HIV AIDS pathophysiology: Difference between revisions
| Line 98: | Line 98: | ||
The transmission of the virus from the mother to the child can occur ''[[in utero]]'' during the last weeks of pregnancy and at childbirth. | The transmission of the virus from the mother to the child can occur ''[[in utero]]'' during the last weeks of pregnancy and at childbirth. | ||
<!--- CONTENT FROM HIV PAGE | |||
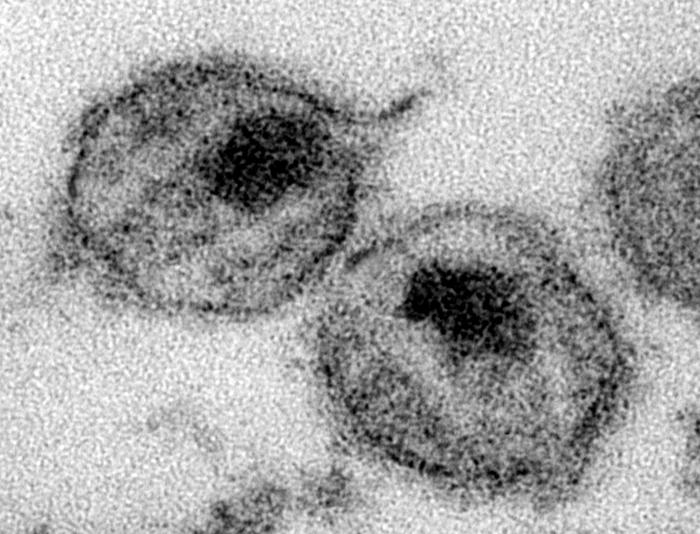
HIV is transmitted as single-stranded, positive-[[Sense (molecular biology)|sense]], enveloped [[RNA virus]]es. Upon entry of the target cell, the viral RNA [[genome]] is converted to double-stranded [[DNA]] by a virally encoded [[reverse transcriptase]] that is present in the virus particle. This viral DNA is then integrated into the cellular DNA by a virally encoded [[integrase]] so that the genome can be [[Transcription (genetics)|transcribed]]. Once the virus has infected the cell, two pathways are possible: either the virus becomes [[Incubation period|latent]] and the infected cell continues to function, or the virus becomes active and replicates, and a large number of virus particles are liberated that can then infect other cells. | |||
Infection with HIV-1 is associated with a progressive decrease of the CD4<SUP>+</SUP> T cell count and an increase in [[viral load]]. The stage of infection can be determined by measuring the patient's CD4<SUP>+</SUP> T cell count, and the level of HIV in the blood. | |||
==Pathophysiology== | |||
[[Image:Hiv-timecourse.png|400px|thumb|left|A generalized graph of the relationship between HIV copies (viral load) and CD4 counts over the average course of untreated HIV infection; any particular individual's disease course may vary considerably. | |||
{{legend-line|blue solid 2px|CD4<sup>+</sup> T cell count (cells per µL)}} | |||
{{legend-line|red solid 2px|HIV RNA copies per mL of plasma}} | |||
]] | |||
The initial infection with HIV generally occurs after transfer of body fluids from an infected person to an uninfected one. | |||
===Stage 1: Primary HIV Infection=== | |||
*The first stage of infection, the primary, or acute infection, is a period of rapid viral replication that immediately follows the individual's exposure to HIV leading to an abundance of virus in the peripheral blood with levels of HIV commonly approaching several million viruses per mL.<ref name=Piatak> {{cite journal | author=Piatak, M., Jr, Saag, M. S., Yang, L. C., Clark, S. J., Kappes, J. C., Luk, K. C., Hahn, B. H., Shaw, G. M. and Lifson, J.D. | title=High levels of HIV-1 in plasma during all stages of infection determined by competitive PCR | journal=Science | year=1993 | pages=1749-1754 | volume=259 | issue=5102 | pmid=8096089 | doi=10.1126/science.8096089}}</ref> This response is accompanied by a marked drop in the numbers of circulating CD4<sup>+</sup> T cells. This acute viremia is associated in virtually all patients with the activation of [[cytotoxic T cell|CD8<sup>+</sup> T cells]], which kill HIV-infected cells, and subsequently with antibody production, or [[seroconversion]]. | |||
* The CD8<sup>+</sup> T cell response is thought to be important in controlling virus levels, which peak and then decline, as the CD4<sup>+</sup> T cell counts rebound to around 800 cells per mL (the normal value is 1200 cells per mL ). | |||
* A good CD8<sup>+</sup> T cell response has been linked to slower disease progression and a better prognosis, though it does not eliminate the virus.<ref name=Pantaleo1998> | |||
{{cite journal | |||
| author=Pantaleo G, Demarest JF, Schacker T, Vaccarezza M, Cohen OJ, Daucher M, Graziosi C, Schnittman SS, Quinn TC, Shaw GM, Perrin L, Tambussi G, Lazzarin A, Sekaly RP, Soudeyns H, Corey L, Fauci AS. | title=The qualitative nature of the primary immune response to HIV infection is a prognosticator of disease progression independent of the initial level of plasma viremia | journal=Proc Natl Acad Sci U S A. | year=1997 | pages=254-258 | volume=94 | issue=1 | pmid=8990195 | |||
}}</ref> | |||
*During this period (usually 2-4 weeks post-exposure) most individuals (80 to 90%) develop an influenza or mononucleosis-like illness called [[acute HIV infection]]. | |||
*The most common '''''symptoms''''' of which may include [[fever]], [[lymphadenopathy]], [[pharyngitis]], [[rash]], [[myalgia]], [[malaise]], mouth and esophagal sores, and may also include, but less commonly, [[headache]], [[nausea]] and [[vomiting]], enlarged liver/spleen, [[weight loss]], [[Candidiasis|thrush]], and neurological symptoms. Infected individuals may experience all, some, or none of these symptoms. | |||
*The '''duration''' of symptoms varies, averaging 28 days and usually lasting at least a week.<ref name=Kahn> | |||
{{cite journal | |||
| author=Kahn, J. O. and Walker, B. D. | title=Acute Human Immunodeficiency Virus type 1 infection | journal=N. Engl. J. Med. | year=1998 | pages=33-39 | volume=331 | issue=1 | pmid=9647878 | |||
}}</ref> | |||
*Because of the nonspecific nature of these symptoms, they are often not recognized as signs of HIV infection. Even if patients go to their doctors or a hospital, they will often be ''misdiagnosed'' as having one of the more common infectious diseases with the same symptoms. Consequently, these primary symptoms are not used to diagnose HIV infection as they do not develop in all cases and because many are caused by other more common diseases. However, recognizing the syndrome can be important because the patient is much more infectious during this period.<ref name="pmid11187417">{{cite journal |author=Daar ES, Little S, Pitt J, ''et al'' |title=Diagnosis of primary HIV-1 infection. Los Angeles County Primary HIV Infection Recruitment Network |journal=Ann. Intern. Med. |volume=134 |issue=1 |pages=25–9 |year=2001 |pmid=11187417 |doi=}}</ref> | |||
{| class="wikitable sortable" | |||
|+ History and physical findings for primary HIV infection<ref name="pmid11187417">{{cite journal |author=Daar ES, Little S, Pitt J, ''et al'' |title=Diagnosis of primary HIV-1 infection. Los Angeles County Primary HIV Infection Recruitment Network |journal=Ann. Intern. Med. |volume=134 |issue=1 |pages=25–9 |year=2001 |pmid=11187417 |doi=}}</ref> | |||
! !! [[sensitivity (tests)|sensitivity]]!! [[specificity (tests)|specificity]] | |||
|- | |||
| Fever || 88% || 50% | |||
|- | |||
| Malaise || 73%|| 58% | |||
|- | |||
| Myalgia || 60%|| 74% | |||
|- | |||
| Rash || 58%|| 79% | |||
|- | |||
| Headache|| 55%|| 56% | |||
|- | |||
| Night sweats || 50%|| 68% | |||
|- | |||
| Sore throat || 43%|| 51% | |||
|- | |||
| Lymphadenopathy|| 38%|| 71% | |||
|- | |||
| Arthralgia || 28%|| 87% | |||
|- | |||
| Nasal congestion|| 18%|| 62% | |||
|} | |||
=== Stage 2: Clinically Asymptomatic Stage=== | |||
*A strong immune defense reduces the number of viral particles in the blood stream, marking the end of the acute HIV infection and the start of the infection's [[incubation period|clinical latency]] stage, which, in turn, may be succeeded by true [[AIDS]]. | |||
*Clinical latency can vary between two weeks and 20 years. | |||
*During this early phase of infection, HIV is active within [[Lymphatic system|lymphoid organs]], where large amounts of virus become trapped in the follicular [[dendritic cell]]s (FDC) network.<ref name=burton> | |||
{{cite journal | |||
| author=Burton GF, Keele BF, Estes JD, Thacker TC, Gartner S. | title=Follicular dendritic cell contributions to HIV pathogenesis | journal=Semin Immunol. | year=2002 | pages=275-284 | volume=14 | issue=4 | pmid=12163303 | |||
}}</ref> | |||
*The surrounding tissues that are rich in CD4<SUP>+</SUP> T cells may also become infected, and viral particles accumulate both in infected cells and as free virus. | |||
*Individuals who are in this phase are still infectious. | |||
*During this time, [[Helper T cell|CD4<SUP>+</SUP> CD45RO<SUP>+</SUP> T cells]] carry most of the proviral load.<ref name=clapham> | |||
{{cite journal | |||
| author=Clapham PR, McKnight A. | title=HIV-1 receptors and cell tropism | journal=Br Med Bull. | year=2001 | pages=43-59 | volume=58 | issue=4 | pmid=11714623 | |||
}}</ref> | |||
===Stage 3: Symptomatic HIV Infection=== | |||
*When CD4<sup>+</sup> T cell numbers decline below a critical level, cell-mediated immunity is lost, and infections with a variety of opportunistic microbes appear. | |||
*The first '''''symptoms''''' often include moderate and unexplained weight loss, recurring respiratory tract infections (such as [[sinusitis]], [[bronchitis]], [[otitis media]], [[pharyngitis]]), [[prostatitis]], skin rashes, and oral ulcerations. | |||
*Common '''''opportunistic infections and tumors''''', most of which are normally controlled by robust CD4<sup>+</sup> T cell-mediated immunity then start to affect the patient. | |||
*Typically, resistance is lost early on to oral Candida species and to ''Mycobacterium tuberculosis'', which leads to an increased susceptibility to [[oral candidiasis]] (thrush) and [[tuberculosis]]. | |||
*Later, reactivation of latent [[Herpesviridae|herpes viruses]] may cause worsening recurrences of [[herpes simplex]] eruptions, [[shingles]], [[Epstein-Barr virus]]-induced B-cell lymphomas, or [[Kaposi's sarcoma]], a [[tumor]] of [[endothelial cell]]s that occurs when HIV proteins such as Tat interact with [[Kaposi's sarcoma-associated herpesvirus|Human Herpesvirus-8]]. | |||
*Pneumonia caused by the fungus ''[[Pneumocystis jirovecii]]'' is common and often fatal. | |||
===Stage 4: Progression from HIV infection to AIDS=== | |||
In the final stages of AIDS, infection with [[cytomegalovirus]] (another herpes virus) or [[Mycobacterium avium complex]] is more prominent. Not all patients with AIDS get all these infections or tumors, and there are other tumors and infections that are less prominent but still significant. | |||
---> | |||
==Related Chapters== | ==Related Chapters== | ||
* [[AIDS defining clinical condition]] | * [[AIDS defining clinical condition]] | ||
Revision as of 14:35, 2 October 2014
|
AIDS Microchapters |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
HIV AIDS pathophysiology On the Web |
|
American Roentgen Ray Society Images of HIV AIDS pathophysiology |
|
Risk calculators and risk factors for HIV AIDS pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Human Immunodeficiency virus causes AIDS by depleting CD4+ T helper lymphocytes. T lymphocytes are essential to the immune response and without them, the body cannot fight infections or kill cancerous cells. Thus the weakened immune system allows opportunistic infections and neoplastic processes. The mechanism of CD4+ T cell depletion differs in the acute and chronic phases, to sum it all AIDS has a complex pathophysiology.[1] To read about the progression of HIV infection to AIDS, click here
Pathophysiology
- The pathophysiologic progression from acute HIV infection to AIDS is described in the chapter HIV infection pathophysiology. This chapter explains the pathophysiology of AIDS.
- The specific decline in CD44 helper T cells, result in inversion of the normal CD4/CD8 T cell ratio. It also cause dysregulation of B cell antibody production.[2][3]
- B cell exhibit increased expression of markers of activation and proliferation.[4] Terminal differentiation of B cell leads to increased immunoglobulin secretion, which further causes polyclonal hypergammaglobulinemia producing non-specific antibodies.[5] This also explain the reason for increases risk of bacterial infection inspite of high circulating levels of immunoglobulins.
- The immune response to antigens begins to decline, as a result, the host fails to respond adequately to opportunistic infections and normally harmless commensals.
- The infections tend to be non-bacterial (i.e fungal, Viral) because the defect preferentially involves cellular immunity.
- Humoral immunity generally improves dramatically after the initiation of ART.
Role of GALT in Pathogenesis
- Port of entry for HIV infection, is mostly through direct blood inoculation or exposure through genital mucosal surface. The gastrointestinal tract contains a large amount of lymphoid tissue, making it an ideal place for replication of Human Immunodeficiency Virus. GALT plays a role in HIV replication. [6]
- GALT has been found to have the following characteristics:
- Site of early viral seeding.
- Establishment of the pro-viral reservoir.
- The proviral GALT reservoir contributes to the following:
- Difficulty in controlling the infection.
- Difficulty in reducing the level of HIV provirus through sustained ART.[7] Various studies measuring the CD44 in GALT, have shown the relatively less reconstitution with ART, than that observed in peripheral blood.[8][9]
Coinfections
Effect of Geographic Area on Opportunistic Infection
The opportunistic infection in AIDS patient reflect the pathogen that are common in that area.
- In USA: Person with AIDS tends to present with commensal organism such as Pneumoncystis and Candida.
- In a study done by National Center of HIV/AIDS,[10] PCP was the most common AIDS-defining opportunistic infection to occur first.
- PCP was the first OI to occur for 36% of HIV-infected persons.
- The most common incident AIDS-defining OI (274 cases per 1000 person-years).
- The most common AIDS-defining OI to have occurred during the course of AIDS (53% of persons who died with AIDS had PCP diagnosed at some time during their course of AIDS).
- In a study done by National Center of HIV/AIDS,[10] PCP was the most common AIDS-defining opportunistic infection to occur first.
- In developing nations: AIDS patients tends to present with Tuberculosis, as it is more prevalent in those countries.
A. The Major Pulmonary Illnesses
-
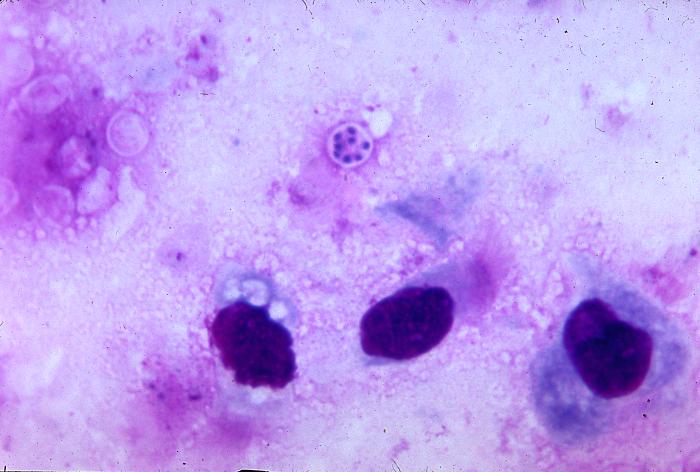
Pneumocystis jiroveci is present in this lung impression smear, using Giemsa stain
-
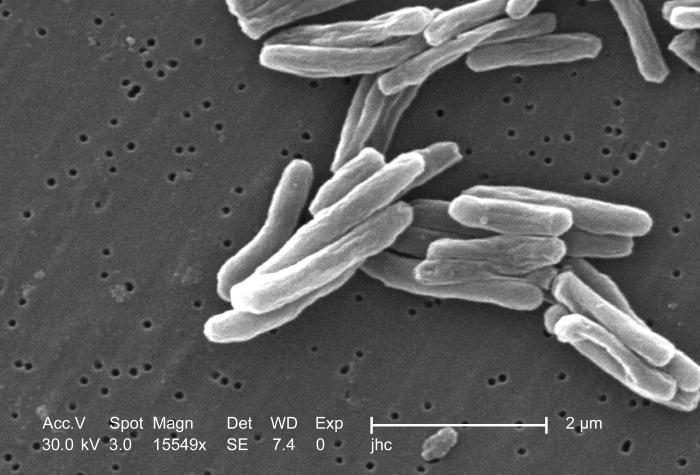
Scanning electron micrograph (SEM) of a number of Gram-positive Mycobacterium tuberculosis bacteria
Pneumocystis jiroveci Pneumonia
Pneumocystis jiroveci pneumonia (originally known as Pneumocystis carinii pneumonia, often abbreviated PCP) is relatively rare in normal, immunocompetent people but common among HIV-infected individuals. Before the advent of effective treatment and diagnosis in Western countries it was a common immediate cause of death. In developing countries, it is still one of the first indications of AIDS in untested individuals, although it does not generally occur unless the CD4 count is less than 200 per µl (Feldman, 2005).
Tuberculosis
Among infections associated with HIV, Tuberculosis (TB) is unique in that it may be transmitted to immunocompetent persons via the respiratory route, is easily treatable once identified, may occur in early-stage HIV disease, and is preventable with drug therapy. However, multi-drug resistance is a potentially serious problem. Even though its incidence has declined because of the use of directly observed therapy and other improved practices in Western countries, this is not the case in developing countries where HIV is most prevalent. In early-stage HIV infection (CD4 count >300 cells per µl), TB typically presents as a pulmonary disease. In advanced HIV infection, TB may present atypically and extrapulmonary TB is common infecting bone marrow, bone, urinary and gastrointestinal tracts, liver, regional lymph nodes, and the central nervous system (Decker and Lazarus, 2000).
B. The Major Gastro-intestinal Illnesses
Esophagitis
Esophagitis is an inflammation of the lining of the lower end of the esophagus (gullet or swallowing tube leading to the stomach). In HIV infected individuals, this could be due to fungus (candidiasis), virus (herpes simplex-1 or cytomegalovirus). In rare cases, it could be due to mycobacteria (Zaidi and Cervia, 2002).
Unexplained Chronic Diarrhea
In HIV infection, there are many possible causes of diarrhea, including common bacterial (Salmonella, Shigella, Listeria, Campylobacter, or Escherichia coli) and parasitic infections, and uncommon opportunistic infections such as cryptosporidiosis, microsporidiosis, Mycobacterium avium complex (MAC) and cytomegalovirus (CMV) colitis. Diarrhea may follow a course of antibiotics (common for Clostridium difficile). It may also be a side effect of several drugs used to treat HIV, or it may simply accompany HIV infection, particularly during primary HIV infection. In the later stages of HIV infection, diarrhea is thought to be a reflection of changes in the way the intestinal tract absorbs nutrients, and may be an important component of HIV-related wasting (Guerrant et al., 1990).
C. The Major Neurological illnesses
Toxoplasmosis
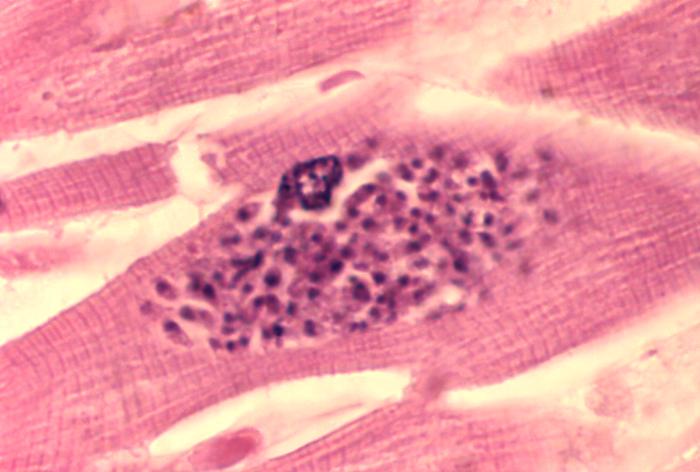
Toxoplasmosis is a disease caused by the single-celled parasite called Toxoplasma gondii. T. gondii usually infects the brain causing toxoplasma encephalitis. It can also infect and cause disease in the eyes and lungs (Luft and Chua, 2000).
Progressive Multifocal Leukoencephalopathy
Progressive multifocal leukoencephalopathy (PML) is a demyelinating disease, in which the myelin sheath covering the axons of nerve cells is gradually destroyed, impairing the transmission of nerve impulses. It is caused by a virus called JC virus which occurs in 70% of the population in latent form, causing disease only when the immune system has been severly weakened, as is the case for AIDS patients. It progresses rapidly, usually causing death within months of diagnosis (Sadler and Nelson, 1997).
HIV-associated Dementia
HIV-1 associated dementia (HAD) is a metabolic encephalopathy induced by HIV infection and fueled by immune activation of brain macrophages and microglia (Gray et al., 2001). These cells are actively infected with HIV and secrete neurotoxins of both host and viral origin. Specific neurologic impairments are manifested by cognitive, behavioral, and motor abnormalities that occur after years of HIV infection and is associated with low CD4+ T cell levels and high plasma viral loads. Prevalence is between 15-30% in Western countries (Heaton et al., 1995; White et al., 1995) and has only been seen in 1-2% of India based infections (Satischandra et al., 2000; Wadia et al., 2001).
D. HIV-associated malignancies
Patients with HIV infection are susceptible to a number of malignancies (Yarchoan et al., 2005). The most common is Kaposi's sarcoma, and the appearance of this tumor in young gay men in New York in 1981 was one of the first signals of the AIDS epidemic. In addition, patients with HIV infection have a higher incidence of certain high grade B cell lymphomas, especially Burkitt-like and large cell lymphomas. These tumors, as well as aggressive cervical cancer in women, confer a diagnosis of AIDS in patients with HIV infection.
E. The Major Dermatological illnesses
AIDS-associated Kaposi sarcoma or KS-AIDS presents with cutaneous lesions that begin as one or several red to purple-red macules, rapidly progressing to papules, nodules, and plaques, with a predilection for the head, neck, trunk, and mucous membranes.
-
Kaposi's sarcoma lesion commonly found in patients with stage IV AIDS
-
Intraoral Kaposi’s sarcoma lesion with an overlying candidiasis infection
Transmission
The three main transmission routes of HIV are sexual contact, exposure to infected body fluids or tissues, and from mother to fetus or child during perinatal period. It is possible to find HIV in the saliva, tears, and urine of infected individuals, but there are no recorded cases of infection by these secretions, and the risk of infection is negligible.
Transmission of HIV depends on the infectiousness of the index case and the susceptibility of the uninfected partner. Exposure to infected body fluids is particularly relevant to intravenous drug users, hemophiliacs and recipients of blood transfusions and blood products. Sharing and reusing syringes contaminated with HIV-infected blood represents a major risk for infection with not only HIV, but also hepatitis B and hepatitis C.
The transmission of the virus from the mother to the child can occur in utero during the last weeks of pregnancy and at childbirth.
Related Chapters
References
- ↑ Guss DA (1994). "The acquired immune deficiency syndrome: an overview for the emergency physician, Part 1". J Emerg Med. 12 (3): 375–84. PMID 8040596.
|access-date=requires|url=(help) - ↑ Frazer IH, Mackay IR, Crapper RM, Jones B, Gust ID, Sarngadharan MG, Campbell DC, Ungar B (1986). "Immunological abnormalities in asymptomatic homosexual men: correlation with antibody to HTLV-III and sequential changes over two years". Q. J. Med. 61 (234): 921–33. PMID 3498182. Retrieved 2012-05-24. Unknown parameter
|month=ignored (help) - ↑ Schechter MT, Boyko WJ, Craib KJ, McLeod A, Willoughby B, Douglas B, Constance P, O'Shaughnessey M (1987). "Effects of long-term seropositivity to human immunodeficiency virus in a cohort of homosexual men". AIDS. 1 (2): 77–82. PMID 2966631. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help) - ↑ Moir S, Malaspina A, Pickeral OK, Donoghue ET, Vasquez J, Miller NJ, Krishnan SR, Planta MA, Turney JF, Justement JS, Kottilil S, Dybul M, Mican JM, Kovacs C, Chun TW, Birse CE, Fauci AS (2004). "Decreased survival of B cells of HIV-viremic patients mediated by altered expression of receptors of the TNF superfamily". J. Exp. Med. 200 (7): 587–99. PMID 15508184. Retrieved 2012-05-25. Unknown parameter
|month=ignored (help) - ↑ Moir S, Malaspina A, Ogwaro KM, Donoghue ET, Hallahan CW, Ehler LA, Liu S, Adelsberger J, Lapointe R, Hwu P, Baseler M, Orenstein JM, Chun TW, Mican JA, Fauci AS (2001). "HIV-1 induces phenotypic and functional perturbations of B cells in chronically infected individuals". Proc. Natl. Acad. Sci. U.S.A. 98 (18): 10362–7. doi:10.1073/pnas.181347898. PMC 56966. PMID 11504927. Retrieved 2012-05-25. Unknown parameter
|month=ignored (help) - ↑ Talal AH, Irwin CE, Dieterich DT, Yee H, Zhang L (2001). "Effect of HIV-1 infection on lymphocyte proliferation in gut-associated lymphoid tissue". J. Acquir. Immune Defic. Syndr. 26 (3): 208–17. PMID 11242193. Retrieved 2012-05-25. Unknown parameter
|month=ignored (help) - ↑ Poles MA, Boscardin WJ, Elliott J, Taing P, Fuerst MM, McGowan I, Brown S, Anton PA (2006). "Lack of decay of HIV-1 in gut-associated lymphoid tissue reservoirs in maximally suppressed individuals". J. Acquir. Immune Defic. Syndr. 43 (1): 65–8. doi:10.1097/01.qai.0000230524.71717.14. PMID 16936559. Retrieved 2012-05-25. Unknown parameter
|month=ignored (help) - ↑ Guadalupe M, Reay E, Sankaran S, Prindiville T, Flamm J, McNeil A, Dandekar S (2003). "Severe CD4+ T-cell depletion in gut lymphoid tissue during primary human immunodeficiency virus type 1 infection and substantial delay in restoration following highly active antiretroviral therapy". J. Virol. 77 (21): 11708–17. PMC 229357. PMID 14557656. Retrieved 2012-05-25. Unknown parameter
|month=ignored (help) - ↑ Shacklett BL, Cox CA, Sandberg JK, Stollman NH, Jacobson MA, Nixon DF (2003). "Trafficking of human immunodeficiency virus type 1-specific CD8+ T cells to gut-associated lymphoid tissue during chronic infection". J. Virol. 77 (10): 5621–31. PMC 154016. PMID 12719554. Retrieved 2012-05-25. Unknown parameter
|month=ignored (help) - ↑ Jones JL, Hanson DL, Dworkin MS, Alderton DL, Fleming PL, Kaplan JE, Ward J (1999). "Surveillance for AIDS-defining opportunistic illnesses, 1992-1997". MMWR CDC Surveill Summ. 48 (2): 1–22. PMID 12412613. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help)
- Pages using citations with accessdate and no URL
- Pages with citations using unsupported parameters
- CS1 maint: Multiple names: authors list
- HIV/AIDS
- Disease
- Immune system disorders
- Infectious disease
- Viral diseases
- Pandemics
- Sexually transmitted infections
- Syndromes
- Virology
- AIDS origin hypotheses
- Medical disasters
- Immunodeficiency
- Microbiology