Giant cell myocarditis
|
Myocarditis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Giant cell myocarditis On the Web |
|
American Roentgen Ray Society Images of Giant cell myocarditis |
|
Risk calculators and risk factors for Giant cell myocarditis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor: Cafer Zorkun, M.D., Ph.D. [2]
Synonyms and keywords: GCM; idiopathic giant cell myocarditis; IGCM.
Overview
Giant cell myocarditis is a rare but often fatal inflammatory process involving the myocardium. Other than cardiac transplantation, there is no known effective treatment for giant cell mycoarditis.
Pathophysiology
Data from a Lewis Rat model and from observational human studies suggest that giant cell myocarditis is mediated by T lymphocytes. The disease may therefore respond to treatment aimed at attenuating T cell function.
Numerous autoimmune disorders have been associated with giant cell myocarditis in case reports, but the true magnitude of the association and causality of any association (if any) is not clear.
Gross Pathology
Images shown below are courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
-
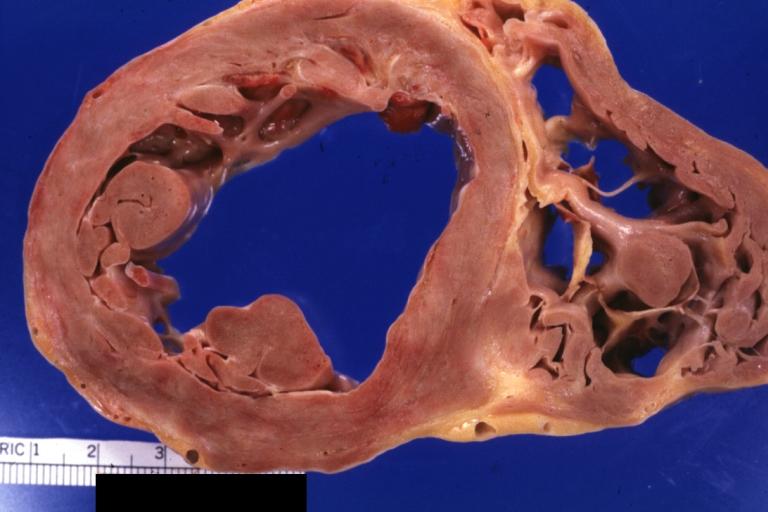
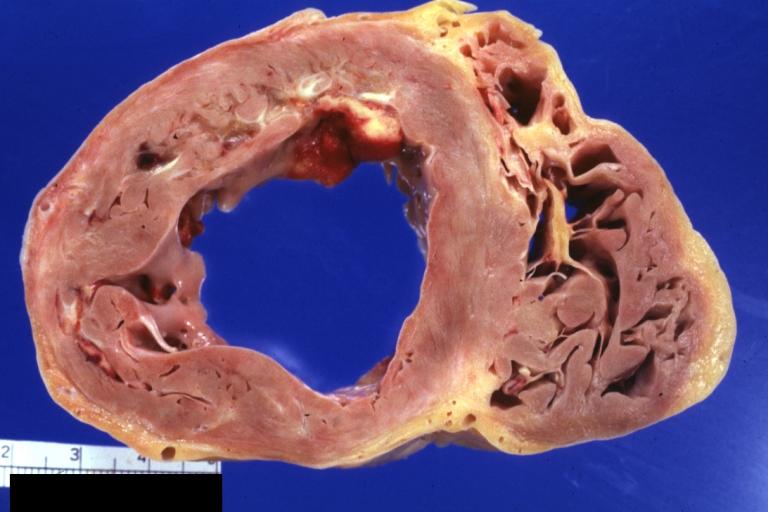
Giant Cell Myocarditis: Gross dilated LV with focal fibrosis
-
Giant Cell Myocarditis: Gross dilated LV with focal fibrosis
-
Giant Cell Myocarditis: Gross dilated LV with focal fibrosis
Microscopic Pathology
Images shown below are courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
-
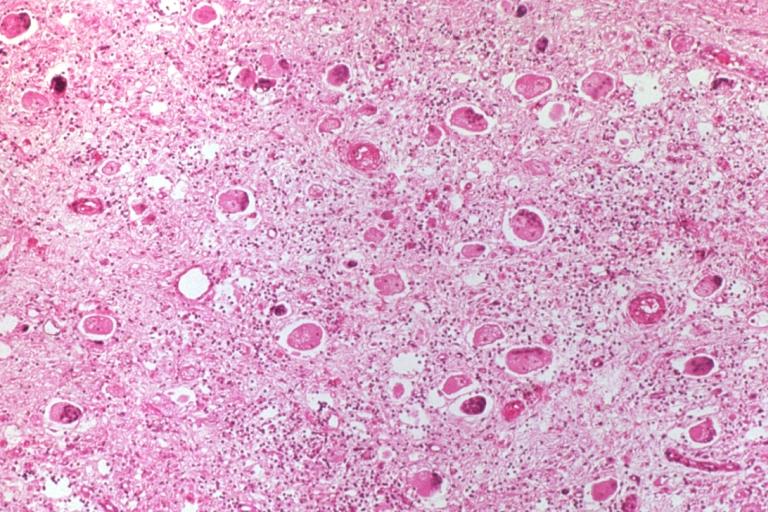
Boecks Sarcoid Giant Cell Myocarditis
-
Boecks Sarcoid Giant Cell Myocarditis
-
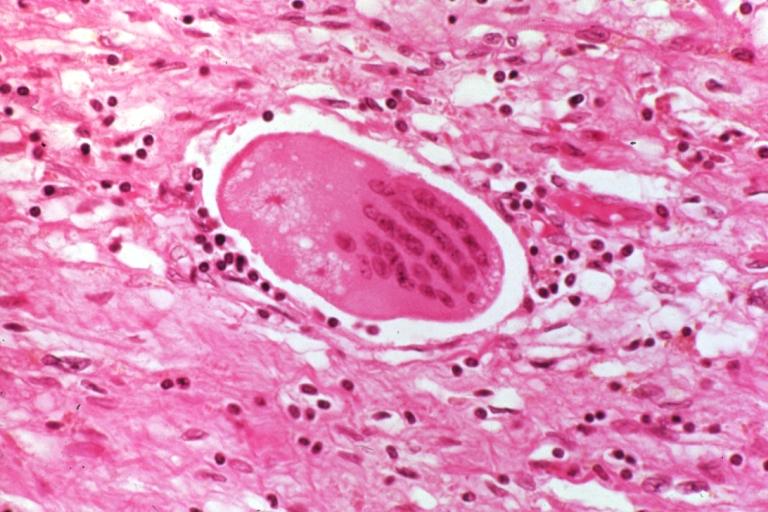
22-year-old man was seropositive for HIV-1 and died suddenly. There was widespread inflammation of the myocardium with giant cells, resembling giant cell myocarditis, that may have represented a precursor to lymphoma.
-
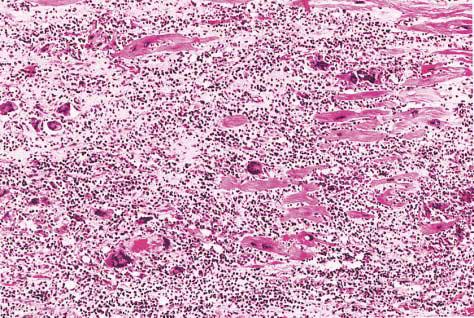
Diffuse geographic myocardial necrosis at low-power magnification. Numerous giant cells (arrows) can be identified within the inflammatory infiltrate (hematoxylin and eosin, x100)
-
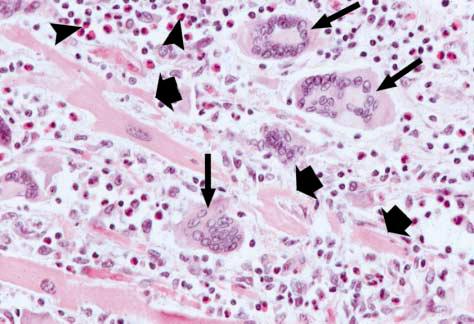
Multinucleated giant cells (long arrows) are seen adjacent to degenerating myocytes (short arrows). The cellular infiltrate contains lymphocytes, histiocytes, and collections of eosinophils (arrowheads) (hematoxylin and eosin, x400)
Epidemiology and Demographics
Giant cell myocarditis often affects young otherwise healthy individuals.
Natural History, Complications and Prognosis
Complications
Giant cell myocarditis is generally characterized by progressive congestive heart failure, and is frequently associated with refractory ventricular arrhythmias. The majority of patients die secondary to congestive heart failure, although some have survived for long periods, often after immunosuppressive treatment.[1][2]
Prognosis
The rate of death or heart transplantation is approximately 70% at one year. Survival following cardiac transplantation is approximately 71% at five years despite a 25% rate of giant cell infiltration in the donor heart.
Diagnosis
Endomyocardial Biopsy
The Giant Cell Myocarditis Registry is a clinical and pathologic database from 63 cases of giant cell myocarditis gathered from 36 medical centers. Using pathologic examination at transplantation or autopsy as the gold standard, the sensitivity of endomyocardial biopsy in detecting giant cell myocarditis was 80% in the GCM registry. [3]
Electrocardiogram
Heart block is frequently observed in giant cell myocarditis.
Treatment
Immunosuppressive Therapy
Immunosuppressive therapy including muromonab-CD3, cyclosporine and/or azathioprine, and steroids has been used to treat giant cell myocarditis. Giant Cell Myocarditis Registry subjects who received cyclosporine and/or azathioprine, with steroids and sometimes muromonab-CD3 had prolonged transplant-free survival: 12.6 months vs 3.0 months for those patients treated with no immunosuppression.[4] While this data is encouraging, it should be noted that it is drawn from a modest registry experience and randomized placebo-controlled trials are lacking.
Cardiac Transplantation
Giant cell myocarditis may recur after cardiac transplantation but may respond to augmented immunosuppression.
References
- ↑ Desjardins V, Pelletier G, Leung TK, Waters D. Successful treatment of severe heart failure caused by idiopathic giant cell myocarditis. Can J Cardiol 1992;8:788-92
- ↑ Ren H, Poston RS Jr, Hruban RH, Baumgartner WA, Baughman KL, Hutchins GM. Long survival with giant cell myocarditis. Mod Pathol 1993;6:402-7.
- ↑ Cooper LT, Berry GJ, Shabetai R.Idiopathic Giant-Cell Myocarditis — Natural History and Treatment. N Engl J Med. 1997 Jun 26;336(26):1860-6
- ↑ Cooper LT, Berry GJ, Shabetai R.Idiopathic Giant-Cell Myocarditis — Natural History and Treatment. N Engl J Med. 1997 Jun 26;336(26):1860-6