Hemorrhoids differential diagnosis: Difference between revisions
Jump to navigation
Jump to search
Ahmed Younes (talk | contribs) |
m (Bot: Removing from Primary care) |
||
| (14 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
[[Image:Home_logo1.png|right|250px|link=https://www.wikidoc.org/index.php/Hemorrhoids]] | |||
{{CMG}}; {{AE}}{{AY}} | {{CMG}}; {{AE}}{{AY}} | ||
==Overview== | ==Overview== | ||
Hemorrhoids should be differentiated from other diseases | Hemorrhoids should be differentiated from other diseases that cause anal discomfort and pain with defecation such as [[rectal cancer]], [[anal fissure]], [[anal abscess]], and [[anal fistula]]. | ||
==Differentiating Hemorrhoids from other Diseases== | ==Differentiating Hemorrhoids from other Diseases== | ||
Hemorrhoids should be differentiated from other diseases | Hemorrhoids should be differentiated from other diseases that cause anal discomfort and pain with defecation such as [[anal fissure]], [[rectal prolapse]] and [[perianal abscess]]. | ||
{| class="wikitable" | {| class="wikitable" | ||
| Line 16: | Line 16: | ||
!Sample image | !Sample image | ||
|- | |- | ||
|Anal fissure | |Hemorrhoids | ||
| | |||
'''External hemorrhoids''' | |||
* External hemorrhoids are painful as the skin below the punctate line is sensitive to pain.<sup>[[Hemorrhoids history and symptoms#cite note-pmid28567655-1|[1]]]</sup> | |||
* [[Blood clots]] may form in external hemorrhoids. | |||
* Thrombosed external hemorrhoids cause [[bleeding]], painful [[swelling]], or a hard lump around the [[anus]]. | |||
* When the [[blood clot]] dissolves, extra skin is left behind. This skin can become [[Irritation|irritated]] or [[itch]]. | |||
* Excessive straining, rubbing, or cleaning around the [[anus]] may make symptoms, such as [[itching]] and [[irritation]], worse. | |||
'''Internal hemorrhoids''' | |||
* The most common symptom of internal hemorrhoids is bright red blood on stool, on toilet paper, or in the toilet bowl after a bowel movement. | |||
* Internal hemorrhoids that are not prolapsed are usually not painful. | |||
* Prolapsed hemorrhoids often cause pain, discomfort, and anal [[Itch|itching]] | |||
| | |||
'''Skin examination''' | |||
* Inspection of the [[anal verge]] may show scratch marks and [[skin tags]]. | |||
* Inspection also may reveal external hemorrhoids or [[Prolapse|prolapsed]] internal hemorrhoids. | |||
'''Digital rectal examination''' | |||
* [[Digital rectal examination]] reveals the size and location of hemorrhoids. | |||
* [[Thrombosed]] hemorrhoids are tender to palpation. | |||
* Internal hemorrhoids are not palpable by [[digital rectal examination]] and the use of [[Anoscopy|anoscope]] is mandatory. | |||
|[[Image:Haemorrhoiden 1Grad endo 01 - By Dr. Joachim Guntau - www.Endoskopiebilder.de, CC BY-SA 3.0, httpscommons.wikimedia.orgwindex.phpcurid=18660115.jpg|center|300px|thumb| External hemorrhoids - By Dr. Joachim Guntau - www.Endoskopiebilder.de, CC BY-SA 3.0, httpscommons.wikimedia.orgwindex.phpcurid=18660115]] | |||
|- | |||
|[[Anal fissure]] | |||
| | | | ||
* [[Fissure|Anal fissure]] usually presents with tearing pain with every bowel movement.<ref name="pmid27041801">{{cite journal |vauthors=Schlichtemeier S, Engel A |title=Anal fissure |journal=Aust Prescr |volume=39 |issue=1 |pages=14–7 |year=2016 |pmid=27041801 |pmc=4816871 |doi=10.18773/austprescr.2016.007 |url=}}</ref> | * [[Fissure|Anal fissure]] usually presents with tearing pain with every bowel movement.<ref name="pmid27041801">{{cite journal |vauthors=Schlichtemeier S, Engel A |title=Anal fissure |journal=Aust Prescr |volume=39 |issue=1 |pages=14–7 |year=2016 |pmid=27041801 |pmc=4816871 |doi=10.18773/austprescr.2016.007 |url=}}</ref> | ||
* Pain usually lasts for minutes to hours after every bowel | * Pain usually lasts for minutes to hours after every bowel movement. | ||
* Patient is typically afraid of going to the bathroom to avoid the pain, which leads to a viscious cycle. The [[Anal fissure|fissure]] worsens the [[constipation]] and the [[constipation]] (hard stool) aggravates the [[Anal fissure|fissure]]. | * Patient is typically afraid of going to the bathroom to avoid the pain, which leads to a viscious cycle. The [[Anal fissure|fissure]] worsens the [[constipation]] and the [[constipation]] (hard stool) aggravates the [[Anal fissure|fissure]]. | ||
* About two thirds of the patients present with bright red blood streaks on toilet papers or on the surface of stools. | * About two-thirds of the patients present with bright red blood streaks on toilet papers or on the surface of stools. | ||
* May be accompanied by [[pruritis]] and [[discharge]]. | * May be accompanied by [[pruritis]] and [[discharge]]. | ||
| | | | ||
* Most [[Anal fissure|fissures]] occur in the posterior midline of the [[Anus|anal canal]].<ref name="pmid26929749">{{cite journal |vauthors=Beaty JS, Shashidharan M |title=Anal Fissure |journal=Clin Colon Rectal Surg |volume=29 |issue=1 |pages=30–7 |year=2016 |pmid=26929749 |pmc=4755763 |doi=10.1055/s-0035-1570390 |url=}}</ref> | * Most [[Anal fissure|fissures]] occur in the posterior midline of the [[Anus|anal canal]].<ref name="pmid26929749">{{cite journal |vauthors=Beaty JS, Shashidharan M |title=Anal Fissure |journal=Clin Colon Rectal Surg |volume=29 |issue=1 |pages=30–7 |year=2016 |pmid=26929749 |pmc=4755763 |doi=10.1055/s-0035-1570390 |url=}}</ref> | ||
* [[Skin tags]] in the perianal area may accompany chronic anal fissures. | * [[Skin tags]] in the perianal area may accompany [[chronic]] [[anal fissures]]. | ||
|[[Image:Anal fissure 1 - By Bernardo Gui - Own work, Public Domain, httpscommons.wikimedia.orgwindex.phpcurid=8885750.jpg|center|300px|thumb|Anal fissure - Own work, Public Domain, httpscommons.wikimedia.orgwindex.phpcurid=8885750]] | |[[Image:Anal fissure 1 - By Bernardo Gui - Own work, Public Domain, httpscommons.wikimedia.orgwindex.phpcurid=8885750.jpg|center|300px|thumb|Anal fissure - Own work, Public Domain, httpscommons.wikimedia.orgwindex.phpcurid=8885750]] | ||
|- | |- | ||
| Line 31: | Line 55: | ||
| | | | ||
* [[Rectal prolapse]] most commonly occurs in multiparous females over 40 years old.<ref name="pmid28144208">{{cite journal |vauthors=Cannon JA |title=Evaluation, Diagnosis, and Medical Management of Rectal Prolapse |journal=Clin Colon Rectal Surg |volume=30 |issue=1 |pages=16–21 |year=2017 |pmid=28144208 |doi=10.1055/s-0036-1593431 |url=}}</ref> | * [[Rectal prolapse]] most commonly occurs in multiparous females over 40 years old.<ref name="pmid28144208">{{cite journal |vauthors=Cannon JA |title=Evaluation, Diagnosis, and Medical Management of Rectal Prolapse |journal=Clin Colon Rectal Surg |volume=30 |issue=1 |pages=16–21 |year=2017 |pmid=28144208 |doi=10.1055/s-0036-1593431 |url=}}</ref> | ||
* | * Appears as a progressive mass protrusion from the [[anus]]. The protrusion first appears with straining and defecation, then progresses to the degree when it is no longer replaced back. | ||
* It presents with [[abdominal discomfort]] and incomplete defecation. | * It presents with [[abdominal discomfort]] and incomplete defecation. | ||
* [[Fecal incontinence]] and anal discharge. | * [[Fecal incontinence]] and anal discharge. | ||
* Pain is not usually present. | * Pain is not usually present. | ||
| | | | ||
* Mass protruding from the anus.<ref name="pmid28144206">{{cite journal |vauthors=Blaker K, Anandam JL |title=Functional Disorders: Rectoanal Intussusception |journal=Clin Colon Rectal Surg |volume=30 |issue=1 |pages=5–11 |year=2017 |pmid=28144206 |doi=10.1055/s-0036-1593433 |url=}}</ref> | * Mass protruding from the [[anus]].<ref name="pmid28144206">{{cite journal |vauthors=Blaker K, Anandam JL |title=Functional Disorders: Rectoanal Intussusception |journal=Clin Colon Rectal Surg |volume=30 |issue=1 |pages=5–11 |year=2017 |pmid=28144206 |doi=10.1055/s-0036-1593433 |url=}}</ref> | ||
* Concentric mucosal rings are characteristic | * Concentric mucosal rings are characteristic of [[rectal prolapse]]. | ||
|[[Image:Prolapse of rectum 01- By Dr. K.-H. Günther, Klinikum Main Spessart, Lohr am Main - Dr. K.-H. Günther, Klinikum Main Spessart, Lohr am Main, CC BY 3.0, httpscommons.wikimedia.orgwindex.phpcurid=20649968.jpg|center|300px|thumb|Rectal prolapse - By Dr. K.-H. Günther, Klinikum Main Spessart, Lohr am Main - Dr. K.-H. Günther, Klinikum Main Spessart, Lohr am Main, CC BY 3.0, httpscommons.wikimedia.orgwindex.phpcurid=20649968]] | |[[Image:Prolapse of rectum 01- By Dr. K.-H. Günther, Klinikum Main Spessart, Lohr am Main - Dr. K.-H. Günther, Klinikum Main Spessart, Lohr am Main, CC BY 3.0, httpscommons.wikimedia.orgwindex.phpcurid=20649968.jpg|center|300px|thumb|Rectal prolapse - By Dr. K.-H. Günther, Klinikum Main Spessart, Lohr am Main - Dr. K.-H. Günther, Klinikum Main Spessart, Lohr am Main, CC BY 3.0, httpscommons.wikimedia.orgwindex.phpcurid=20649968]] | ||
|- | |- | ||
|Perianal [[abscess]] | |[[Perianal abscess]] | ||
| | |||
* [[Perianal abscess]] presents with severe, continuous, dull, aching pain in the perianal area.<ref name="pmid28223268">{{cite journal |vauthors=Sahnan K, Adegbola SO, Tozer PJ, Watfah J, Phillips RK |title=Perianal abscess |journal=BMJ |volume=356 |issue= |pages=j475 |year=2017 |pmid=28223268 |doi= |url=}}</ref> | |||
* Pain is exacerbated with bowel movements, but is not exclusive to it. | |||
* [[Constipation]] due to fear of bowel movements. | |||
* [[Fever]], [[headache]], and [[chills]] may accompany the pain. | |||
* If the [[abscess]] starts to drain, discharge of purulent or bloody fluid may be noticed. | |||
| | | | ||
* | * Flatulent, [[erythematous]], and tender area of skin overlying the [[abscess]]. | ||
* If [[abscess]] is deep, tenderness is elicited with digital rectal examination. | |||
* If abscess | |||
| | | | ||
|- | |- | ||
|[[ | |[[Anal cancer]] | ||
| | | | ||
* Rectal bleeding is the most common presentation.<ref name="pmid28610905">{{cite journal |vauthors=Moureau-Zabotto L, Vendrely V, Abramowitz L, Borg C, Francois E, Goere D, Huguet F, Peiffert D, Siproudhis L, Ducreux M, Bouché O |title=Anal cancer: French Intergroup Clinical Practice Guidelines for diagnosis, treatment and follow-up |journal=Dig Liver Dis |volume= |issue= |pages= |year=2017 |pmid=28610905 |doi=10.1016/j.dld.2017.05.011 |url=}}</ref> | * Rectal bleeding is the most common presentation.<ref name="pmid28610905">{{cite journal |vauthors=Moureau-Zabotto L, Vendrely V, Abramowitz L, Borg C, Francois E, Goere D, Huguet F, Peiffert D, Siproudhis L, Ducreux M, Bouché O |title=Anal cancer: French Intergroup Clinical Practice Guidelines for diagnosis, treatment and follow-up |journal=Dig Liver Dis |volume= |issue= |pages= |year=2017 |pmid=28610905 |doi=10.1016/j.dld.2017.05.011 |url=}}</ref> | ||
* Mass sensation in the anus. | * Mass sensation in the [[anus]]. | ||
* Mucoid discharge may occur. | * Mucoid discharge may occur. | ||
* Patient may give a history of anal condyloma (especially homosexual men).<ref name="pmid28528690">{{cite journal |vauthors=Prigge ES, von Knebel Doeberitz M, Reuschenbach M |title=Clinical relevance and implications of HPV-induced neoplasia in different anatomical locations |journal=Mutat. Res. |volume=772 |issue= |pages=51–66 |year=2017 |pmid=28528690 |doi=10.1016/j.mrrev.2016.06.005 |url=}}</ref> | * Patient may give a history of anal [[condyloma]] (especially homosexual men).<ref name="pmid28528690">{{cite journal |vauthors=Prigge ES, von Knebel Doeberitz M, Reuschenbach M |title=Clinical relevance and implications of HPV-induced neoplasia in different anatomical locations |journal=Mutat. Res. |volume=772 |issue= |pages=51–66 |year=2017 |pmid=28528690 |doi=10.1016/j.mrrev.2016.06.005 |url=}}</ref> | ||
* Fecal incontinence. | * Fecal incontinence. | ||
| | | | ||
* On digital rectal examination, solid hemorrhagic mass that is firmly fixed to the surrounding structures is noted. | * On digital rectal examination, solid hemorrhagic mass that is firmly fixed to the surrounding structures is noted. | ||
* Femoral and inguinal lymph nodes may show lymphadenopathy secondary to spread of cancer. | * Femoral and inguinal [[lymph nodes]] may show [[lymphadenopathy]] secondary to spread of cancer. | ||
|[[Image:Anal CA - By Internet Archive Book Images - httpswww.flickr.comphotosinternetarchivebookimages14598073128Source book page httpsarchive.orgstreamdiseasesofrectum00gantdiseasesofrectum00gant-pagen653mode1up, No restrictions, httpsc.jpg|center|300px|thumb|Anal Cancer - By Internet Archive Book Images - httpswww.flickr.comphotosinternetarchivebookimages14598073128Source book page httpsarchive.orgstreamdiseasesofrectum00gantdiseasesofrectum00gant-pagen653mode1up, No restrictions, httpsc]] | |[[Image:Anal CA - By Internet Archive Book Images - httpswww.flickr.comphotosinternetarchivebookimages14598073128Source book page httpsarchive.orgstreamdiseasesofrectum00gantdiseasesofrectum00gant-pagen653mode1up, No restrictions, httpsc.jpg|center|300px|thumb|Anal Cancer - By Internet Archive Book Images - httpswww.flickr.comphotosinternetarchivebookimages14598073128Source book page httpsarchive.orgstreamdiseasesofrectum00gantdiseasesofrectum00gant-pagen653mode1up, No restrictions, httpsc]] | ||
|- | |- | ||
|[[Condylomata acuminata]] | |[[Condylomata acuminata]] | ||
| | | | ||
* Patient may give a history of anal | * Patient may give a history of unprotected anal sex with an infected partner. | ||
* | * Having multiple sexual partners is a risk factor and should be investigated.<ref name="pmid28160045">{{cite journal |vauthors=Wieland U, Kreuter A |title=[Genital warts in HIV-infected individuals] |language=German |journal=Hautarzt |volume=68 |issue=3 |pages=192–198 |year=2017 |pmid=28160045 |doi=10.1007/s00105-017-3938-z |url=}}</ref> | ||
* Condyloma | * [[Condyloma acuminata]] presents with painless warts that vary in size, shape, and color. | ||
* Pruritis and discharge | * [[ Pruritis]] and discharge may accompany the warts. | ||
| | |||
* Anal [[condyloma acuminata]] may be accompanied by cervical, vaginal, or even ororpharyngeal warts, so the patient should be examined thoroughly.<ref name="pmid27364818">{{cite journal |vauthors=Köhn FM, Schultheiss D, Krämer-Schultheiss K |title=[Dermatological diseases of the external male genitalia : Part 2: Infectious and malignant dermatological] |language=German |journal=Urologe A |volume=55 |issue=7 |pages=981–96 |year=2016 |pmid=27364818 |doi=10.1007/s00120-016-0163-9 |url=}}</ref> | |||
| | | | ||
|} | |} | ||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
{{WH}} | |||
{{WS}} | |||
[[Category:Gastroenterology]] | [[Category:Gastroenterology]] | ||
[[Category:Surgery]] | [[Category:Surgery]] | ||
[[Category:Needs overview]] | [[Category:Needs overview]] | ||
Latest revision as of 22:03, 29 July 2020

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ahmed Younes M.B.B.CH [2]
Overview
Hemorrhoids should be differentiated from other diseases that cause anal discomfort and pain with defecation such as rectal cancer, anal fissure, anal abscess, and anal fistula.
Differentiating Hemorrhoids from other Diseases
Hemorrhoids should be differentiated from other diseases that cause anal discomfort and pain with defecation such as anal fissure, rectal prolapse and perianal abscess.
| Disease | History | Physical exam findings | Sample image |
|---|---|---|---|
| Hemorrhoids |
External hemorrhoids
Internal hemorrhoids
|
Skin examination
Digital rectal examination
|
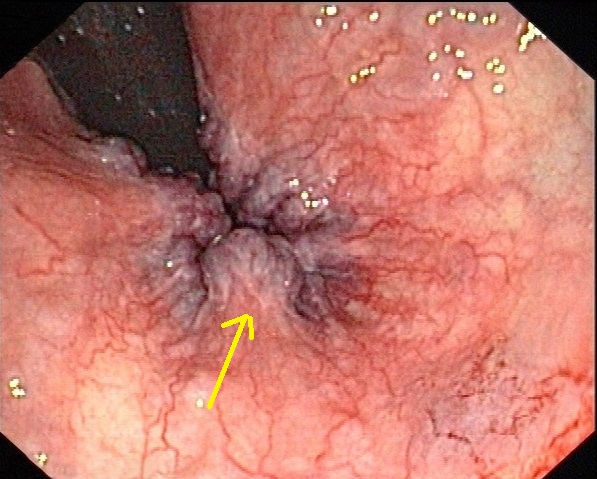 |
| Anal fissure |
|
|
 |
| Rectal prolapse |
|
|
 |
| Perianal abscess |
|
|
|
| Anal cancer |
|
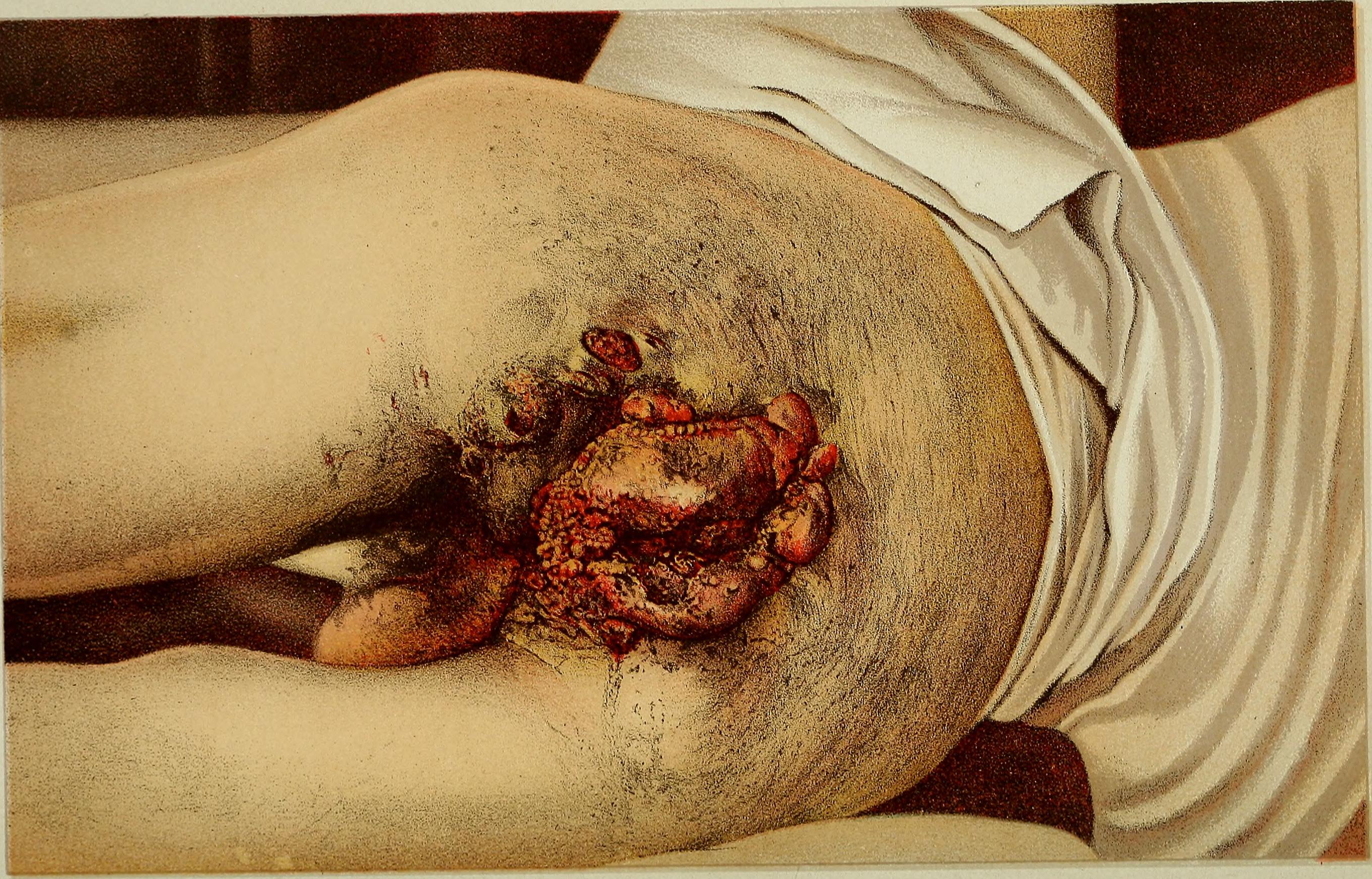 | |
| Condylomata acuminata |
|
|
References
- ↑ Schlichtemeier S, Engel A (2016). "Anal fissure". Aust Prescr. 39 (1): 14–7. doi:10.18773/austprescr.2016.007. PMC 4816871. PMID 27041801.
- ↑ Beaty JS, Shashidharan M (2016). "Anal Fissure". Clin Colon Rectal Surg. 29 (1): 30–7. doi:10.1055/s-0035-1570390. PMC 4755763. PMID 26929749.
- ↑ Cannon JA (2017). "Evaluation, Diagnosis, and Medical Management of Rectal Prolapse". Clin Colon Rectal Surg. 30 (1): 16–21. doi:10.1055/s-0036-1593431. PMID 28144208.
- ↑ Blaker K, Anandam JL (2017). "Functional Disorders: Rectoanal Intussusception". Clin Colon Rectal Surg. 30 (1): 5–11. doi:10.1055/s-0036-1593433. PMID 28144206.
- ↑ Sahnan K, Adegbola SO, Tozer PJ, Watfah J, Phillips RK (2017). "Perianal abscess". BMJ. 356: j475. PMID 28223268.
- ↑ Moureau-Zabotto L, Vendrely V, Abramowitz L, Borg C, Francois E, Goere D, Huguet F, Peiffert D, Siproudhis L, Ducreux M, Bouché O (2017). "Anal cancer: French Intergroup Clinical Practice Guidelines for diagnosis, treatment and follow-up". Dig Liver Dis. doi:10.1016/j.dld.2017.05.011. PMID 28610905.
- ↑ Prigge ES, von Knebel Doeberitz M, Reuschenbach M (2017). "Clinical relevance and implications of HPV-induced neoplasia in different anatomical locations". Mutat. Res. 772: 51–66. doi:10.1016/j.mrrev.2016.06.005. PMID 28528690.
- ↑ Wieland U, Kreuter A (2017). "[Genital warts in HIV-infected individuals]". Hautarzt (in German). 68 (3): 192–198. doi:10.1007/s00105-017-3938-z. PMID 28160045.
- ↑ Köhn FM, Schultheiss D, Krämer-Schultheiss K (2016). "[Dermatological diseases of the external male genitalia : Part 2: Infectious and malignant dermatological]". Urologe A (in German). 55 (7): 981–96. doi:10.1007/s00120-016-0163-9. PMID 27364818.