Epidural abscess MRI: Difference between revisions
Joao Silva (talk | contribs) |
Joao Silva (talk | contribs) |
||
| Line 20: | Line 20: | ||
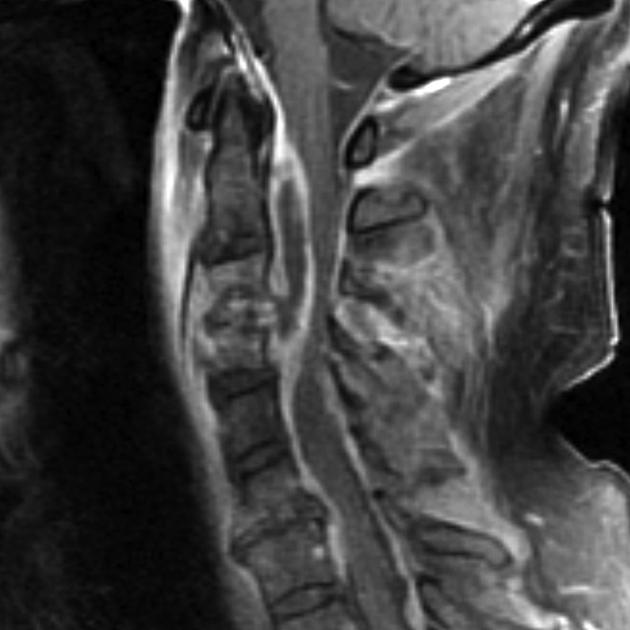
[[Image: | [[Image:Spinal epidural abscess(MRI).jpg|thumb|center|Spinal Epidural Abscess accompanied by C3/C4 level discitis osteomyelitis]] | ||
==References== | ==References== | ||
Revision as of 03:28, 31 March 2014
|
Epidural abscess Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Epidural abscess MRI On the Web |
|
American Roentgen Ray Society Images of Epidural abscess MRI |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: João André Alves Silva, M.D. [2]
Overview
An epidural abscess is a rare suppurative infection of the central nervous system, a collection of pus localised in the epidural space, lying outside the dura mater, which accounts for less than 2% of focal CNS infections. [1] It may occur in two different places: intracranially or in the spinal canal. Because the initial symptoms and clinical characteristics are not always identical, and are similar to the ones in other diseases, along with the fact that they are both rare conditions, the final diagnosis might be delayed in time. This late diagnosis comes at great cost to the patient, since it is usually accompanied by a bad prognosis and severe complications with a potential fatal outcome. The diagnosis of epidural abscess should be first suspected from the clinical findings, being posteriorly supported by laboratory tests and imaging studies, however it can only be confirmed after surgical drainage and proper study of the collected material. According to the location of the collection, the abscess may have different origins, different organisms involved, symptoms, evolutions, complications and therapeutical techniques. [2][3]
MRI
The MRI is the preferred imaging study to help in the diagnosis of epidural abscess, mainly because:
- it shows the infection early in its course
- provides accurate location of the lesion
- good report of the evolution of the inflammatory changes
It is considered to be as effective as the myelography in the diagnosis of epidural abscess, however it is superior to that one, particularly in emergency situations when it allows the physicians to examine the spinal cord in all planes, without having to move the patient, who might have a neurological injury. This way we avoid a possible worsening of the condition. [4] The epidural abscess appears as a lentiform or crescent-shaped fluid collection, which on T2-weighted images appears as an hyperintense image compared to the CSF. On T1-weighted images, when compared to the brain tissue the fluid collection may show as isointense or hypointense. After administration of gadolinium contrast, the dura mater is enhanced on T1-weighted images. [5]
Intracranial Epidural Abscess
The MRI is the preferred image method to investigate epidural abscess since it has higher accuracy defining intracranial lesions, when compared to the CT scan. However, it is less effective for the evaluation of bone erosions than this last one.
Spinal Epidural Abscess
The MRI with gadolinium contrast is the preferred method to help in the diagnosis of spinal epidural abscess since it's not an invasive test and helps to delineate longitudinally and the paraspinal extension of the abscess, hence helping to plan surgical approach. It is also helpful to differentiate an abscess from malignancy. [4][3]
References
- ↑ Longo, Dan L. (Dan Louis) (2012). Harrison's principles of internal medici. New York: McGraw-Hill. ISBN 978-0-07-174889-6.
- ↑ Danner, R. L.; Hartman, B. J. (1987). "Update of Spinal Epidural Abscess: 35 Cases and Review of the Literature". Clinical Infectious Diseases. 9 (2): 265–274. doi:10.1093/clinids/9.2.265. ISSN 1058-4838.
- ↑ 3.0 3.1 Darouiche, Rabih O. (2006). "Spinal Epidural Abscess". New England Journal of Medicine. 355 (19): 2012–2020. doi:10.1056/NEJMra055111. ISSN 0028-4793.
- ↑ 4.0 4.1 Grewal, S. (2006). "Epidural abscesses". British Journal of Anaesthesia. 96 (3): 292–302. doi:10.1093/bja/ael006. ISSN 0007-0912.
- ↑ Longo, Dan L. (Dan Louis) (2012). Harrison's principles of internal medici. New York: McGraw-Hill. ISBN 978-0-07-174889-6.