Hematopoiesis
|
Hematopoiesis Microchapters |
|
Hematopoiesis On the Web |
|---|
|
American Roentgen Ray Society Images of Hematopoiesis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Haematopoiesis (from Ancient Greek: haima blood; poiesis to make) (or hematopoiesis in the United States; sometimes also haemopoiesis or hemopoiesis) is the formation of blood cellular components. All of the cellular components of the blood are derived from haematopoietic stem cells. The term multipotent refers to the ability of a cell to become several different types of cell (but not all types in a germ layer). Multipotent haematopoietic cells can become any type of cell in the blood system. The multipotent cells determine what type of cell to become, or differentiate, in a step-wise fashion. It normally goes at a speed of 1011–1012 cells per day [1]

Lineages
All blood cells are divided into three lineages.
- Erythroid cells are the oxygen carrying red blood cells.
- Lymphoid cells are the cornerstone of the adaptive immune system. They are derived from common lymphoid progenitors. The lymphoid lineage is primarily composed of T-cells and B-cells. (white blood cells)
- Myeloid cells, which includes granulocytes, megakaryocytes, and macrophages, are derived from common myeloid progenitors, and are involved in such diverse roles as innate immunity, adaptive immunity, and blood clotting.
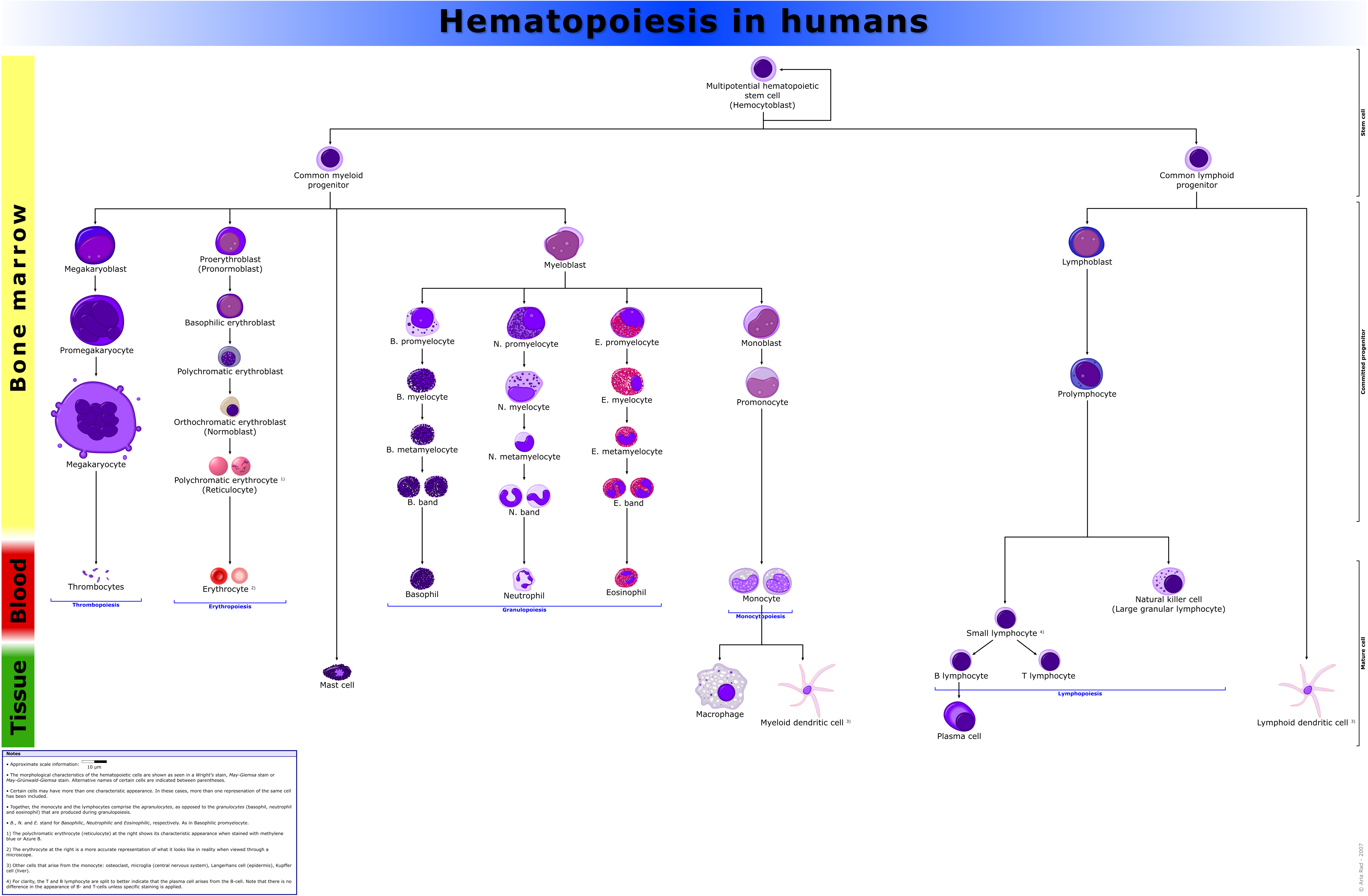
Granulopoiesis
Granulopoiesis (or granulocytopoiesis) is hematopoiesis of granulocytes.
It occurs primarily within bone marrow.
It involves the following stages:
- Pluripotential hemopoietic stem cell
- Myeloblast
- Promyelocyte
- Eosino/neutro/basophilic myelocyte
- Metamyelocyte
- Band cell
- Granulocytes (Eosino/neutro/basophil)
Locations
In developing embryos, blood formation occurs in aggregates of blood cells in the yolk sac, called blood islands. As development progresses, blood formation occurs in the spleen, liver and lymph nodes. When bone marrow develops, it eventually assumes the task of forming most of the blood cells for the entire organism. However, maturation, activation, and some proliferation of lymphoid cells occurs in secondary lymphoid organs (spleen, thymus, and lymph nodes). While most haematopoiesis in adults occurs in the marrow of the long bones such as the femurs, it also occurs in spongy bone like ribs and sternum).
Extramedullary
In some cases, the liver, thymus, and spleen may resume their haematopoietic function, if necessary. This is called extramedullary haematopoiesis. It may cause these organs to increase in size substantially. [1]
Other vertebrates
In some vertebrates, haematopoiesis can occur wherever there is a loose stroma of connective tissue and slow blood supply, such as the gut, spleen, kidney or ovaries.
Maturation
As a stem cell matures it undergoes changes in gene expression (the extent by which a gene exerts influence on its target changes) that limit the cell types that it can become and move it closer to a specific cell type. These changes can often be tracked by monitoring the presence of proteins on the surface of the cell. Each successive change moves the cell closer to its final choice of cell type and further limits its potential cell type until it is fully differentiated. This process is usually presented as a dendrogram or decision tree, which starts with a stem cell at the single starting point, and branches for the major lineages that branch into intermediate semi-differentiated cell types, and eventually, to fully differentiated cells.
Determination
It seems like it's the location of blood cells that makes the cell determination and not vice versa (i.e. e.g. that a hematopoietic stem cell determined to differentiate into a specific cell type would end up at a destined location). For instance, the thymus provides an environment for thymocytes to differentiate into a variety of different functional T cells.
For the stem cells and other undifferentiated blood cells in the bone marrow, the determination is generally explained by the determinism theory of hematopoiesis, saying that colony stimulating factors and other factors of the hematopoietic microenvironment determine the cells to follow a certain path of cell differentiation. This is the classical way of describing hematopoiesis. In fact, however, it is not really true. The ability of the bone marrow to regulate the quantity of different cell types to be produced is more accurately explained by a stochastic theory: Undifferentiated blood cells are determined to specific cell types by randomness. The hematopoietic microenvironment avails some of the cells to survive and some, on the other hand, to perform apoptosis. By regulating this balance between different cell types, the bone marrow can alter the quantity of different cells to ultimately be produced.
Haematopoietic growth factors
Red and white blood cell production is regulated with great precision in healthy humans, and the production of granulocytes is rapidly increased during infection. The proliferation and self-renewal of these cells depend on stem cell factor (SCF). Glycoprotein growth factors regulate the proliferation and maturation of the cells that enter the blood from the marrow, and cause cells in one or more committed cell lines to proliferate and mature. Three more factors which stimulate the production of committed stem cells are called colony-stimulating factors (CSFs) and include granulocyte-macrophage CSF (GM-CSF), granulocyte CSF (G-CSF) and macrophage CSF (M-CSF). These stimulate a lot of granulocyte formation. They are active on either progenitor cells or end product cells.
Erythropoietin is required for a myeloid progenitor cell to become an erythrocyte. [2] On the other hand, thrombopoietin makes myeloid progenitor cells differentiate to megakaryocytes (thrombocyte-forming cells).[2]
Examples of cytokines and the blood cells they give rise to, is shown in the picture below.

Transcription factors
Growth factors initiate signal transduction pathways, altering transcription factors, that, in turn activate genes that determines the differentiation of blood cells.
The early committed progenitors express low levels of transcription factors that may commit them to discrete cell lineages. Which cell lineage is selected for differentiation may depend both on chance and on the external signals received by progenitor cells. Several transcription factors have been isolated that regulate differentiation along the major cell lineages. For instance, PU.1 commits cells to the myeloid lineage whereas GATA-1 has an essential role in erythropoietic and megakaryocytic differentiation.
Extramedullary hematopoiesis in a thalassemia patient
Related Chapters
- Granulopoiesis, the hematopoiesis of granulocytes.
References
cs:Krvetvorba de:Hämatopoese nl:Hematopoëse sv:Hematopoes



