Daptomycin adverse reactions
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Abdurahman Khalil, M.D. [2]
The following adverse reactions are described, or described in greater detail, in other sections:
-Anaphylaxis/hypersensitivity reactions
-Myopathy and rhabdomyolysis
-Eosinophilic pneumonia
-Peripheral neuropathy
-Increased International Normalized Ratio (INR)/prolonged prothrombin time
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Clinical Trials Experience
Clinical trials enrolled 1,864 patients treated with CUBICIN and 1,416 treated with comparator.
Complicated Skin and Skin Structure Infection Trials
In Phase 3 complicated skin and skin structure infection (cSSSI) trials, CUBICIN was discontinued in 15/534 (2.8%) patients due to an adverse reaction, while comparator was discontinued in 17/558 (3.0%) patients.
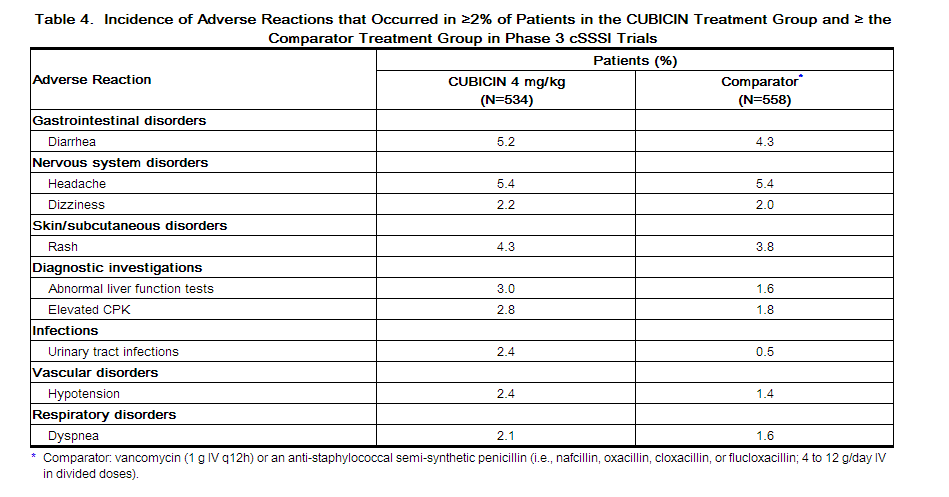
The rates of the most common adverse reactions, organized by body system, observed in cSSSI (4 mg/kg CUBICIN) patients are displayed in Table 4
Drug-related adverse reactions (possibly or probably drug-related) that occurred in <1% of patients receiving CUBICIN in the cSSSI trials are as follows:
Body as a Whole: fatigue, weakness, rigors, flushing, hypersensitivity
Blood/Lymphatic System: leukocytosis, thrombocytopenia, thrombocytosis, eosinophilia, increased International Normalized Ratio (INR)
Cardiovascular System: supraventricular arrhythmia
Dermatologic System: eczema
Digestive System: abdominal distension, stomatitis, jaundice, increased serum lactate dehydrogenase
Metabolic/Nutritional System: hypomagnesemia, increased serum bicarbonate, electrolyte disturbance
Musculoskeletal System: myalgia, muscle cramps, muscle weakness, arthralgia
Nervous System: vertigo, mental status change, paresthesia
Special Senses: taste disturbance, eye irritation
S. aureus Bacteremia/Endocarditis Trial
In the S. aureus bacteremia/endocarditis trial, CUBICIN was discontinued in 20/120 (16.7%) patients due to an adverse reaction, while comparator was discontinued in 21/116 (18.1%) patients.
Serious Gram-negative infections (including bloodstream infections) were reported in 10/120 (8.3%) CUBICIN-treated patients and 0/115 comparator-treated patients. Comparator-treated patients received dual therapy that included initial gentamicin for 4 days. Infections were reported during treatment and during early and late follow-up. Gram-negative infections included cholangitis, alcoholic pancreatitis, sternal osteomyelitis/mediastinitis, bowel infarction, recurrent Crohn's disease, recurrent line sepsis, and recurrent urosepsis caused by a number of different Gram-negative bacteria.
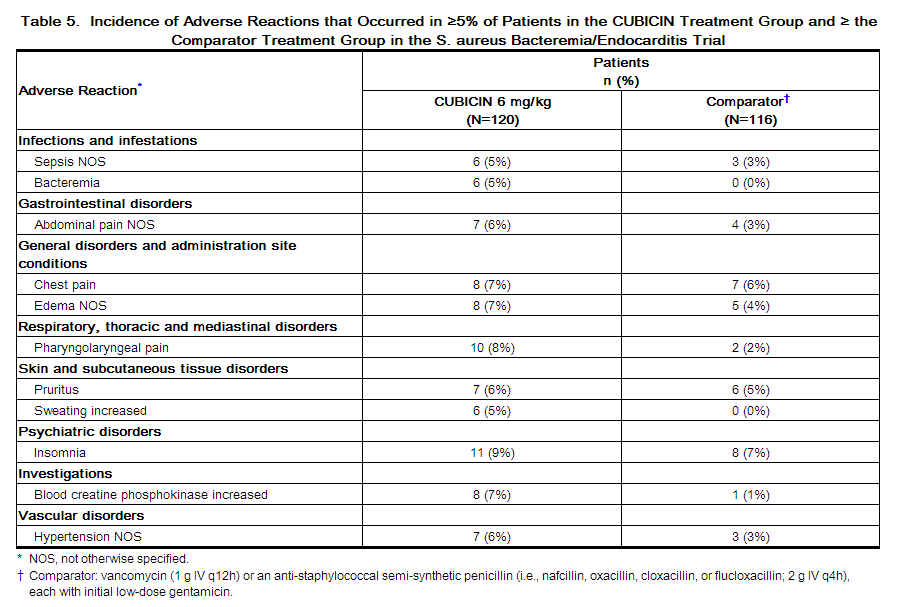
The rates of the most common adverse reactions, organized by System Organ Class (SOC), observed in S. aureus bacteremia/endocarditis (6 mg/kg CUBICIN) patients are displayed in Table 5.
The following reactions, not included above, were reported as possibly or probably drug-related in the CUBICIN-treated group:
Blood and Lymphatic System Disorders: eosinophilia, lymphadenopathy, thrombocythemia, thrombocytopenia
Cardiac Disorders: atrial fibrillation, atrial flutter, cardiac arrest
Ear and Labyrinth Disorders: tinnitus
Eye Disorders: vision blurred
Gastrointestinal Disorders: dry mouth, epigastric discomfort, gingival pain, hypoesthesia oral
Infections and Infestations: candidal infection NOS, vaginal candidiasis, fungemia, oral candidiasis, urinary tract infection fungal
Investigations: blood phosphorous increased, blood alkaline phosphatase increased, INR increased, liver function test abnormal, alanine aminotransferase increased, aspartate aminotransferase increased, prothrombin time prolonged
Metabolism and Nutrition Disorders: appetite decreased NOS
Musculoskeletal and Connective Tissue Disorders: myalgia
Nervous System Disorders: dyskinesia, paresthesia
Psychiatric Disorders: hallucination NOS
Renal and Urinary Disorders: proteinuria, renal impairment NOS
Skin and Subcutaneous Tissue Disorders: pruritus generalized, rash vesicular
Other Trials
In Phase 3 trials of community-acquired pneumonia (CAP), the death rate and rates of serious cardiorespiratory adverse events were higher in CUBICIN-treated patients than in comparator-treated patients. These differences were due to lack of therapeutic effectiveness of CUBICIN in the treatment of CAP in patients experiencing these adverse events [see Indications and Usage ].
Laboratory Changes
Complicated Skin and Skin Structure Infection Trials
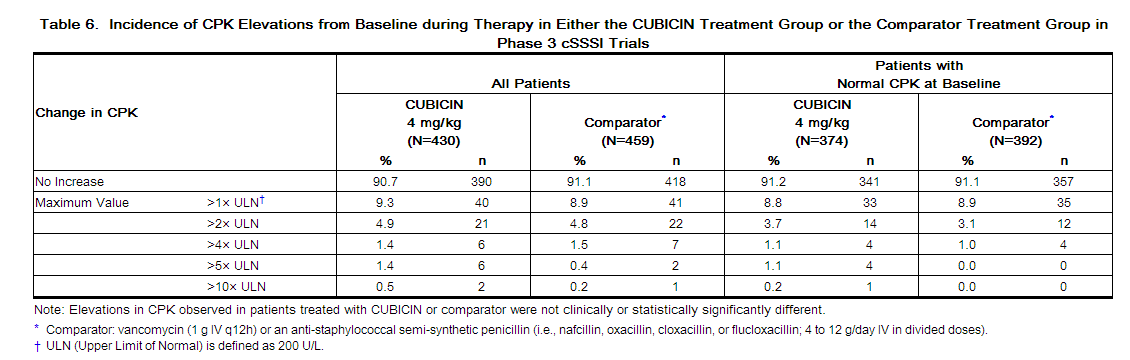
In Phase 3 cSSSI trials of CUBICIN at a dose of 4 mg/kg, elevations in CPK were reported as clinical adverse events in 15/534 (2.8%) CUBICIN-treated patients, compared with 10/558 (1.8%) comparator-treated patients. Of the 534 patients treated with CUBICIN, 1 (0.2%) had symptoms of muscle pain or weakness associated with CPK elevations to greater than 4 times the upper limit of normal (ULN). The symptoms resolved within 3 days and CPK returned to normal within 7 to 10 days after treatment was discontinued [see Warnings and Precautions ]. Table 6 summarizes the CPK shifts from Baseline through End of Therapy in the cSSSI trials.
S. aureus Bacteremia/Endocarditis Trial
In the S. aureus bacteremia/endocarditis trial, at a dose of 6 mg/kg, 11/120 (9.2%) CUBICIN-treated patients, including two patients with baseline CPK levels >500 U/L, had CPK elevations to levels >500 U/L, compared with 1/116 (0.9%) comparator-treated patients. Of the 11 CUBICIN-treated patients, 4 had prior or concomitant treatment with an HMG-CoA reductase inhibitor. Three of these 11 CUBICIN-treated patients discontinued therapy due to CPK elevation, while the one comparator-treated patient did not discontinue therapy [see Warnings and Precautions].
Post-Marketing Experience
The following adverse reactions have been identified during postapproval use of CUBICIN. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to estimate their frequency reliably or establish a causal relationship to drug exposure.
Immune System Disorders: anaphylaxis; hypersensitivity reactions, including angioedema, drug rash with eosinophilia and systemic symptoms (DRESS), pruritus, hives, shortness of breath, difficulty swallowing, truncal erythema, and pulmonary eosinophilia [see Contraindications , Warnings and Precautions ]
Infections and Infestations: Clostridium difficile–associated diarrhea [see Warnings and Precautions (5.5)]
Musculoskeletal Disorders: myoglobin increased; rhabdomyolysis (some reports involved patients treated concurrently with CUBICIN and HMG-CoA reductase inhibitors) [see Warnings and Precautions , Drug Interactions , and Clinical Pharmacology ]
Respiratory, Thoracic, and Mediastinal Disorders: cough, eosinophilic pneumonia [see Warnings and Precautions ]
Nervous System Disorders: peripheral neuropathy [see Warnings and Precautions ]
Skin and Subcutaneous Tissue Disorders: serious skin reactions, including Stevens-Johnson syndrome and vesiculobullous rash (with or without mucous membrane involvement)
Gastrointestinal Disorders: nausea, vomiting
References
http://www.accessdata.fda.gov/drugsatfda_docs/label/2010/021572s033lbl.pdf