Hepatitis A overview
|
Hepatitis A |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Hepatitis A overview On the Web |
|
American Roentgen Ray Society Images of Hepatitis A overview |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
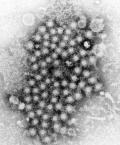
Hepatitis A (formerly known as infectious hepatitis and epidemical virus) is an acute infectious disease of the liver caused by the hepatitis A virus (Hep A),[1] an RNA virus, usually spread the fecal-oral route; transmitted person-to-person by ingestion of contaminated food or water or through direct contact with an infectious person. Tens of millions of individuals worldwide are estimated to become infected with Hep A each year.[2] The time between infection and the appearance of the symptoms (the incubation period) is between two and six weeks and the average incubation period is 28 days.[3]
In developing countries, and in regions with poor hygiene standards, the incidence of infection with this virus is high[4] and the illness is usually contracted in early childhood. As incomes rise and access to clean water increases, the incidence of HAV decreases.[5] Hepatitis A infection causes no clinical signs and symptoms in over 90% of infected children and since the infection confers lifelong immunity, the disease is of no special significance to those infected early in life. In Europe, the United States and other industrialized countries, on the other hand, the infection is contracted primarily by susceptible young adults, most of whom are infected with the virus during trips to countries with a high incidence of the disease[3] or through contact with infectious persons.
HAV infection produces a self-limited disease that does not result in chronic infection or chronic liver disease. However, 10–15% of patients might experience a relapse of symptoms during the 6 months after acute illness. Acute liver failure from Hepatitis A is rare (overall case-fatality rate: 0.5%). The risk for symptomatic infection is directly related to age, with >80% of adults having symptoms compatible with acute viral hepatitis and the majority of children having either asymptomatic or unrecognized infection.[6] Antibody produced in response to HAV infection persists for life and confers protection against reinfection. The disease can be prevented by vaccination, and hepatitis A vaccine has been proven effective in controlling outbreaks worldwide.[3]
Diagnosis
Laboratory Findings
Hepatitis A cannot be differentiated from other types of viral hepatitis on the basis of clinical or epidemiologic features alone. Serologic testing to detect immunoglobulin M (IgM) antibody to the capsid proteins of HAV (IgM anti-HAV) is required to confirm a diagnosis of acute HAV infection. In most persons, IgM anti-HAV becomes detectable 5-10 days before the onset of symptoms and can persist for up to 6 months after infection [7][8]. Immunoglobulin G (IgG) anti-HAV, which appears early in the course of infection, remains detectable for the person's lifetime and confers lifelong protection against the disease [9]. Commercial diagnostic tests are available for the detection of IgM and total (IgM and IgG) anti-HAV in serum.
HAV RNA can be detected in the blood and stool of most persons during the acute phase of infection by using nucleic acid amplification methods, and nucleic acid sequencing has been used to determine the relatedness of HAV isolates [10]. However, these methods, available in only a limited number of research laboratories, generally are not used for diagnostic purposes.
CT
CT scan is usually not indicated towards diagnosis of hepatitis A. However it may be done to exclude alternative diagnosis.
Ultrasound
Ultrasound of the abdomen may be carried out in patients with hepatitis A to evaluate for any other possible causes of hepatomegaly or chronic liver disease.
References
- ↑ Ryan KJ, Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill. pp. 541–4. ISBN 0838585299.
- ↑ Wasley A, Fiore A, Bell BP (2006). "Hepatitis A in the era of vaccination". Epidemiol Rev. 28: 101–11. doi:10.1093/epirev/mxj012. PMID 16775039.
- ↑ 3.0 3.1 3.2 Connor BA (2005). "Hepatitis A vaccine in the last-minute traveler". Am. J. Med. 118 (Suppl 10A): 58S–62S. doi:10.1016/j.amjmed.2005.07.018. PMID 16271543.
- ↑ Steffen R (2005). "Changing travel-related global epidemiology of hepatitis A". Am. J. Med. 118 (10): 46S–49S. doi:10.1016/j.amjmed.2005.07.016. PMID 16271541. Retrieved 2008-12-20. Unknown parameter
|month=ignored (help) - ↑ Jacobsen KH, Koopman JS (2005). "The effects of socioeconomic development on worldwide hepatitis A virus seroprevalence patterns". Int J Epidemiol. 34 (3): 600–9. doi:10.1093/ije/dyi062. PMID 15831565.
- ↑ Ciocca M. (2000). "Clinical course and consequences of hepatitis A infection". Vaccine. 18: 71–4. doi:10.1016/S0264-410X(99)00470-3. PMID 10683554.
- ↑ Bower WA, Nainan OV, Margolis HS. Duration of viremia in naturally-acquired hepatitis A viral infections. [Abstract 103] In: Abstracts of the Infectious Diseases Society of America 35th Annual Meeting. Alexandria, VA: Infectious Diseases Society of America, 1997.
- ↑ Liaw YF, Yang CY, Chu CM, Huang MJ (1986). "Appearance and persistence of hepatitis A IgM antibody in acute clinical hepatitis A observed in an outbreak". Infection. 14 (4): 156–8. PMID 3759243.
|access-date=requires|url=(help) - ↑ Stapleton JT (1995). "Host immune response to hepatitis A virus". The Journal of Infectious Diseases. 171 Suppl 1: S9–14. PMID 7876654. Retrieved 2012-02-28. Unknown parameter
|month=ignored (help) - ↑ Hutin YJ, Pool V, Cramer EH, Nainan OV, Weth J, Williams IT, Goldstein ST, Gensheimer KF, Bell BP, Shapiro CN, Alter MJ, Margolis HS (1999). "A multistate, foodborne outbreak of hepatitis A. National Hepatitis A Investigation Team". The New England Journal of Medicine. 340 (8): 595–602. doi:10.1056/NEJM199902253400802. PMID 10029643. Retrieved 2012-02-28. Unknown parameter
|month=ignored (help)
- Pages using duplicate arguments in template calls
- CS1 maint: Extra text: authors list
- CS1 maint: Multiple names: authors list
- Pages with citations using unsupported parameters
- Pages using citations with accessdate and no URL
- Foodborne illnesses
- Hepatitis
- Picornaviruses
- Viral diseases
- Mature chapter
- Infectious disease
- Disease