Glaucoma physical examination
|
Glaucoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Glaucoma physical examination On the Web |
|
American Roentgen Ray Society Images of Glaucoma physical examination |
|
Risk calculators and risk factors for Glaucoma physical examination |
Please help WikiDoc by adding more content here. It's easy! Click here to learn about editing.
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Rohan Bir Singh, M.B.B.S.[2]
Ocular Examination
- External adnexae
- Useful in determining the presence of a variety of conditions associated with secondary glaucomas as well as external ocular manifestations of glaucoma therapy.
- Pupils
- Pupillary responses are one measure of compliance in patients who are on miotic therapy. Corectopia, ectropion uveae and pupillary abnormalities may be observed in some forms of glaucoma. Testing for a RAPD may detect asymmetric optic nerve damage in glaucoma.
- Conjunctiva
- conjunctival injection can lead to acutely elevated IOP during chronic use of sympathomimetic drops
- massive episcleral venous dilation can cause chronically elevated IOP
- black adrenochrome deposits due to chronic use of epinephrine derivative drops
- use of topical antiglaucoma medication may lead to decreased tear production, allergic reactions, foreshortening of the conjunctival fornices, scarring.
- to measure size, height, degree of vascularization, integrity of a filtering bleb if present
- Episclera and sclera
- dilation of the episcleral vessels can cause elevated episcleral venous pressure.
- sentinel vessels in case of an intraocular tumor
- thinning or staphylomatous areas
- Cornea
- enlargement of the cornea, breaks in Descemet’s membrane (Haab’s striae) can lead to developmental glaucoma
- punctate epithelial defects (especially in the inferonasal interpalpebral region) secondary to medication toxicity
- microcystic epithelial edema → acute elevated IOP
- endothelial abnormalities → underlying associated secondary glaucoma
- Krukenberg spindle in pigmentary glaucoma
- deposition of exfoliation material in exfoliation syndrome
- keratic precipitates in uveitic glaucoma
- guttae in Fuchs endothelial dystrophy
- irregular and vesicular lesions in posterior polymorphous dystrophy
- ‘beaten bronze’ appearance in the iridocorneal endothelial syndrome
- anteriorly displaced Schwalbe’s line → Axenfeld-Rieger syndrome
- traumatic or surgical corneal scars, corneal thickness
- Anterior chamber
- width of the chamber angle → van Herick method (A narrow slit beam is directed at an angle of 60˚ onto the cornea just anterior to the limbus. If the distance from the anterior iris surface to the posterior surface of the cornea is less than one fourth the thickness of the cornea, the angle may be narrow)
- uniformity of depth of the anterior chamber (iris bombe, iris masses)
- inflammatory cells, red cells, ghost cells, fibrin, vitreous
- Iris
- heterochromia, iris atrophy, transillumination defects, ectropion uveae, corectopia, nevi, nodules, exfoliative material
- early stages of neovascularization of the anterior segment → fine tufts around
the pupillary margin, fine network of vessels on the surface of the iris.
- evidence of trauma (sphincter tear, iridodonesis), iris pigmentation \
- Lens
- exfoliative material, phacodonesis, subluxation, dislocation
- lens size, shape and clarity
- posterior subcapsular cataract → chronic corticosteroid use
- presence, type and position of an IOL
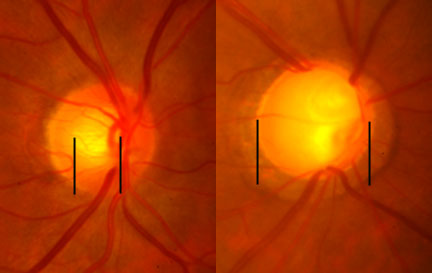
- Fundus
- careful assessment of the optic disc
- hemorrhage, effusion, masses, inflammatory lesion, retinovascular occlusion, diabetic retinopathy, retinal detachment
-
0.5 to 0.9 cup-to-disc ratio. Increase seen with open angle glaucoma.
-
Glaucoma
-
A normal range of vision. Courtesy NIH National Eye Institute
-
The same view with advanced vision loss from glaucoma.