Flock worker's lung: Difference between revisions
Jump to navigation
Jump to search
Sara Mohsin (talk | contribs) |
Sara Mohsin (talk | contribs) No edit summary |
||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{ | {{Flock worker's lung}} | ||
{{CMG}} {{AE}} | {{CMG}} {{AE}} | ||
Revision as of 21:35, 13 August 2020
|
Flock worker's lung Microchapters |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief:
Synonyms and keywords: Synonym 1; Synonym 2; Synonym 3
Overview
Flock Worker's Lung.
Historical Perspective
- Since 1975, published case reports have raised suspicion of a respiratory hazard associated with various synthetic fibers, including polyester, nylon, and acrylic dust.
- Early reports in 1974 and 1981 of workplace evaluations by National Institute of Occupational Safety and Health (NIOSH) investigators attributed respiratory symptoms among workers to irritant properties of nonrespirable flock fibers on the upper airways but did not pursue the possibility of lung disease associated with flock work [1]
- During 1990 and 1991, five workers from a nylon flock processing plant in Ontario presented with cough and dyspnea.[2]
- In 1995 and 1996, two workers from a similar nylon flock processing plant in Rhode Island presented separately to the same physician with cough and dyspnea
- The initial working diagnosis for the lung disease in these two workers was work-related hypersensitivity pneumonitis. With additional case finding investigation at the Rhode Island location, a total of eight cases among the approximately 150 workers at the plant were identified by January 1998 based upon a screening questionnaire (symptoms of cough and dyspnea), pulmonary function abnormalities (restrictive pattern with reduced diffusing capacity), radiographic findings and/or histological findings on tissue obtained by open lung or transbronchial lung biopsy .Based upon the aggregate histopathological results from biopsied cases, the disease process was not thought to be hypersensitivity pneumonitis.[2]
- "flock worker's lung" formally came to known in 1998, when researchers from NIOSH published the results of an epidemiological investigation of outbreaks in Ontario and Rhode Island.
- Previously, interstitial lung disease in flock workers was incorrectly attributed to mycotoxins present in contaminated adhesive.[1]
Classification
The disease currently still has not been stratified.
Pathophysiology
- Flock consists of short fibers that are cut from long filaments and glued to backing material such as cloth to provide a fuzzy, carpet-like surface texture. They are usually prepared from synthetic materials such as nylon, rayon, or polypropylene. The cutting process results in formation of airborne particles or fibers in the respirable range. Inhalation of flock dust causes an interstitial lung disease.[3]
- Preliminary toxicologic studies suggest that ultrafine respirable fragments of nylon cause an acute inflammatory lung injury in rats after a single intratracheal instillation. However, flock finishing agents or other components of the particulate matter present in the air of flock processing plants cannot yet be ruled out.
- The interstitial pneumonitis we have studied among nylon flock processing workers has a histopathological pattern— bronchiolar and peribronchiolar lymphocytic inflammation and lymphoid hyperplasia—which suggests an inflammatory and possibly immunologic response to a respirable toxic agent [4]
- In one study microscopic examination of polypropylene fibre-exposed lungs revealed a dose-dependent increase in cellularity (especially macrophage infiltration), but no fibrosis. In another study , the researchers found high serum IL-8 and TNF-α levels in the polypropylene flocking workers. Furthermore, these levels showed a negative correlation with DL,CO. These results suggest that IL-8 and TNF-α may act as key mediators for inflammatory lung injury in the pathogenesis of polypropylene flocking worker's lung.[5]
Causes
- FWL results from the inhalation of airborne nylon fibers at work. Nylon fibers are used in making products for upholstery, automobiles, carpet, and apparel.
Differentiating Flock Worker's Lung from other Diseases
- Silicosis
- Asbestosis
- Berylliosis
- Industrial printing chemicals (e.g. carbon black, ink mist)
- Hypersensitivity pneumonitis
- Coal Workers Pneumoconiosis
Epidemiology and Demographics
- Cases have been reported in the United States, Canada, Turkey, and Spain.[6]
- In a study flocking workers when compared to controls, whereas age, sex, tobacco use and working years were not found to be significantly associated with respiratory symptoms. [5]
Risk Factors
- Flock worker’s lung is seen in textile workers chronically exposed to short nylon fibers typically flocked onto textile products.[7]Flock is produced by guillotine cutting or rotary cutting. Rotary cutting has been claimed to be more hazardous than guillotine cutting .[5]
- Working in production and maintenance, on a flocking range, and more days and hours per week; cleaning with compressed air; and a higher current and cumulative respirable dust exposure were found to be strongly associated with symptoms of the disease.[1]
- Multivariate analyses showed that being a polypropylene flocking worker was a predictive factor for impairment of pulmonary function.
- A study showed that the risk of respiratory symptoms increased 3.6 fold in polypropylene flocking workers when compared to controls.[5]
Natural History, Complications and Prognosis
The natural history of FWL includes the following patterns
- complete resolution of symptoms;
- radiographic and pulmonary function abnormalities;
- permanent, but stable symptoms and restrictive pulmonary function deficits;
- and progressive decline in pulmonary function, causing death from respiratory failure and secondary pulmonary hypertension. A low baseline diffusing capacity of the lung for carbon monoxide is associated with the persistence and progression of FWL [8]
- In general, recovery occurred over a period of months or years after steroid treatment and leaving the place of work, with some having persistent dyspnoea, exercise limitation, or requirements for chronic supplemental oxygen.[9]
- There was also threefold increase in lung cancer incidence. [10]
Diagnosis
Diagnostic Criteria
A case of flock-worker's lung is defined as
- a histologic diagnosis of nonspecific interstitial pneumonia characterized by bronchiolocentric nodular and diffuse interstitial lymphoid infiltrates and nonuniform alveolar filling by macrophages, with or without interstitial fibrosis;
- Other histologic manifestations of Interstitial Lung Disease (ILD) not attributable to another disease; or
- In the absence of a tissue specimen, a grossly abnormal distribution of cell types on bronchoalveolar lavage (BAL) with restrictive lung function and HRCT findings of either diffuse ground glass opacity or micronodularity.[11]
History and Symptoms
- The nylon flock exposed workers mostly commonly presented with chronic respiratory symptoms over several years, but subacute presentations also occurred. For example, in a Canadian outbreak, 5 of 88 exposed workers developed disease after exposure occurring over several days
- Restrictive ventilatory defects are most common, but obstructive defects have been reported. [12]
A study showed 20 individual from different geographic locations having FWL shared symptoms of
- dyspnea and cough, with and without sputum production.
- These symptoms were present for months to years before clinical presentation, which, for some cases, seemed precipitated by an acute exacerbation in the preceding few days. Symptom onsets for the patients occurred over a 15-yr period, with no apparent concentration of onsets for any plant location.
- Few nonrespiratory symptoms were noted. Weight loss was noted in two patients and two workers had arthralgias or myalgias. Eight of the 20 patients were noted to have asthma, increased bronchial responsiveness to methacholine, or increased bronchodilator responsiveness.[2]
Physical Examination
- Physical examination in one study showed that both patients with FWL and control groups were evaluated as normal.[5]
- Others have reported
- inspiratory crackles on auscultation [9]
- Pulmonary function test results revealing a restrictive pattern [4]
Laboratory Findings
- There are no specific laboratory findings associated with FWL.
Imaging Findings
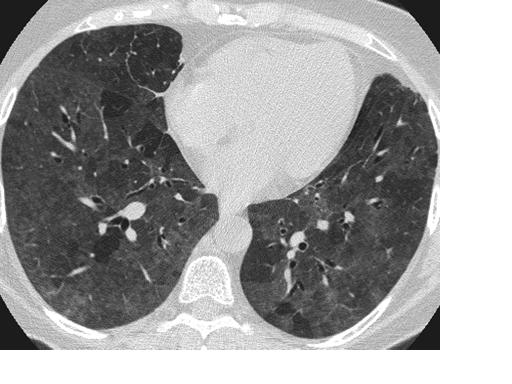
- High-resolution CT scan remained a highly sensitive diagnostic test. Pulmonary function tests and plain chest radiograph were less sensitive.[13]
- The most common findings in FWL on CT scan were ground-glass opacities and micronodules, with a peripheral predominance in some.[14]
Other Diagnostic Studies
- Transbronchial biopsy may prove helpful in the consideration of alternate diagnoses, but wedge biopsy by thoracotomy or thoracoscopy is necessary to adequately examine the characteristic lesion of this interstitial lung disease in relation to the pulmonary lobular architecture. [4]
Treatment
Medical Therapy
- Cessation of nylon exposure and corticosteroid therapy, for exacerbation of respiratory problems, has been observed to lead symptomatic improvement but over all lung functions are still seen to decline in certain cases.[7][9]
Prevention
- several observations affirmed that the exposure preceded the disease and that the disease improved with exposure cessation to the implicated work environments.[1]
- NIOSH has made recommendations to companies that manufacture flock and make flock containing products that aim to reduce workers’ exposure to flock dust. These include: engineering controls and alternative methods to cleaning the workplace with compressed air, which re-aerosolizes settled dust, improved cutter maintenance, and implementation of medical surveillance programs have reduced the number of reported cases.[3][12]
References
- ↑ 1.0 1.1 1.2 1.3 Kreiss K (June 2013). "Occupational lung disease: from case reports to prevention". Chest. 143 (6): 1529–1531. doi:10.1378/chest.12-3001. PMC 3673658. PMID 23732577.
- ↑ 2.0 2.1 2.2 Eschenbacher WL, Kreiss K, Lougheed MD, Pransky GS, Day B, Castellan RM (June 1999). "Nylon flock-associated interstitial lung disease". Am. J. Respir. Crit. Care Med. 159 (6): 2003–8. doi:10.1164/ajrccm.159.6.9808002. PMID 10351952.
- ↑ 3.0 3.1 "CDC - NIOSH Program Portfolio : Respiratory Diseases : Risks".
- ↑ 4.0 4.1 4.2 Eschenbacher, William L.; Kreiss, Kathleen; Lougheed, M. Diane; Pransky, Glenn S.; Day, Brian; Castellan, Robert M. (1999). "Nylon Flock–Associated Interstitial Lung Disease". American Journal of Respiratory and Critical Care Medicine. 159 (6): 2003–2008. doi:10.1164/ajrccm.159.6.9808002. ISSN 1073-449X.
- ↑ 5.0 5.1 5.2 5.3 5.4 Atis, S. (2005). "The respiratory effects of occupational polypropylene flock exposure". European Respiratory Journal. 25 (1): 110–117. doi:10.1183/09031936.04.00138403. ISSN 0903-1936.
- ↑ "Flock worker's lung - Wikipedia".
- ↑ 7.0 7.1 "Chronic Hypersensitivity Pneumonitis Associated with Inhaled Exposure to Nylon Powder for 3-D Printing: A Variant of Nylon Flock Worker's Lung Disease? | D46. CASE REPORTS IN ENVIRONMENTAL AND OCCUPATIONAL HEALTH".
- ↑ Turcotte, Scott E.; Chee, Alex; Walsh, Ronald; Grant, F. Curry; Liss, Gary M.; Boag, Alexander; Forkert, Lutz; Munt, Peter W.; Lougheed, M. Diane (2013). "Flock Worker's Lung Disease". Chest. 143 (6): 1642–1648. doi:10.1378/chest.12-0920. ISSN 0012-3692.
- ↑ 9.0 9.1 9.2 Barroso, E.; Ibañez, M.D.; Aranda, F.I.; Romero, S. (2002). "Polyethylene flock-associated interstitial lung disease in a Spanish female". European Respiratory Journal. 20 (6): 1610–1612. doi:10.1183/09031936.02.00030102. ISSN 0903-1936.
- ↑ Kern, David G.; Kern, Eli; Crausman, Robert S.; Clapp, Richard W. (2011). "A Retrospective Cohort Study of Lung Cancer Incidence in Nylon Flock Workers, 1998–2008". International Journal of Occupational and Environmental Health. 17 (4): 345–351. doi:10.1179/oeh.2011.17.4.345. ISSN 1077-3525.
- ↑ "Chronic Interstitial Lung Disease in Nylon Flocking Industry Workers -- Rhode Island, 1992-1996".
- ↑ 12.0 12.1 Sauler, Maor; Gulati, Mridu (2012). "Newly Recognized Occupational and Environmental Causes of Chronic Terminal Airways and Parenchymal Lung Disease". Clinics in Chest Medicine. 33 (4): 667–680. doi:10.1016/j.ccm.2012.09.002. ISSN 0272-5231.
- ↑ Kern, David G.; Kuhn, Charles; Ely, E. Wesley; Pransky, Glenn S.; Mello, Curtis J.; Fraire, Armando E.; Müller, Joachim (2000). "Flock Worker's Lung". Chest. 117 (1): 251–259. doi:10.1378/chest.117.1.251. ISSN 0012-3692.
- ↑ Weiland, David A.; Lynch, David A.; Jensen, Steven P.; Newell, John D.; Miller, David E.; Crausman, Robert S.; Kuhn, Charles; Kern, David G. (2003). "Thin-Section CT Findings in Flock Worker's Lung, a Work-related Interstitial Lung Disease". Radiology. 227 (1): 222–231. doi:10.1148/radiol.2271011063. ISSN 0033-8419.