HIV AIDS pathophysiology
|
AIDS Microchapters |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
HIV AIDS pathophysiology On the Web |
|
American Roentgen Ray Society Images of HIV AIDS pathophysiology |
|
Risk calculators and risk factors for HIV AIDS pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Human Immunodeficiency virus causes AIDS by depleting CD4+ T helper lymphocytes. T lymphocytes are essential to the immune response and without them, the body cannot fight infections or kill cancerous cells. Thus the weakened immune system allows opportunistic infections and neoplastic processes. The mechanism of CD4+ T cell depletion differs in the acute and chronic phases, to sum it all AIDS has a complex pathophysiology.[1] To read about the progression of HIV infection to AIDS, click here
Pathophysiology
- The pathophysiologic progression from acute HIV infection to AIDS is described in the chapter HIV infection pathophysiology. This chapter explains the pathophysiology of AIDS.
- The specific decline in CD44 helper T cells, result in inversion of the normal CD4/CD8 T cell ratio. It also cause dysregulation of B cell antibody production.[2][3]
- The immune response to antigens begins to decline, as a result, the host fails to respond adequately to opportunistic infections and normally harmless commensals.
- The infections tend to be non-bacterial (i.e fungal, Viral) because the defect preferentially involves cellular immunity.
Role of GALT in pathogenesis
- Port of entry for HIV infection, is mostly through direct blood inoculation or exposure through genital mucosal surface. The gastrointestinal tract contains a large amount of lymphoid tissue, making it an ideal place for replication of Human Immunodeficiency Virus. GALT plays a role in HIV replication. [4]
- GALT has been found to have the following characteristics:
- Site of early viral seeding.
- Establishment of the pro-viral reservoir.
- The proviral GALT reservoir contributes to the following:
- Difficulty in controlling the infection.
- Difficulty in reducing the level of HIV provirus through sustained ART.[5] Various studies measuring the CD44 in GALT, have shown the relatively less reconstitution with ART, than that observed in peripheral blood.
Coinfections
Effect of geographic area on Opportunistic infection
The opportunistic infection in AIDS patient reflect the pathogen that are common in that area.
- In USA: Person with AIDS tends to present with commensal organism such as Pneumoncystis and Candida.
- In a study done by National Center of HIV/AIDS,[6] PCP was the most common AIDS-defining opportunistic infection to occur first.
- PCP was the first OI to occur for 36% of HIV-infected persons.
- The most common incident AIDS-defining OI (274 cases per 1000 person-years).
- The most common AIDS-defining OI to have occurred during the course of AIDS (53% of persons who died with AIDS had PCP diagnosed at some time during their course of AIDS).
- In a study done by National Center of HIV/AIDS,[6] PCP was the most common AIDS-defining opportunistic infection to occur first.
- In developing nations: Tuberculosis is more prevalent in those countries.
A. The major pulmonary illnesses
-
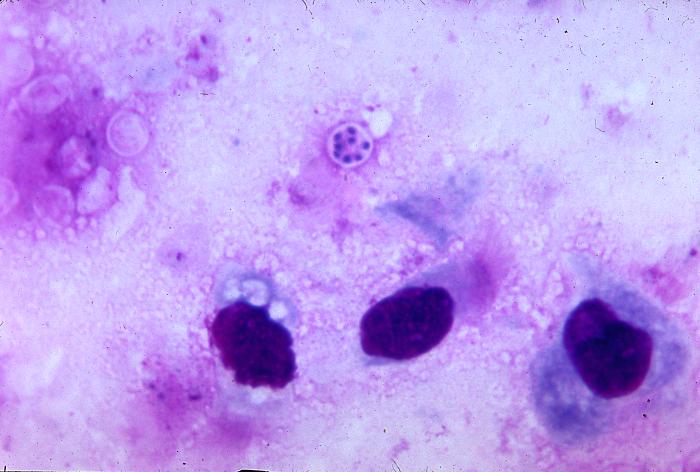
Pneumocystis jiroveci is present in this lung impression smear, using Giemsa stain
-
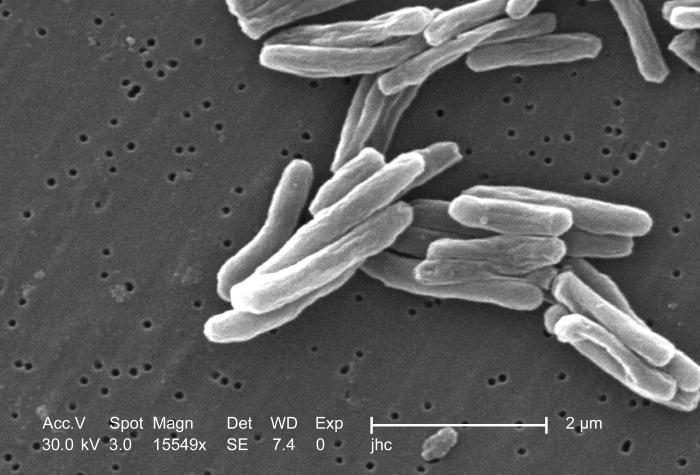
Scanning electron micrograph (SEM) of a number of Gram-positive Mycobacterium tuberculosis bacteria
Pneumocystis jiroveci pneumonia
Pneumocystis jiroveci pneumonia (originally known as Pneumocystis carinii pneumonia, often abbreviated PCP) is relatively rare in normal, immunocompetent people but common among HIV-infected individuals. Before the advent of effective treatment and diagnosis in Western countries it was a common immediate cause of death. In developing countries, it is still one of the first indications of AIDS in untested individuals, although it does not generally occur unless the CD4 count is less than 200 per µl (Feldman, 2005).
Tuberculosis
Among infections associated with HIV, Tuberculosis (TB) is unique in that it may be transmitted to immunocompetent persons via the respiratory route, is easily treatable once identified, may occur in early-stage HIV disease, and is preventable with drug therapy. However, multi-drug resistance is a potentially serious problem. Even though its incidence has declined because of the use of directly observed therapy and other improved practices in Western countries, this is not the case in developing countries where HIV is most prevalent. In early-stage HIV infection (CD4 count >300 cells per µl), TB typically presents as a pulmonary disease. In advanced HIV infection, TB may present atypically and extrapulmonary TB is common infecting bone marrow, bone, urinary and gastrointestinal tracts, liver, regional lymph nodes, and the central nervous system (Decker and Lazarus, 2000).
B. The major gastro-intestinal illnesses
Esophagitis
Esophagitis is an inflammation of the lining of the lower end of the esophagus (gullet or swallowing tube leading to the stomach). In HIV infected individuals, this could be due to fungus (candidiasis), virus (herpes simplex-1 or cytomegalovirus). In rare cases, it could be due to mycobacteria (Zaidi and Cervia, 2002).
Unexplained chronic diarrhea
In HIV infection, there are many possible causes of diarrhea, including common bacterial (Salmonella, Shigella, Listeria, Campylobacter, or Escherichia coli) and parasitic infections, and uncommon opportunistic infections such as cryptosporidiosis, microsporidiosis, Mycobacterium avium complex (MAC) and cytomegalovirus (CMV) colitis. Diarrhea may follow a course of antibiotics (common for Clostridium difficile). It may also be a side effect of several drugs used to treat HIV, or it may simply accompany HIV infection, particularly during primary HIV infection. In the later stages of HIV infection, diarrhea is thought to be a reflection of changes in the way the intestinal tract absorbs nutrients, and may be an important component of HIV-related wasting (Guerrant et al., 1990).
C. The major neurological illnesses
Toxoplasmosis
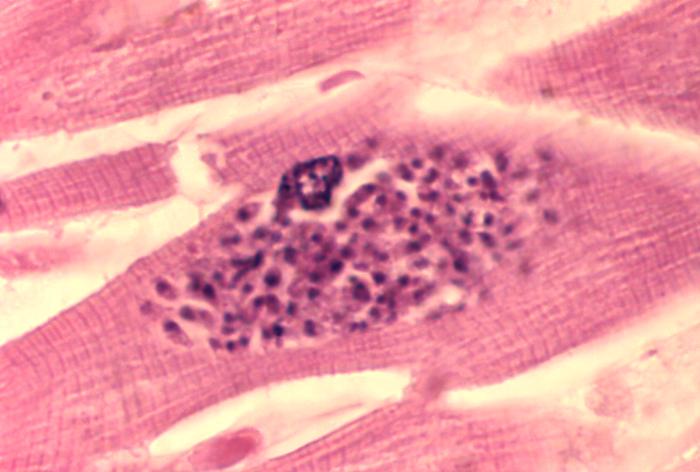
Toxoplasmosis is a disease caused by the single-celled parasite called Toxoplasma gondii. T. gondii usually infects the brain causing toxoplasma encephalitis. It can also infect and cause disease in the eyes and lungs (Luft and Chua, 2000).
Progressive multifocal leukoencephalopathy
Progressive multifocal leukoencephalopathy (PML) is a demyelinating disease, in which the myelin sheath covering the axons of nerve cells is gradually destroyed, impairing the transmission of nerve impulses. It is caused by a virus called JC virus which occurs in 70% of the population in latent form, causing disease only when the immune system has been severly weakened, as is the case for AIDS patients. It progresses rapidly, usually causing death within months of diagnosis (Sadler and Nelson, 1997).
HIV-associated dementia
HIV-1 associated dementia (HAD) is a metabolic encephalopathy induced by HIV infection and fueled by immune activation of brain macrophages and microglia (Gray et al., 2001). These cells are actively infected with HIV and secrete neurotoxins of both host and viral origin. Specific neurologic impairments are manifested by cognitive, behavioral, and motor abnormalities that occur after years of HIV infection and is associated with low CD4+ T cell levels and high plasma viral loads. Prevalence is between 15-30% in Western countries (Heaton et al., 1995; White et al., 1995) and has only been seen in 1-2% of India based infections (Satischandra et al., 2000; Wadia et al., 2001).
D. HIV-associated malignancies
Patients with HIV infection are susceptible to a number of malignancies (Yarchoan et al., 2005). The most common is Kaposi's sarcoma, and the appearance of this tumor in young gay men in New York in 1981 was one of the first signals of the AIDS epidemic. In addition, patients with HIV infection have a higher incidence of certain high grade B cell lymphomas, especially Burkitt-like and large cell lymphomas. These tumors, as well as aggressive cervical cancer in women, confer a diagnosis of AIDS in patients with HIV infection.
E. The major dermatological illnesses
AIDS-associated Kaposi sarcoma or KS-AIDS presents with cutaneous lesions that begin as one or several red to purple-red macules, rapidly progressing to papules, nodules, and plaques, with a predilection for the head, neck, trunk, and mucous membranes.
-
Kaposi's sarcoma lesion commonly found in patients with stage IV AIDS
-
Intraoral Kaposi’s sarcoma lesion with an overlying candidiasis infection
Related Chapters
References
- ↑ Guss DA (1994). "The acquired immune deficiency syndrome: an overview for the emergency physician, Part 1". J Emerg Med. 12 (3): 375–84. PMID 8040596.
|access-date=requires|url=(help) - ↑ Frazer IH, Mackay IR, Crapper RM, Jones B, Gust ID, Sarngadharan MG, Campbell DC, Ungar B (1986). "Immunological abnormalities in asymptomatic homosexual men: correlation with antibody to HTLV-III and sequential changes over two years". Q. J. Med. 61 (234): 921–33. PMID 3498182. Retrieved 2012-05-24. Unknown parameter
|month=ignored (help) - ↑ Schechter MT, Boyko WJ, Craib KJ, McLeod A, Willoughby B, Douglas B, Constance P, O'Shaughnessey M (1987). "Effects of long-term seropositivity to human immunodeficiency virus in a cohort of homosexual men". AIDS. 1 (2): 77–82. PMID 2966631. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help) - ↑ Talal AH, Irwin CE, Dieterich DT, Yee H, Zhang L (2001). "Effect of HIV-1 infection on lymphocyte proliferation in gut-associated lymphoid tissue". J. Acquir. Immune Defic. Syndr. 26 (3): 208–17. PMID 11242193. Retrieved 2012-05-25. Unknown parameter
|month=ignored (help) - ↑ Poles MA, Boscardin WJ, Elliott J, Taing P, Fuerst MM, McGowan I, Brown S, Anton PA (2006). "Lack of decay of HIV-1 in gut-associated lymphoid tissue reservoirs in maximally suppressed individuals". J. Acquir. Immune Defic. Syndr. 43 (1): 65–8. doi:10.1097/01.qai.0000230524.71717.14. PMID 16936559. Retrieved 2012-05-25. Unknown parameter
|month=ignored (help) - ↑ Jones JL, Hanson DL, Dworkin MS, Alderton DL, Fleming PL, Kaplan JE, Ward J (1999). "Surveillance for AIDS-defining opportunistic illnesses, 1992-1997". MMWR CDC Surveill Summ. 48 (2): 1–22. PMID 12412613. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help)