Ductal carcinoma
| Ductal carcinoma | |
 | |
|---|---|
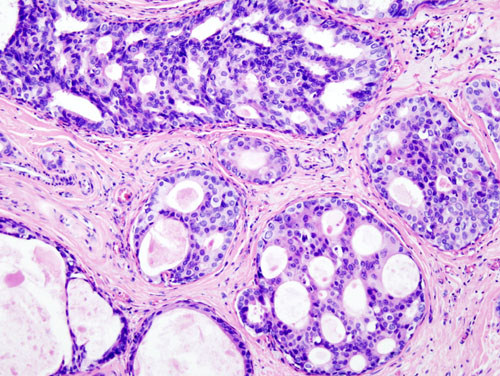
| Histopathologic image from ductal cell carcinoma in situ (DCIS) of breast. Hematoxylin-eosin stain. | |
| ICD-10 | C50, D05 |
| ICD-9 | 174-175, 233.0 |
| ICD-O: | 8500 |
| MeSH | D018270 |
|
WikiDoc Resources for Ductal carcinoma |
|
Articles |
|---|
|
Most recent articles on Ductal carcinoma Most cited articles on Ductal carcinoma |
|
Media |
|
Powerpoint slides on Ductal carcinoma |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Ductal carcinoma at Clinical Trials.gov Trial results on Ductal carcinoma Clinical Trials on Ductal carcinoma at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Ductal carcinoma NICE Guidance on Ductal carcinoma
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Ductal carcinoma Discussion groups on Ductal carcinoma Patient Handouts on Ductal carcinoma Directions to Hospitals Treating Ductal carcinoma Risk calculators and risk factors for Ductal carcinoma
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Ductal carcinoma |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [1] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Ductal carcinoma is the most common type of breast cancer in women. It comes in two forms: infiltrating ductal carcinoma (IDC), an invasive, malignant abnormal proliferation of cells in tissue known as neoplasm, and ductal carcinoma in situ (DCIS), a noninvasive neoplasm.
Intraductal carcinoma
Intraductal carcinoma of the breast (Ductal Carcinoma In Situ, DCIS) is the most common type of noninvasive breast cancer in women. Ductal carcinoma refers to the development of cancer cells within the milk ducts of the breast. In situ means "in place" and refers to the fact that the cancer has not moved out of the duct and into any surrounding tissue.
As screening mammography has become more widespread, DCIS has become one of the most commonly diagnosed breast conditions. It is often referred to as "stage zero breast cancer." In countries where screening mammography is uncommon, DCIS is sometimes diagnosed at a later stage, but in countries where screening mammography is widespread, it is usually diagnosed on a mammogram when it is so small that it has not formed a lump. DCIS is not painful or dangerous, and it does not metastasize unless it first develops into invasive cancer.
DCIS is usually discovered through a mammogram as very small specks of calcium known as microcalcifications. However, not all microcalcifications indicate the presence of DCIS, which must be confirmed by biopsy. DCIS may be multifocal, and treatment is aimed at excising all of the abnormal duct elements, leaving "clear margins", an area of much debate. After excision treatment often includes local radiation therapy. With appropriate treatment, DCIS is unlikely to develop into invasive cancer. Surgical excision with radiation lowers the risk that the DCIS will recur or that invasive breast cancer will develop.
Treatment options for DCIS
DCIS patients have two surgery strategy choices. They are lumpectomy (most commonly followed by radiation therapy) or mastectomy.
Lumpectomy is surgery that removes only the cancer and a rim of normal breast tissue around it. For women with only one area of cancer in their breast, and a tumor under 4 centimeters that was removed with clear margins, lumpectomy followed by radiation is often equivalent to mastectomy for mortality related to their cancer, albeit at the higher risk of local disease recurrence on the breast/chest wall. The addition of radiation therapy to lumpectomy in DCIS reduces the risk of local recurrence by about 58% as compared to excision alone. Lumpectomy with radiation is estimated to carry between a 12-19% chance at 15 years for local recurrence of breast cancer (approximately a 0.5% to 1.0% risk per year), which would require a "salvage mastectomy". Patients with family history of breast cancer and those presenting with breast cancer who are less than 40 years old face higher risks of local recurrence with breast conservation techniques. Extensive DCIS of high grade, large size, and resected with minimal surgical margins, even with radiotherapy, results in recurrence rates of at least 50% and would be better served with a mastectomy procedure.
Mastectomy may also be the preferred treatment in certain instances:
- Two or more tumors exist in different areas of the breast (a "multifocal" cancer).
- Failure to achieve adequate margins on attempted lumpectomy.
- The breast has previously received radiation (XRT) treatment.
- The tumor is large relative to the size of the breast.
- The patient has had scleroderma or another disease of the connective tissue, which can complicate XRT treatment.
- The patient lives in an area where XRT is inaccessible
- The patient is apprehensive about their risk of local recurrence
- The patient is less than 40 or has a strong family history of breast cancer
The system for analysing the suitability of DCIS patients for the options of breast conservation without radiation, breast conservation with radiation, or mastectomy is called the VanNuys Prognostic Scoring Index (VNPI). This VNPI analyzes DCIS features in terms of size, grade, surgical margins, and patient age and assigns "scores" to favourable features.
Tamoxifen or another hormonal therapy is recommended for some women with DCIS to help prevent breast cancer. Hormonal therapy further decreases the risk of recurrence of DCIS or the development of invasive breast cancer. However, they have potentially dangerous side effects, such as increased risk of endometrial cancer, severe circulatory problems, or stroke. In addition, hot flashes, vaginal dryness, abnormal vaginal bleeding, and a possibility of premature menopause are common for women who were not yet menopausal when they started treatment.
Unlike women with invasive breast cancer, women with DCIS do not undergo chemotherapy and have traditionally not been advised to have their lymph nodes tested or removed. Some institutional series reporting significant rates of recurrent invasive cancers after mastectomy for DCIS, have recently endorsed routine sentinal node biopsy (SNB) in these patients. [1], while other have concluded it be reserved for selected patients. Most agree that SNB should be considered with tissue diagnosis of high risk DCIS (grade III with palpable mass or larger size on imaging) as well as in patients undergoing mastectomy after a core or excisional biopsy diagnosis of DCIS. [2] [3] Experts are not sure whether all women with DCIS would eventually develop invasive breast cancer if they live for a long time and are not treated.
Invasive Ductal Carcinoma
Invasive Ductal Carcinoma (IDC) is the most common form of invasive breast cancer. It accounts for 80% of all types of breast cancer. On a mammography, it is usually visualized as a mass with fine spikes radiating from the edges. On physical examination, this lump usually feels much harder or firmer than benign breast lesions. On microscopic examination, the cancerous cells invade and replace the surrounding normal tissues. IDC is divided in several histological subtypes.
Prognosis for IDC
The prognosis of IDC depends, in part, on its histological subtype. Mucinous, papillary, cribriform, and tubular carcinomas have longer survival, and lower recurrence rates. The prognosis of the most common form of IDC, called "IDC Not Otherwise Specified", is intermediate. Finally, some rare forms of breast cancer (e.g. sarcomatoid carcinoma, inflammatory carcinoma) have a poor prognosis.
Regardless of the histological subtype, the prognosis of IDC depends also on its staging, histological grade, expression of hormone receptors and of oncogenes like HER2/neu.
Treatment options for IDC
Treatment of IDC usually starts with surgery to remove the main tumor mass and to sample the lymph nodes in the axilla. The stage of the tumor is ascertained after this first surgery. Adjuvant therapy (i.e. treatment after surgery) usually includes chemotherapy, radiotherapy, hormonal therapy (e.g. Tamoxifen) and targeted therapy (e.g. Trastuzumab). More surgery is occasionally needed to complete the removal of the initial tumor or to remove recurrences.
The treatment options offered to a given patient are determined by the form, stage and location of the cancer, and also by the age, history of prior disease and general health of the patient. Not all patients are treated the same way.
References
- ↑ Tan JC, McCready DR, Easson AM, Leong WL. Role of Sentinel Lymph Node Biopsy in Ductal Carcinoma-in-situ Treated by Mastectomy. Ann Surg Oncol. 2007 Feb;14(2):638-45.[PMID 17103256]
- ↑ van Deurzen CH, et al. Is there an indication for sentinel node biopsy in patients with ductal carcinoma in situ of the breast? A review. Eur J Cancer. 2007 Feb 12. [PMID 17300928]
- ↑ Yen TW, et al. Predictors of invasive breast cancer in patients with an initial diagnosis of ductal carcinoma in situ: a guide to selective use of sentinel lymph node biopsy in management of ductal carcinoma in situ. J Am Coll Surg. 2005 Apr;200(4):516-26. [PMID 15804465]
- Original text on IDC from Infiltrating Ductal Carcinoma, licensed under the GNU Free Documentation License.
|
Breast Cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Ductal carcinoma On the Web |
|
American Roentgen Ray Society Images of Ductal carcinoma |