Hepatitis A overview: Difference between revisions
Rim Halaby (talk | contribs) |
Rim Halaby (talk | contribs) |
||
| Line 80: | Line 80: | ||
==Diagnosis== | ==Diagnosis== | ||
===History and Symptoms=== | |||
[[Hepatitis A virus]] ([[HAV]]) infection can be either [[asymptomatic]] or [[symptomatic]].<ref name="pmid4191502">{{cite journal |author=Krugman S, Giles JP |title=Viral hepatitis. New light on an old disease |journal=[[JAMA : the Journal of the American Medical Association]] |volume=212 |issue=6 |pages=1019–29 |year=1970 |month=May |pmid=4191502 |doi= |url= |accessdate=2012-02-28}}</ref> [[Symptoms]] of [[hepatitis A]] include [[fever]], [[fatigue]], [[loss of appetite]], [[nausea]], [[vomiting]], [[abdominal pain]], and [[jaundice]]. | |||
===Physical Examination=== | |||
Hepatitis A virus infection is commonly associated with [[fever]], [[jaundice]], icteric [[sclera]], [[abdominal tenderness]], and [[hepatomegaly]] on physical examination. Other pertinent findings include [[rash]], [[cervical]] [[lymphadenopathy]], [[abdominal distension]], [[ascites]], and [[altered mental status]]. | |||
===Laboratory Findings=== | ===Laboratory Findings=== | ||
Hepatitis A cannot be differentiated from other types of viral hepatitis on the basis of clinical or epidemiologic features alone. Serologic | [[Hepatitis A]] cannot be differentiated from other types of [[viral hepatitis]] on the basis of clinical or [[epidemiologic]] features alone. Laboratory tests are required for its [[diagnosis]]. Serologic tests in hepatitis A virus (HAV) infection reveal elevated [[IgM]] anti-[[HAV]] in the acute phase (gold standard) in addition to an elevated [[IgG]] anti-[[HAV]] that remains elevated for the person's lifetime. Additional laboratory findings include the detection and sequencing of [[HAV]] [[RNA]], an elevated direct [[bilirubin]], and elevated [[liver enzymes]]. [[Liver biopsy]] has a minimal role in the [[diagnosis]] of HAV infection and it is only used when the [[diagnosis]] is unclear or when relapse is suspected. | ||
===CT=== | |||
A [[CT scan]] is usually not indicated for the [[diagnosis]] of [[hepatitis A]]. However, it may be performed to exclude alternative diagnoses. | |||
===Ultrasound=== | ===Ultrasound=== | ||
An [[ultrasound]] of the [[abdomen]] may be performed in patients with [[hepatitis A]] to rule out other possible causes of [[hepatomegaly]] or [[chronic liver disease]]. Common ultrasound findings in acute [[hepatitis A]] include brightness of the [[portal vein]] walls and decreased [[echogenicity]] of the [[liver]]. | |||
==Treatment== | ==Treatment== | ||
Revision as of 02:18, 30 July 2014
|
Hepatitis A |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Hepatitis A overview On the Web |
|
American Roentgen Ray Society Images of Hepatitis A overview |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2]
Overview
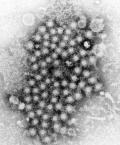
Hepatitis A (formerly known as infectious hepatitis and epidemical virus) is an acute infectious disease of the liver caused by the hepatitis A virus (Hep A),[1] an RNA virus, usually spread the fecal-oral route; transmitted person-to-person by ingestion of contaminated food or water or through direct contact with an infectious person. Tens of millions of individuals worldwide are estimated to become infected with Hep A each year.[2] The time between infection and the appearance of the symptoms (the incubation period) is between two and six weeks and the average incubation period is 28 days.[3]
In developing countries, and in regions with poor hygiene standards, the incidence of infection with this virus is high[4] and the illness is usually contracted in early childhood. As incomes rise and access to clean water increases, the incidence of HAV decreases.[5] Hepatitis A infection causes no clinical signs and symptoms in over 90% of infected children and since the infection confers lifelong immunity, the disease is of no special significance to those infected early in life. In Europe, the United States and other industrialized countries, on the other hand, the infection is contracted primarily by susceptible young adults, most of whom are infected with the virus during trips to countries with a high incidence of the disease[3] or through contact with infectious persons.
HAV infection produces a self-limited disease that does not result in chronic infection or chronic liver disease. However, 10–15% of patients might experience a relapse of symptoms during the 6 months after acute illness. Acute liver failure from Hepatitis A is rare (overall case-fatality rate: 0.5%). The risk for symptomatic infection is directly related to age, with >80% of adults having symptoms compatible with acute viral hepatitis and the majority of children having either asymptomatic or unrecognized infection.[6] Antibody produced in response to HAV infection persists for life and confers protection against reinfection. The disease can be prevented by vaccination, and hepatitis A vaccine has been proven effective in controlling outbreaks worldwide.[3]
Historical Perspective
Hepatitis A virus was first identified in 1973. It was classified as a separate disease from other types of hepatitis during World War II. However, its true prevalence and route of transmission would only be recognized later.[7] During 1995-1996, the Food and Drug Administration (FDA) approved the inactivated hepatitis A vaccines. Consequently, hepatitis A became a disease that was not only common but also vaccine-preventable.
Pathophysiology
Hepatitis A is a liver disease caused by the hepatitis A virus (HAV). HAV has fecal-oral transmission and its infectivity peaks about 2-weeks before the onset of jaundice. Gross observation of the liver may show an enlarged and erythematous liver, while microscopically it may reveal lymphocyte infiltration and inflammation of the portal tracts.
Causes
Hepatitis A is a liver disease caused by the hepatitis A virus (HAV). HAV has fecal-oral transmission and its infectivity peaks about 2-weeks before the onset of jaundice. Gross observation of the liver may show an enlarged and erythematous liver, while microscopically it may reveal lymphocyte infiltration and inflammation of the portal tracts.
Differential Diagnosis
Hepatitis A must be differentiated from other diseases that cause fever, nausea, vomiting, jaundice, hepatomegaly, icteric sclera, elevated ALT, AST, and PCR such as other viral hepatitis, alcoholic hepatitis, and autoimmune hepatitis.
Epidemiology and Demographics
The incidence of hepatitis A varies among eras, countries and even cities within the same country. In recent years it has been noted a shift in prevalence, what was once a disease more prevalent in children, is today predominant in adults. In the United States, the incidence of hepatitis A in 2011 was 0.4 cases per 100,000 population. In recent years, the rates of hepatitis A have been similar among all age groups. After the introduction of the HAV vaccine, historic differences in rates of hepatitis A among racial/ethnic populations have also narrowed. In developed countries, elimination of historic geographic differences in incidence rates has also occurred. In developing countries with very poor sanitary conditions and hygienic practices, most children (90%) are infected with the hepatitis A virus before the age of 10.
Risk Factors
Subjects who are not immunized against hepatitis A virus (HAV) and who travel to endemic areas where there is poor sanitation and lack of safe water are at increased risk of contracting HAV infection. Additional risk factors for HAV include intravenous drug injection, living in a household with an infected person, having a sexual partner with acute HAV infection, and attending childcare centers.
Screening
The detection of hepatitis A virus (HAV) antibodies in the blood is used to screen for hepatitis A. Anti-HAV IgG remains elevated after acute disease.[8]
Natural History, Complications and Prognosis
Hepatitis A is caused by infection with hepatitis A virus (HAV) which has an incubation period of approximately 28 days. HAV infection produces a self-limited disease, rarely leading to acute liver failure. The risk for symptomatic infection is related to the age of the patient. While children most commonly have either asymptomatic or unrecognized infection, more than 80% of adults exhibit symptoms of acute viral hepatitis, such as fatigue, malaise, nausea, vomiting, and anorexia.[9] Possible complications of hepatitis A include dehydration, electrolyte imbalance, bleeding, and rarely fulminant hepatitis. The prognosis depends on the age of the patient and the underlying liver condition. Approximately 10 to 15% of patients experience a relapse of symptoms during the 6 months following acute illness.
Diagnosis
History and Symptoms
Hepatitis A virus (HAV) infection can be either asymptomatic or symptomatic.[10] Symptoms of hepatitis A include fever, fatigue, loss of appetite, nausea, vomiting, abdominal pain, and jaundice.
Physical Examination
Hepatitis A virus infection is commonly associated with fever, jaundice, icteric sclera, abdominal tenderness, and hepatomegaly on physical examination. Other pertinent findings include rash, cervical lymphadenopathy, abdominal distension, ascites, and altered mental status.
Laboratory Findings
Hepatitis A cannot be differentiated from other types of viral hepatitis on the basis of clinical or epidemiologic features alone. Laboratory tests are required for its diagnosis. Serologic tests in hepatitis A virus (HAV) infection reveal elevated IgM anti-HAV in the acute phase (gold standard) in addition to an elevated IgG anti-HAV that remains elevated for the person's lifetime. Additional laboratory findings include the detection and sequencing of HAV RNA, an elevated direct bilirubin, and elevated liver enzymes. Liver biopsy has a minimal role in the diagnosis of HAV infection and it is only used when the diagnosis is unclear or when relapse is suspected.
CT
A CT scan is usually not indicated for the diagnosis of hepatitis A. However, it may be performed to exclude alternative diagnoses.
Ultrasound
An ultrasound of the abdomen may be performed in patients with hepatitis A to rule out other possible causes of hepatomegaly or chronic liver disease. Common ultrasound findings in acute hepatitis A include brightness of the portal vein walls and decreased echogenicity of the liver.
Treatment
Surgery
Patients who develop fulminant hepatitis may require aggressive supportive therapy, and be transferred to a center capable of performing liver transplantation.
References
- ↑ Ryan KJ, Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill. pp. 541–4. ISBN 0838585299.
- ↑ Wasley A, Fiore A, Bell BP (2006). "Hepatitis A in the era of vaccination". Epidemiol Rev. 28: 101–11. doi:10.1093/epirev/mxj012. PMID 16775039.
- ↑ 3.0 3.1 3.2 Connor BA (2005). "Hepatitis A vaccine in the last-minute traveler". Am. J. Med. 118 (Suppl 10A): 58S–62S. doi:10.1016/j.amjmed.2005.07.018. PMID 16271543.
- ↑ Steffen R (2005). "Changing travel-related global epidemiology of hepatitis A". Am. J. Med. 118 (10): 46S–49S. doi:10.1016/j.amjmed.2005.07.016. PMID 16271541. Retrieved 2008-12-20. Unknown parameter
|month=ignored (help) - ↑ Jacobsen KH, Koopman JS (2005). "The effects of socioeconomic development on worldwide hepatitis A virus seroprevalence patterns". Int J Epidemiol. 34 (3): 600–9. doi:10.1093/ije/dyi062. PMID 15831565.
- ↑ Ciocca M. (2000). "Clinical course and consequences of hepatitis A infection". Vaccine. 18: 71–4. doi:10.1016/S0264-410X(99)00470-3. PMID 10683554.
- ↑ Melnick JL (1995). "History and epidemiology of hepatitis A virus". J Infect Dis. 171 Suppl 1: S2–8. PMID [ 7876643 [ Check
|pmid=value (help). - ↑ "Hepatitis A Screening".
- ↑ Sexually Transmitted Diseases Treatment Guidelines, 2010. Centers for Disease Control and Prevention. Recommendations and Reports December 17, 2010 / 59(RR12);1-110 [1]
- ↑ Krugman S, Giles JP (1970). "Viral hepatitis. New light on an old disease". JAMA : the Journal of the American Medical Association. 212 (6): 1019–29. PMID 4191502. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help)
- Pages using duplicate arguments in template calls
- CS1 maint: Extra text: authors list
- CS1 maint: Multiple names: authors list
- Pages with citations using unsupported parameters
- CS1 errors: PMID
- Pages using citations with accessdate and no URL
- Foodborne illnesses
- Hepatitis
- Picornaviruses
- Viral diseases
- Mature chapter
- Infectious disease
- Disease