chief:''' [[C. Michael Gibson, M.S., M.D.]] [mailto:charlesmichaelgibson@gmail.com] Phone:617-632-7753; '''Associate Editor(s)-In-Chief:''' [[Kashish Goel|Kashish Goel, M.D.]] | |||
==Overview== | |||
National Cholesterol Education Program Adult Treatment Panel (NCEP ATP) III issued guidelines for detection, evaluation, and treatment of high blood cholesterol in adults in 2001. | |||
==ATP I== | |||
ATP I provided an outline for primary prevention of [[CHD]] in those with [[LDL]] > 160 mg/dL. | |||
==ATP II== | |||
ATP II added an important approach of intensive management of [[LDL]] in patients with established [[CHD]] and established a goal of lowering LDL to ≤ 100 mg/dL. | |||
==ATP III== | |||
ATP III guidelines | |||
* Elevated [[diabetes]] to the status of a [[CHD]] risk equivalent | |||
* Used [[Framingham risk score]] for risk assessment | |||
* Identified secondary targets such as the [[metabolic syndrome]] | |||
* Modified the LDL goals | |||
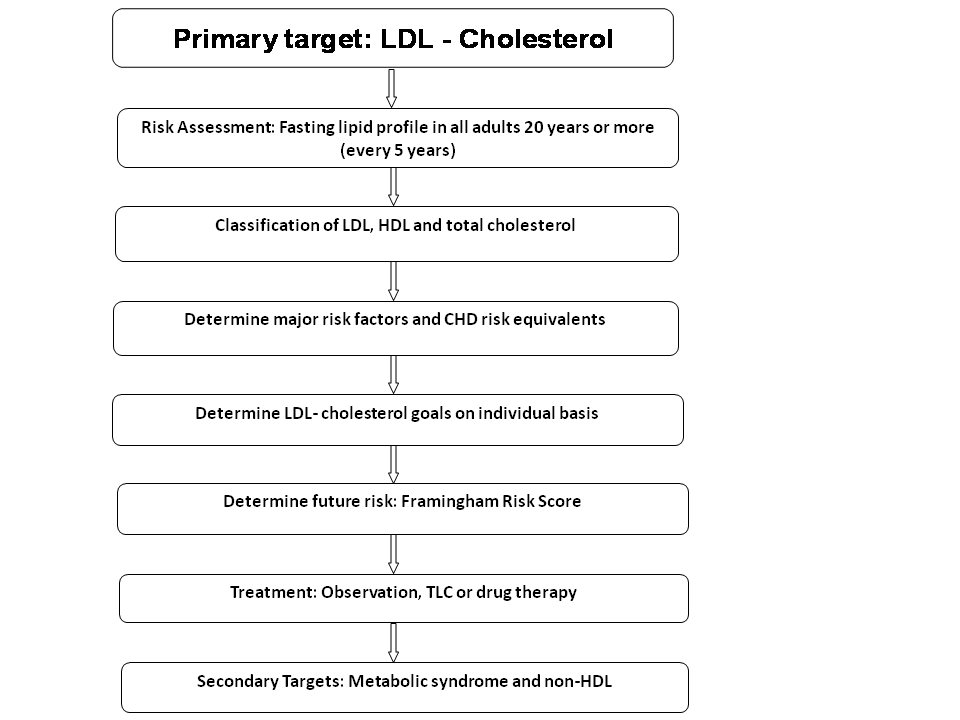
* An overview of step-wise approach in ATP III is provided in the following flowchart. Individual points are discussed below. | |||
[[Image:NCEP guidelines.png|550px]] | |||
Adapted from NCEP ATP III guidelines<ref name="pmid12485966">{{cite journal| author=National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III)| title=Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. | journal=Circulation | year= 2002 | volume= 106 | issue= 25 | pages= 3143-421 | pmid=12485966 | doi= | pmc= | url= }} </ref> | |||
==Primary target== | |||
Multiple levels of evidence including experimental animals, epidemiologic studies and controlled clinical trials have shown a causal relationship between cardiovascular disease and elevated [[LDL]] - cholesterol. NCEP recommends "LDL cholesterol should continue to be the primary target of cholesterol lowering therapy."<ref name="pmid12485966">{{cite journal|author=National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III)|title=Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. | journal=Circulation | year= 2002 | volume= 106 | issue= 25 | pages= 3143-421 | pmid=12485966 | doi= | pmc= | url= }} </ref><ref name="pmid7566020">{{cite journal| author=Shepherd J, Cobbe SM, Ford I, Isles CG, Lorimer AR, MacFarlane PW et al.| title=Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study Group. | journal=N Engl J Med | year= 1995 | volume= 333 | issue= 20 | pages= 1301-7 | pmid=7566020 |doi=10.1056/NEJM199511163332001 | pmc= | url= }} </ref><ref name="pmid9613910">{{cite journal| author=Downs JR, Clearfield M, Weis S, Whitney E, Shapiro DR, Beere PA et al.|title=Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. | journal=JAMA | year= 1998 | volume= 279 | issue= 20 | pages= 1615-22 | pmid=9613910 | doi= | pmc= |url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9613910 }} </ref><ref name="pmid15007110">{{cite journal|author=Cannon CP, Braunwald E, McCabe CH, Rader DJ, Rouleau JL, Belder R et al.| title=Intensive versus moderate lipid lowering with statins after acute coronary syndromes. |journal=N Engl J Med | year= 2004 | volume= 350 | issue= 15 | pages= 1495-504 | pmid=15007110 | doi=10.1056/NEJMoa040583 | pmc= |url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15007110 }} [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15341453 Review in: ACP J Club. 2004 Sep-Oct;141(2):33]</ref> | |||
==Risk assessment== | |||
# All individuals above the age of 20 years should have a fasting lipid profile, once every 5 years. | |||
# If the testing sample was non-fasting, only values of total cholesterol (TC) and [[HDL]] should be considered evaluable. | |||
# If abnormal (TC > 200 mg/dL or HDL < 40 mg/dL), then a repeat fasting lipoprotein profile should be done. | |||
==Classification== | |||
[[LDL]] Cholesterol | |||
* <100: Optimal | |||
* 100-129: Near optimal/above optimal | |||
* 130-159: Borderline high | |||
* 160-189: High | |||
* ≥ 190: Very high | |||
Total Cholesterol | |||
* <200: Desirable | |||
* 200-239: Borderline high | |||
* ≥ 240: High | |||
HDL Cholesterol | |||
* <40: Low | |||
* ≥ 60: High | |||
==Risk factors== | |||
Three categories of risk factors modify the goal LDL in each individual: | |||
===Major risk factors=== | |||
*[[Cigarette smoking]] | |||
*[[Hypertension]] (BP>= 140/90 mmHg or on antihypertensive medication) | |||
*Low [[HDL]] (<40 mg/dL) | |||
*Family history of premature [[CHD]] (male first-degree relative <55 years; female first-degree relative <65 years) | |||
*Age (men >=45 years; women >=55 years) | |||
===CHD risk equivalents=== | |||
*[[Peripheral arterial disease]] | |||
*[[Abdominal aortic aneurysm]] | |||
*[[Carotid artery disease]] ([[transient ischemic attacks]] or [[stroke]] of carotid origin or >50% obstruction of a carotid artery) | |||
*[[Diabetes]] | |||
* The presence of > 2 CHD risk factors is associated with a 10-year risk for coronary heart disease events of >20% | |||
===Coronary Heart Disease=== | |||
* [[Myocardial infarction]] | |||
* [[Unstable angina]] | |||
* [[Stable angina]] | |||
* Coronary artery revascularization procedures such as [[angioplasty]] or bypass surgery | |||
* Evidence of clinically significant myocardial ischemia | |||
==Future risk== | |||
Future 10-year risk should be calculated using online calculators (for eg:http://hp2010.nhlbihin.net/atpiii/calculator.asp?usertype=prof) to help guide the target [[LDL]] goal. This is based on Framingham risk score. | |||
==LDL goal== | |||
:'''LDL goals''' | |||
:{| class="wikitable" border="1" | |||
|+ | |||
! Risk Category !! LDL-C goal !! Initiate TLC !!Consider drug therapy | |||
|- | |||
| ''High Risk''<br>CHD or CHD risk equivalents (10-year risk >20%) || < 100 mg/dL (optional goal:<70 mg/dL) || ≥ 100 mg/dL || <100 mg/dL | |||
|- | |||
| ''Moderately high risk''<br>2+ risk factors (10-year risk 10% to 20%) || <130 mg/dL || ≥ 130 mg/dL || 100-129 mg/dL | |||
|- | |||
| ''Moderate risk''<br>2+ risk factors (10-year risk <10%) || <130 mg/dL || ≥ 130 mg/dL || ≥ 160 mg/dL | |||
|- | |||
| ''Lower risk''<br>0-1 risk factors || <160 mg/dL || ≥ 160 mg/dL || 160-189 mg/dL | |||
|} | |||
ATP III LDL-C Goals and Cut-points for therapeutic lifestyle changes (TLC) and Drug Therapy<ref name="pmid15249516">{{cite journal| author=Grundy SM, Cleeman JI, Merz CN, Brewer HB, Clark LT, Hunninghake DB et al.| title=Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. |journal=Circulation | year= 2004 | volume= 110 | issue= 2 | pages= 227-39 | pmid=15249516 | doi=10.1161/01.CIR.0000133317.49796.0E | pmc= |url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15249516 }} </ref>) | |||
NCEP updated their 2001 recommendations, based on new clinical trials evidence. '''''An optional [[LDL]] goal of <70 mg/dL has been suggested in high-risk individuals, based recent data.''''' However, this has not been incorporated into guidelines as yet. The National Heart, Lung, and Blood Institute is leading the development of an updated cholesterol guidleines (ATP IV) which are expected to be released in 2012<ref>http://www.nhlbi.nih.gov/guidelines/cholesterol/atp4/index.htm</ref>. | |||
==References== | |||
{{Reflist|2}} | |||
[[Category:Disease]] | |||
[[Category:Cardiology]] | |||
[[Category:Up-To-Date]] | |||
[[Category:Up-To-Date cardiology]] | |||
{{WikiDoc Help Menu}} | |||
{{WikiDoc Sources}} | |||
Latest revision as of 17:16, 13 November 2013
Template:Hypercholesterolemia Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Phone:617-632-7753; Associate Editor(s)-In-Chief: Kashish Goel, M.D.
Overview
National Cholesterol Education Program Adult Treatment Panel (NCEP ATP) III issued guidelines for detection, evaluation, and treatment of high blood cholesterol in adults in 2001.
ATP I
ATP I provided an outline for primary prevention of CHD in those with LDL > 160 mg/dL.
ATP II
ATP II added an important approach of intensive management of LDL in patients with established CHD and established a goal of lowering LDL to ≤ 100 mg/dL.
ATP III
ATP III guidelines
- Elevated diabetes to the status of a CHD risk equivalent
- Used Framingham risk score for risk assessment
- Identified secondary targets such as the metabolic syndrome
- Modified the LDL goals
- An overview of step-wise approach in ATP III is provided in the following flowchart. Individual points are discussed below.
Adapted from NCEP ATP III guidelines[1]
Primary target
Multiple levels of evidence including experimental animals, epidemiologic studies and controlled clinical trials have shown a causal relationship between cardiovascular disease and elevated LDL - cholesterol. NCEP recommends "LDL cholesterol should continue to be the primary target of cholesterol lowering therapy."[1][2][3][4]
Risk assessment
- All individuals above the age of 20 years should have a fasting lipid profile, once every 5 years.
- If the testing sample was non-fasting, only values of total cholesterol (TC) and HDL should be considered evaluable.
- If abnormal (TC > 200 mg/dL or HDL < 40 mg/dL), then a repeat fasting lipoprotein profile should be done.
Classification
LDL Cholesterol
- <100: Optimal
- 100-129: Near optimal/above optimal
- 130-159: Borderline high
- 160-189: High
- ≥ 190: Very high
Total Cholesterol
- <200: Desirable
- 200-239: Borderline high
- ≥ 240: High
HDL Cholesterol
- <40: Low
- ≥ 60: High
Risk factors
Three categories of risk factors modify the goal LDL in each individual:
Major risk factors
- Cigarette smoking
- Hypertension (BP>= 140/90 mmHg or on antihypertensive medication)
- Low HDL (<40 mg/dL)
- Family history of premature CHD (male first-degree relative <55 years; female first-degree relative <65 years)
- Age (men >=45 years; women >=55 years)
CHD risk equivalents
- Peripheral arterial disease
- Abdominal aortic aneurysm
- Carotid artery disease (transient ischemic attacks or stroke of carotid origin or >50% obstruction of a carotid artery)
- Diabetes
- The presence of > 2 CHD risk factors is associated with a 10-year risk for coronary heart disease events of >20%
Coronary Heart Disease
- Myocardial infarction
- Unstable angina
- Stable angina
- Coronary artery revascularization procedures such as angioplasty or bypass surgery
- Evidence of clinically significant myocardial ischemia
Future risk
Future 10-year risk should be calculated using online calculators (for eg:http://hp2010.nhlbihin.net/atpiii/calculator.asp?usertype=prof) to help guide the target LDL goal. This is based on Framingham risk score.
LDL goal
- LDL goals
Risk Category LDL-C goal Initiate TLC Consider drug therapy High Risk
CHD or CHD risk equivalents (10-year risk >20%)< 100 mg/dL (optional goal:<70 mg/dL) ≥ 100 mg/dL <100 mg/dL Moderately high risk
2+ risk factors (10-year risk 10% to 20%)<130 mg/dL ≥ 130 mg/dL 100-129 mg/dL Moderate risk
2+ risk factors (10-year risk <10%)<130 mg/dL ≥ 130 mg/dL ≥ 160 mg/dL Lower risk
0-1 risk factors<160 mg/dL ≥ 160 mg/dL 160-189 mg/dL
ATP III LDL-C Goals and Cut-points for therapeutic lifestyle changes (TLC) and Drug Therapy[5])
NCEP updated their 2001 recommendations, based on new clinical trials evidence. An optional LDL goal of <70 mg/dL has been suggested in high-risk individuals, based recent data. However, this has not been incorporated into guidelines as yet. The National Heart, Lung, and Blood Institute is leading the development of an updated cholesterol guidleines (ATP IV) which are expected to be released in 2012[6].
References
- ↑ 1.0 1.1 National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) (2002). "Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report". Circulation. 106 (25): 3143–421. PMID 12485966.
- ↑ Shepherd J, Cobbe SM, Ford I, Isles CG, Lorimer AR, MacFarlane PW; et al. (1995). "Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study Group". N Engl J Med. 333 (20): 1301–7. doi:10.1056/NEJM199511163332001. PMID 7566020.
- ↑ Downs JR, Clearfield M, Weis S, Whitney E, Shapiro DR, Beere PA; et al. (1998). "Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study". JAMA. 279 (20): 1615–22. PMID 9613910.
- ↑ Cannon CP, Braunwald E, McCabe CH, Rader DJ, Rouleau JL, Belder R; et al. (2004). "Intensive versus moderate lipid lowering with statins after acute coronary syndromes". N Engl J Med. 350 (15): 1495–504. doi:10.1056/NEJMoa040583. PMID 15007110. Review in: ACP J Club. 2004 Sep-Oct;141(2):33
- ↑ Grundy SM, Cleeman JI, Merz CN, Brewer HB, Clark LT, Hunninghake DB; et al. (2004). "Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines". Circulation. 110 (2): 227–39. doi:10.1161/01.CIR.0000133317.49796.0E. PMID 15249516.
- ↑ http://www.nhlbi.nih.gov/guidelines/cholesterol/atp4/index.htm