Epidural abscess MRI
|
Epidural abscess Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Epidural abscess MRI On the Web |
|
American Roentgen Ray Society Images of Epidural abscess MRI |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: João André Alves Silva, M.D. [2]; Anthony Gallo, B.S. [3]
Overview
MRI
MRI is the preferred imaging study in the diagnosis of epidural abscess. MRI is considered to be as effective as myelography in the diagnosis of epidural abscess, however MRI is superior, particularly in emergency situations, as it allows for visualization of the spinal cord in all planes without having to move the patient, who might have a neurological injury.[1] Epidural abscess appears as a lentiform or crescent-shaped fluid collection. On T2-weighted images, epidural abscesses appear hyperintense compared to the cerebrospinal fluid. On T1-weighted images, epidural abscesses appear isointense or hypointense when compared to the brain. After administration of gadolinium contrast, the dura mater is enhanced on T1-weighted images.[2]
Intracranial Epidural Abscess
MRI is the preferred imaging method to investigate intracranial epidural abscess because it has higher accuracy defining intracranial lesions, compared to CT scan.
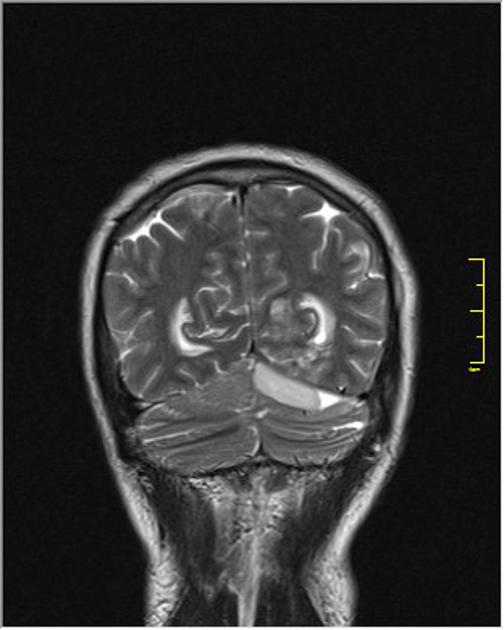
Image courtesy of Radiopaedia [4]
Spinal Epidural Abscess
The MRI with gadolinium contrast is the preferred method to help in the diagnosis of spinal epidural abscess since it's not an invasive test and helps to delineate longitudinally and the paraspinal extension of the abscess, hence helping to plan surgical approach. It is also helpful to differentiate an abscess from malignancy. [1][3]
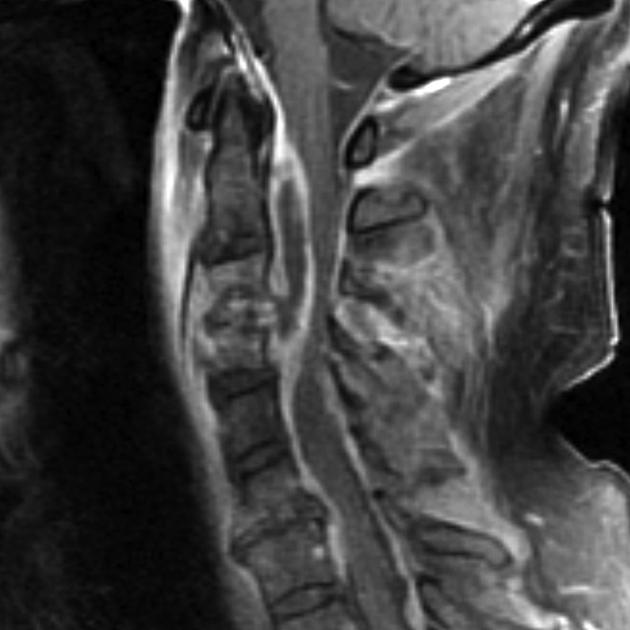
Image courtesy of Dr Frank Gaillard [5]
References
- ↑ 1.0 1.1 Grewal, S. (2006). "Epidural abscesses". British Journal of Anaesthesia. 96 (3): 292–302. doi:10.1093/bja/ael006. ISSN 0007-0912.
- ↑ Longo, Dan L. (Dan Louis) (2012). Harrison's principles of internal medici. New York: McGraw-Hill. ISBN 978-0-07-174889-6.
- ↑ Darouiche, Rabih O. (2006). "Spinal Epidural Abscess". New England Journal of Medicine. 355 (19): 2012–2020. doi:10.1056/NEJMra055111. ISSN 0028-4793.