Hiatus hernia pathophysiology: Difference between revisions
No edit summary |
m (Bot: Removing from Primary care) |
||
| (7 intermediate revisions by 2 users not shown) | |||
| Line 4: | Line 4: | ||
{{CMG}}; {{AE}} {{ADS}} | {{CMG}}; {{AE}} {{ADS}} | ||
==Overview== | ==Overview== | ||
It is | It is understood that hiatus hernia is the result of either decreased [[elastin]] of phrenoesophageal membrane due to aging or imbalance in pressure gradient between intra-abdominal pressure and intra-thoracic pressure leading to the esophagogastric junction being displaced into normal hiatus. A rise in intra-abdominal pressure and lower thoracic pressure can cause hernia. Occasionally, esophageal shortening pulls the junction into the hiatus. This physiological shortening may occur as a normal response to [[swallowing]]. The LES is shorter and weaker in large hiatus hernia and have severe reflux symptoms and trauma. Paraesophageal hernia are less common and have lower incidence of [[gastroesophageal reflux disease]]. | ||
== Pathophysiology == | |||
=== Anatomy and physiology === | |||
*[[Lower esophageal sphincter]] (LES) is the group of [[smooth muscles]] in the distal [[esophagus]] at the [[gastroesophageal junction]]. | |||
[ | * LES prevents the reflux of gastric contents into [[esophagus]]. | ||
* The mechanisms or structures preventing the reflux include: | |||
**Angle of His: Anhle of his is the angle between the [[cardia]] of [[stomach]] and distal portion of [[esophagus]]. It functions as a valve or flap. | |||
**Diaphragmatic [[crura]] | |||
**High LES pressure as compared to intraabdominal pressure | |||
The | |||
** | |||
**Diaphragmatic crura | |||
**LES pressure as compared to intraabdominal pressure | |||
**Phrenoesophageal membrane | **Phrenoesophageal membrane | ||
*Phrenoesophageal ligament | *Phrenoesophageal ligament or membrane is fibrous elastic connective tissue arising from [[Crura of the diaphragm|crura]] and inserts circumferentially into [[esophageal]] [[muscles]]. | ||
*It maintains and support LES by anchoring it during [[peristalsis]]. | *It maintains and support LES by anchoring it during [[peristalsis]]. | ||
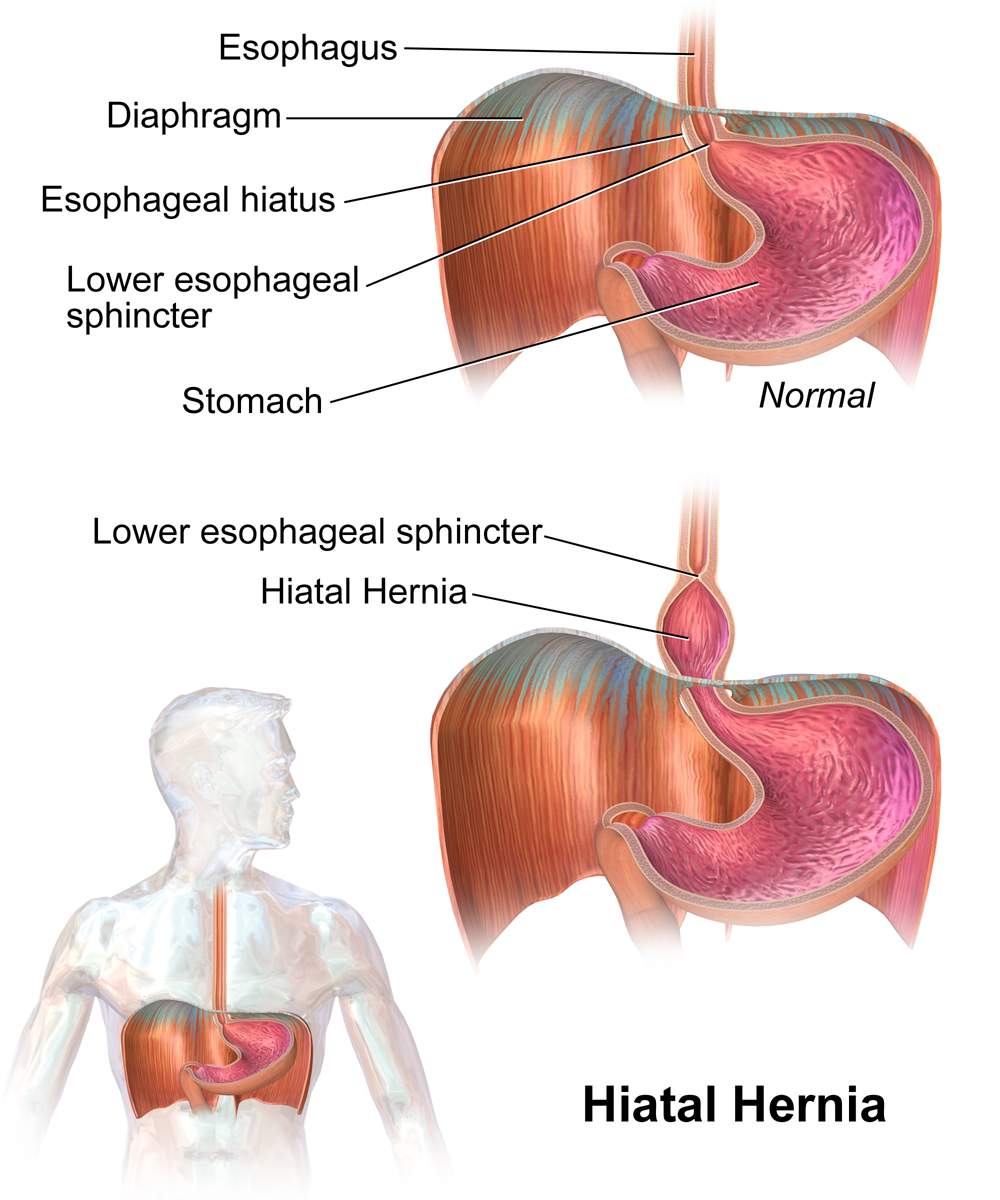
[[File:Hiatal Hernia.png|thumb|center|250px|Hiatal Hernia By BruceBlaus<ref>- Own work, CC BY-SA 4.0, https://commons.wikimedia.org/w/index.php?curid=44924605</ref>]] | [[File:Hiatal Hernia.png|thumb|center|250px|Hiatal Hernia By BruceBlaus<ref>- Own work, CC BY-SA 4.0, https://commons.wikimedia.org/w/index.php?curid=44924605</ref>]] | ||
=== Pathogenesis === | === Pathogenesis === | ||
* | * The parts of [[diaphragm]] involved in the pathophysiology of the hiatus hernia include:<ref name="pmid15836451">{{cite journal |vauthors=Boeckxstaens GE |title=The lower oesophageal sphincter |journal=Neurogastroenterol. Motil. |volume=17 Suppl 1 |issue= |pages=13–21 |year=2005 |pmid=15836451 |doi=10.1111/j.1365-2982.2005.00661.x |url=}}</ref><ref name="pmid12180879">{{cite journal |vauthors=Sivacolundhu RK, Read RA, Marchevsky AM |title=Hiatal hernia controversies--a review of pathophysiology and treatment options |journal=Aust. Vet. J. |volume=80 |issue=1-2 |pages=48–53 |year=2002 |pmid=12180879 |doi= |url=}}</ref> | ||
**Crura (crus of diaphragm) | **[[Crura]] ([[crus of diaphragm]]) | ||
**Esophageal hiatus (opening in [[diaphragm]] for [[esophagus]] at T10) | **[[Esophageal hiatus]] (opening in [[diaphragm]] for [[esophagus]] at T10) | ||
*It is understood that hiatus hernia is the result of either:<ref name="pmid10075953">{{cite journal |vauthors=Kahrilas PJ, Lin S, Chen J, Manka M |title=The effect of hiatus hernia on gastro-oesophageal junction pressure |journal=Gut |volume=44 |issue=4 |pages=476–82 |year=1999 |pmid=10075953 |pmc=1727465 |doi= |url=}}</ref> | *It is understood that hiatus hernia is the result of either:<ref name="pmid10075953">{{cite journal |vauthors=Kahrilas PJ, Lin S, Chen J, Manka M |title=The effect of hiatus hernia on gastro-oesophageal junction pressure |journal=Gut |volume=44 |issue=4 |pages=476–82 |year=1999 |pmid=10075953 |pmc=1727465 |doi= |url=}}</ref> | ||
**Decreased elastin of phrenoesophageal membrane due to aging | **Decreased [[elastin]] of phrenoesophageal membrane due to aging<ref name="pmid4734411">{{cite journal |vauthors=Wolf BS |title=Sliding hiatal hernia: the need for redefinition |journal=Am J Roentgenol Radium Ther Nucl Med |volume=117 |issue=2 |pages=231–47 |year=1973 |pmid=4734411 |doi= |url=}}</ref><ref name="pmid98978">{{cite journal |vauthors=Friedland GW |title=Progress in radiology: historical review of the changing concepts of lower esophageal anatomy: 430 B.C.--1977 |journal=AJR Am J Roentgenol |volume=131 |issue=3 |pages=373–8 |year=1978 |pmid=98978 |doi=10.2214/ajr.131.3.373 |url=}}</ref> | ||
** | **Imbalance in pressure gradient between intra-abdominal pressure and intra-thoracic pressure leading to the esophagogastric junction being displaced into normal hiatus.A rise in intraabdominal pressure and fall in intra-thoracic pressure may lead to development of hernia.<ref name="MenezesHerbella2017">{{cite journal|last1=Menezes|first1=Mariano A.|last2=Herbella|first2=Fernando A. M.|title=Pathophysiology of Gastroesophageal Reflux Disease|journal=World Journal of Surgery|volume=41|issue=7|year=2017|pages=1666–1671|issn=0364-2313|doi=10.1007/s00268-017-3952-4}}</ref> | ||
***The causes of increased | ***The causes of increased intra-abdominal pressure that may lead to hiatus hernia include:<ref>https://my.clevelandclinic.org/health/diseases/8098-hiatal-hernia</ref> | ||
****Coughing | ****[[Coughing]] | ||
****[[Vomiting]] | ****[[Vomiting]] | ||
****Heavy lifting | ****Heavy lifting | ||
| Line 51: | Line 38: | ||
****[[Pregnancy]] | ****[[Pregnancy]] | ||
****Physical strain | ****Physical strain | ||
** | **Occasionally, esophageal shortening pulls the junction into the hiatus. This physiological shortening may occur as a normal response to swallowing.<ref name="pmid10718444">{{cite journal |vauthors=Christensen J, Miftakhov R |title=Hiatus hernia: a review of evidence for its origin in esophageal longitudinal muscle dysfunction |journal=Am. J. Med. |volume=108 Suppl 4a |issue= |pages=3S–7S |year=2000 |pmid=10718444 |doi= |url=}}</ref>The LES is shorter and weaker in large hiatus hernia and have severe reflux symptoms.<ref name="pmid8554137">{{cite journal |vauthors=Patti MG, Goldberg HI, Arcerito M, Bortolasi L, Tong J, Way LW |title=Hiatal hernia size affects lower esophageal sphincter function, esophageal acid exposure, and the degree of mucosal injury |journal=Am. J. Surg. |volume=171 |issue=1 |pages=182–6 |year=1996 |pmid=8554137 |doi=10.1016/S0002-9610(99)80096-8 |url=}}</ref> | ||
**Trauma | **Trauma | ||
*The symptoms in hiatus hernia are the result of reflux esophagitis and the mechanisms involved | *The symptoms in hiatus hernia are the result of reflux esophagitis and the mechanisms involved include:<ref name="pmid10075953">{{cite journal |vauthors=Kahrilas PJ, Lin S, Chen J, Manka M |title=The effect of hiatus hernia on gastro-oesophageal junction pressure |journal=Gut |volume=44 |issue=4 |pages=476–82 |year=1999 |pmid=10075953 |pmc=1727465 |doi= |url=}}</ref> | ||
*#Low resting LES pressure | *#Low resting LES pressure | ||
*#Prolonged time taken to clear acid | *#Prolonged time taken to clear acid | ||
| Line 59: | Line 46: | ||
*#Transient LES relaxation which occurs more frequently in hiatus hernia | *#Transient LES relaxation which occurs more frequently in hiatus hernia | ||
*The pathophysiology of hiatus hernia depends on the histological subtype:<ref name="pmid18656819">{{cite journal |vauthors=Kahrilas PJ, Kim HC, Pandolfino JE |title=Approaches to the diagnosis and grading of hiatal hernia |journal=Best Pract Res Clin Gastroenterol |volume=22 |issue=4 |pages=601–16 |year=2008 |pmid=18656819 |pmc=2548324 |doi=10.1016/j.bpg.2007.12.007 |url=}}</ref> | *The pathophysiology of hiatus hernia depends on the histological subtype:<ref name="pmid18656819">{{cite journal |vauthors=Kahrilas PJ, Kim HC, Pandolfino JE |title=Approaches to the diagnosis and grading of hiatal hernia |journal=Best Pract Res Clin Gastroenterol |volume=22 |issue=4 |pages=601–16 |year=2008 |pmid=18656819 |pmc=2548324 |doi=10.1016/j.bpg.2007.12.007 |url=}}</ref> | ||
**Paraesophageal hernia are less common and have | **Paraesophageal hernia are less common and have lower incidence of [[gastroesophageal reflux disease]]. | ||
**The initial clinical | **The initial clinical presentation including [[dysphagia]], postprandial [[nausea and vomiting]] are result of impaired gastric emptying due to mechanical obstruction. | ||
**It enlarges with time and symptoms are related to the abnormal | **It enlarges with time and results in symptoms are related to the abnormal intra-thoracic location of the stomach. | ||
**The gastrosplenic and gastrocolic | **The [[Gastrosplenic ligament|gastrosplenic]] and [[gastrocolic ligament]] are laxed. | ||
*The hiatus hernia reduces LES sphincter.<ref name="pmid10075953">{{cite journal |vauthors=Kahrilas PJ, Lin S, Chen J, Manka M |title=The effect of hiatus hernia on gastro-oesophageal junction pressure |journal=Gut |volume=44 |issue=4 |pages=476–82 |year=1999 |pmid=10075953 |pmc=1727465 |doi= |url=}}</ref> | *The hiatus hernia reduces LES sphincter.<ref name="pmid10075953">{{cite journal |vauthors=Kahrilas PJ, Lin S, Chen J, Manka M |title=The effect of hiatus hernia on gastro-oesophageal junction pressure |journal=Gut |volume=44 |issue=4 |pages=476–82 |year=1999 |pmid=10075953 |pmc=1727465 |doi= |url=}}</ref> | ||
| Line 73: | Line 60: | ||
==Associated Conditions== | ==Associated Conditions== | ||
Conditions associated with hiatus hernia include: | |||
*[[Gastroesophageal reflux disease]]<ref name="pmid15638947">{{cite journal |vauthors=Gatopoulou A, Mimidis K, Giatromanolaki A, Papadopoulos V, Polychronidis A, Lyratzopoulos N, Sivridis E, Minopoulos G |title=Impact of hiatal hernia on histological pattern of non-erosive reflux disease |journal=BMC Gastroenterol |volume=5 |issue= |pages=2 |year=2005 |pmid=15638947 |pmc=546187 |doi=10.1186/1471-230X-5-2 |url=}}</ref> | *[[Gastroesophageal reflux disease]]<ref name="pmid15638947">{{cite journal |vauthors=Gatopoulou A, Mimidis K, Giatromanolaki A, Papadopoulos V, Polychronidis A, Lyratzopoulos N, Sivridis E, Minopoulos G |title=Impact of hiatal hernia on histological pattern of non-erosive reflux disease |journal=BMC Gastroenterol |volume=5 |issue= |pages=2 |year=2005 |pmid=15638947 |pmc=546187 |doi=10.1186/1471-230X-5-2 |url=}}</ref> | ||
*[[Esophagal ring]]<ref name=":0">{{cite book | last = Haber | first = Meryl | title = Differential diagnosis in surgical pathology | publisher = Saunders | location = Philadelphia | year = 2002 | isbn = 9780721690537 }}</ref> | *[[Esophagal ring]]<ref name=":0">{{cite book | last = Haber | first = Meryl | title = Differential diagnosis in surgical pathology | publisher = Saunders | location = Philadelphia | year = 2002 | isbn = 9780721690537 }}</ref> | ||
| Line 81: | Line 69: | ||
[[File:Hiatus-hernia.jpg|thumb|center|200 px| Gastroscopy showing Hiatus hernia- By Adamantios <ref>CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=1784490</ref>]] | [[File:Hiatus-hernia.jpg|thumb|center|200 px| Gastroscopy showing Hiatus hernia- By Adamantios <ref>CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=1784490</ref>]] | ||
*On gross pathology, | *On gross pathology, characteristic findings of hiatus hernia include:<ref name=":0" /> | ||
**Herniated portion gets dilated and undergo ischemic changes | **Herniated portion gets dilated and undergo ischemic changes | ||
**Ischemic necrosis can be seen | **Ischemic necrosis can be seen | ||
==Microscopic Pathology== | ==Microscopic Pathology== | ||
*On microscopic histopathological analysis, variable chronic inflammation, ischemia and necrosis | *On microscopic histopathological analysis, variable [[chronic inflammation]], [[ischemia]] and [[necrosis]] may be seen in hiatus hernia.<ref name=":0" /> | ||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
[[Category: | |||
[[Category:Surgery]] | |||
[[Category:Gastroenterology]] | |||
[[Category:Up-To-Date]] | |||
[[Category:Disease]] | [[Category:Disease]] | ||
Latest revision as of 22:10, 29 July 2020
|
Hiatus Hernia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Hiatus hernia pathophysiology On the Web |
|
American Roentgen Ray Society Images of Hiatus hernia pathophysiology |
|
Risk calculators and risk factors for Hiatus hernia pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Amandeep Singh M.D.[2]
Overview
It is understood that hiatus hernia is the result of either decreased elastin of phrenoesophageal membrane due to aging or imbalance in pressure gradient between intra-abdominal pressure and intra-thoracic pressure leading to the esophagogastric junction being displaced into normal hiatus. A rise in intra-abdominal pressure and lower thoracic pressure can cause hernia. Occasionally, esophageal shortening pulls the junction into the hiatus. This physiological shortening may occur as a normal response to swallowing. The LES is shorter and weaker in large hiatus hernia and have severe reflux symptoms and trauma. Paraesophageal hernia are less common and have lower incidence of gastroesophageal reflux disease.
Pathophysiology
Anatomy and physiology
- Lower esophageal sphincter (LES) is the group of smooth muscles in the distal esophagus at the gastroesophageal junction.
- LES prevents the reflux of gastric contents into esophagus.
- The mechanisms or structures preventing the reflux include:
- Phrenoesophageal ligament or membrane is fibrous elastic connective tissue arising from crura and inserts circumferentially into esophageal muscles.
- It maintains and support LES by anchoring it during peristalsis.
Pathogenesis
- The parts of diaphragm involved in the pathophysiology of the hiatus hernia include:[2][3]
- Crura (crus of diaphragm)
- Esophageal hiatus (opening in diaphragm for esophagus at T10)
- It is understood that hiatus hernia is the result of either:[4]
- Decreased elastin of phrenoesophageal membrane due to aging[5][6]
- Imbalance in pressure gradient between intra-abdominal pressure and intra-thoracic pressure leading to the esophagogastric junction being displaced into normal hiatus.A rise in intraabdominal pressure and fall in intra-thoracic pressure may lead to development of hernia.[7]
- Occasionally, esophageal shortening pulls the junction into the hiatus. This physiological shortening may occur as a normal response to swallowing.[9]The LES is shorter and weaker in large hiatus hernia and have severe reflux symptoms.[10]
- Trauma
- The symptoms in hiatus hernia are the result of reflux esophagitis and the mechanisms involved include:[4]
- Low resting LES pressure
- Prolonged time taken to clear acid
- Delayed gastric emptying
- Transient LES relaxation which occurs more frequently in hiatus hernia
- The pathophysiology of hiatus hernia depends on the histological subtype:[11]
- Paraesophageal hernia are less common and have lower incidence of gastroesophageal reflux disease.
- The initial clinical presentation including dysphagia, postprandial nausea and vomiting are result of impaired gastric emptying due to mechanical obstruction.
- It enlarges with time and results in symptoms are related to the abnormal intra-thoracic location of the stomach.
- The gastrosplenic and gastrocolic ligament are laxed.
- The hiatus hernia reduces LES sphincter.[4]
Video shows formation of hiatus hernia
{{#ev:youtube|vYP1mHLEGEw}}
Genetics
- Hiatus hernia is possibly transmitted in autosomal dominant to male to male inheritance pattern.[12][13][14][15]
- Sliding hiatus hernia is usually sporadic but some cases have been seen following familial pattern, as do the paraoesophageal hiatus hernia.[16]
Associated Conditions
Conditions associated with hiatus hernia include:
- Gastroesophageal reflux disease[17]
- Esophagal ring[18]
- Congenital diaphragmatic hernia[12][19]
- Epiphrenic diverticula[20]
Gross Pathology

- On gross pathology, characteristic findings of hiatus hernia include:[18]
- Herniated portion gets dilated and undergo ischemic changes
- Ischemic necrosis can be seen
Microscopic Pathology
- On microscopic histopathological analysis, variable chronic inflammation, ischemia and necrosis may be seen in hiatus hernia.[18]
References
- ↑ - Own work, CC BY-SA 4.0, https://commons.wikimedia.org/w/index.php?curid=44924605
- ↑ Boeckxstaens GE (2005). "The lower oesophageal sphincter". Neurogastroenterol. Motil. 17 Suppl 1: 13–21. doi:10.1111/j.1365-2982.2005.00661.x. PMID 15836451.
- ↑ Sivacolundhu RK, Read RA, Marchevsky AM (2002). "Hiatal hernia controversies--a review of pathophysiology and treatment options". Aust. Vet. J. 80 (1–2): 48–53. PMID 12180879.
- ↑ 4.0 4.1 4.2 Kahrilas PJ, Lin S, Chen J, Manka M (1999). "The effect of hiatus hernia on gastro-oesophageal junction pressure". Gut. 44 (4): 476–82. PMC 1727465. PMID 10075953.
- ↑ Wolf BS (1973). "Sliding hiatal hernia: the need for redefinition". Am J Roentgenol Radium Ther Nucl Med. 117 (2): 231–47. PMID 4734411.
- ↑ Friedland GW (1978). "Progress in radiology: historical review of the changing concepts of lower esophageal anatomy: 430 B.C.--1977". AJR Am J Roentgenol. 131 (3): 373–8. doi:10.2214/ajr.131.3.373. PMID 98978.
- ↑ Menezes, Mariano A.; Herbella, Fernando A. M. (2017). "Pathophysiology of Gastroesophageal Reflux Disease". World Journal of Surgery. 41 (7): 1666–1671. doi:10.1007/s00268-017-3952-4. ISSN 0364-2313.
- ↑ https://my.clevelandclinic.org/health/diseases/8098-hiatal-hernia
- ↑ Christensen J, Miftakhov R (2000). "Hiatus hernia: a review of evidence for its origin in esophageal longitudinal muscle dysfunction". Am. J. Med. 108 Suppl 4a: 3S–7S. PMID 10718444.
- ↑ Patti MG, Goldberg HI, Arcerito M, Bortolasi L, Tong J, Way LW (1996). "Hiatal hernia size affects lower esophageal sphincter function, esophageal acid exposure, and the degree of mucosal injury". Am. J. Surg. 171 (1): 182–6. doi:10.1016/S0002-9610(99)80096-8. PMID 8554137.
- ↑ Kahrilas PJ, Kim HC, Pandolfino JE (2008). "Approaches to the diagnosis and grading of hiatal hernia". Best Pract Res Clin Gastroenterol. 22 (4): 601–16. doi:10.1016/j.bpg.2007.12.007. PMC 2548324. PMID 18656819.
- ↑ 12.0 12.1 Goodman, R. M.; Wooley, C. F.; Ruppert, R. D.; Freimanis, A. K. (1969). "A Possible Genetic Role in Esophageal Hiatus Hernia". Journal of Heredity. 60 (2): 71–74. doi:10.1093/oxfordjournals.jhered.a107936. ISSN 1465-7333.
- ↑ Carré IJ, Johnston BT, Thomas PS, Morrison PJ (1999). "Familial hiatal hernia in a large five generation family confirming true autosomal dominant inheritance". Gut. 45 (5): 649–52. PMC 1727703. PMID 10517898.
- ↑ Sillero C, Reyes A, Pérez-Mateo M, Vázquez N, Alonso P, Arenas M (1984). "[Hiatal hernia of familial nature]". Rev Clin Esp (in Spanish; Castilian). 172 (2): 79–81. PMID 6718778.
- ↑ Gryglewski A, Pena IZ, Tomaszewski KA, Walocha JA (2014). "Unsolved questions regarding the role of esophageal hiatus anatomy in the development of esophageal hiatal hernias". Adv Clin Exp Med. 23 (4): 639–44. PMID 25166451.
- ↑ Baglaj SM, Noblett HR (1999). "Paraoesophageal hernia in children: familial occurrence and review of the literature". Pediatr. Surg. Int. 15 (2): 85–7. doi:10.1007/s003830050522. PMID 10079336.
- ↑ Gatopoulou A, Mimidis K, Giatromanolaki A, Papadopoulos V, Polychronidis A, Lyratzopoulos N, Sivridis E, Minopoulos G (2005). "Impact of hiatal hernia on histological pattern of non-erosive reflux disease". BMC Gastroenterol. 5: 2. doi:10.1186/1471-230X-5-2. PMC 546187. PMID 15638947.
- ↑ 18.0 18.1 18.2 Haber, Meryl (2002). Differential diagnosis in surgical pathology. Philadelphia: Saunders. ISBN 9780721690537.
- ↑ Furtado R, Le Page P, Falk G (2013). "'Pantaloon' diaphragmatic hernia masquerading as a paraoesophageal hiatal hernia". ANZ J Surg. 83 (12): 994–5. doi:10.1111/ans.12252. PMID 24289054.
- ↑ Tedesco P, Fisichella PM, Way LW, Patti MG (2005). "Cause and treatment of epiphrenic diverticula". Am. J. Surg. 190 (6): 891–4. doi:10.1016/j.amjsurg.2005.08.016. PMID 16307941.
- ↑ CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=1784490