Cryptococcosis pathophysiology
|
Cryptococcosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Cryptococcosis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Cryptococcosis pathophysiology |
|
Risk calculators and risk factors for Cryptococcosis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Serge Korjian M.D.; Yazan Daaboul, M.D.
Overview
Pathophysiology
- Infective cryptococcal species are ubiquitous and natural exposure is very common.
- Infection occurs by inhalation of aerosolized, dessicated basidiospores.
- Once these spores reach the alveoli, they are phagocytosed by the alveolar macrophages without prior opsonization (usually required for yeast forms).
- Cryptococci are intracellular pathogens. Once they are phagocytosed, they germinate and multiply within the macrophages.
- Activated macrophages are capable of destroying the yeast forms that develop; however, non-activated macrophages act as germination centers for cryptococci.
- Cryptococci have the ability of forming giant cells that resist phagocytosis and have been hypothesized to play a role in latent infections and reactivation.
- Cryptococci also have the ability of changing the number of sets of chromosomes during infection, this has been associated with heteroresistance to certain antifungal agents.
- After exposure to desiccated yeast cells or spores, patients may clear infection or contain it within granulomata as a latent infection, or it may disseminate depending on host immune status or other less well understood mechanisms.
- Disseminated disease occurs among patients with compromised cell-mediated immunity.
- The immune response to cryptococcal infection is highly dependent on host T-cell function, and interferon-γ and TNF-α signaling.
- Granuloma formation can also be seen and may also be responsible for reactivation in patients with immunocompromised states.[1][2]
Microscopic Pathology
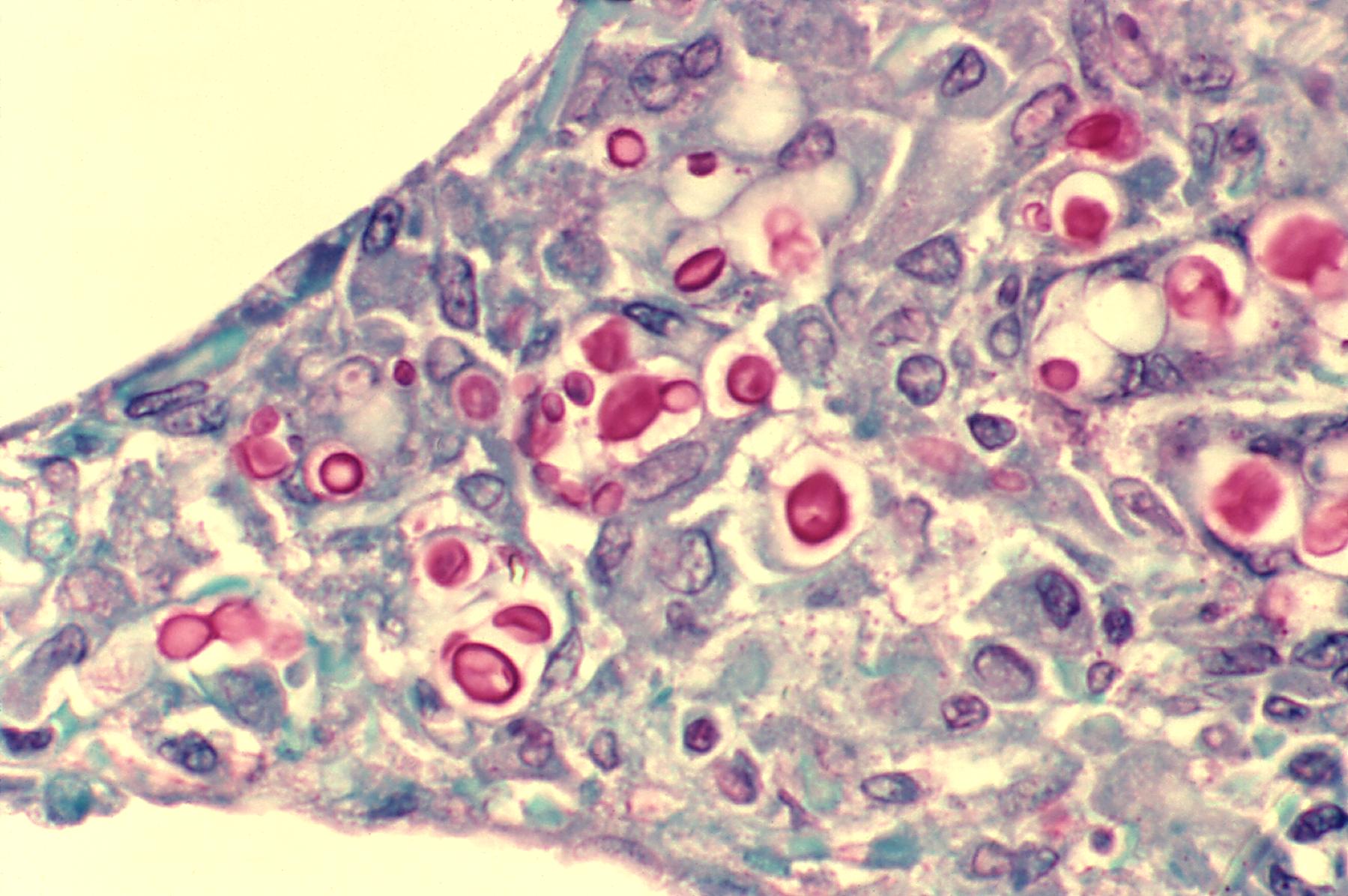
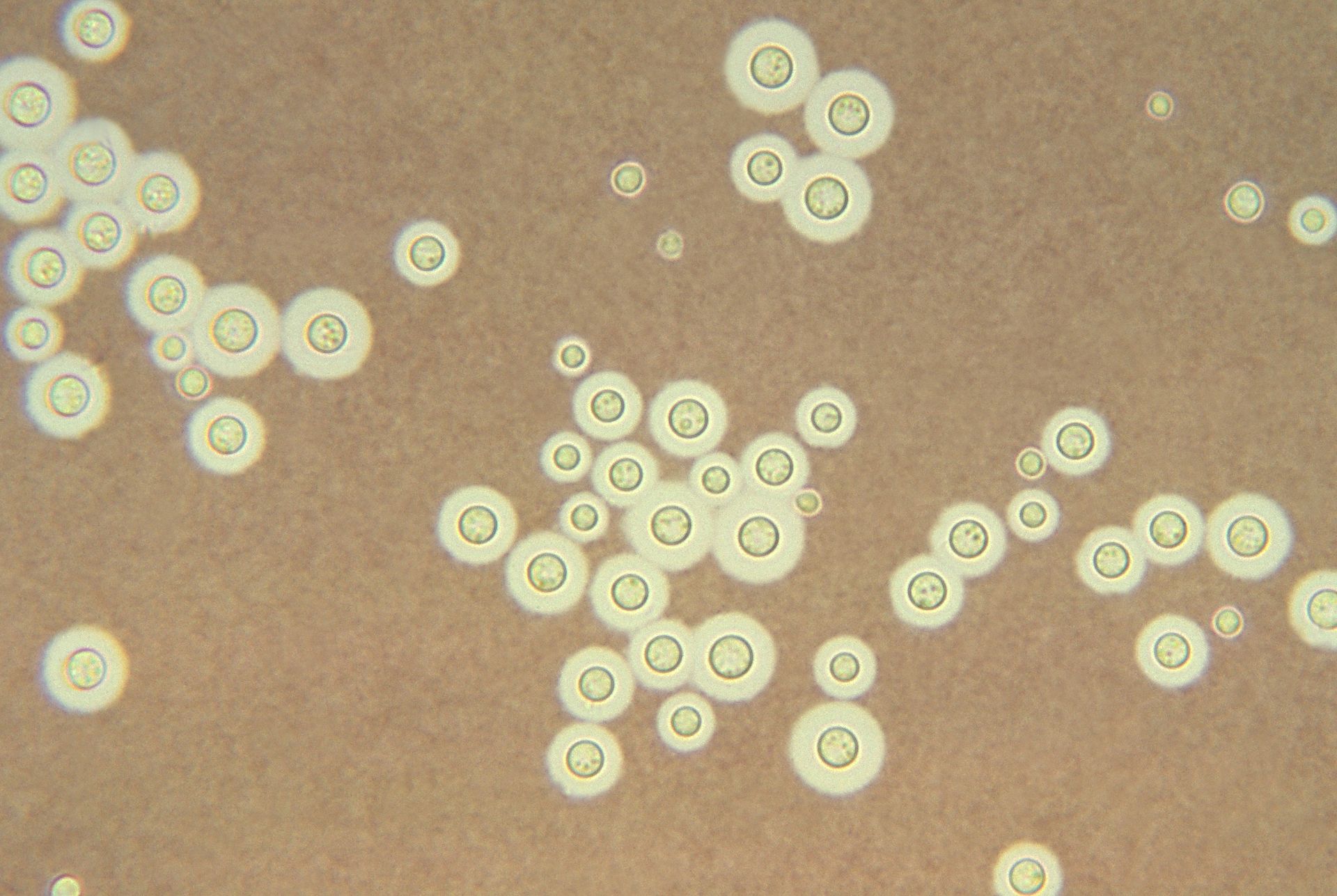
- Cryptococcus exists in yeast form.
- It is round/ovoid and approximately 5-15 μm (resembles Histoplasma or Candida, but often larger).
- It is characterized by a thick mucopolysaccharde capsule with a refractile center.
- India ink staining is used for easy visualization of the capsule in cerebrospinal fluid.[3]
- It has a tear drop-shaped budding pattern which is useful in differentiating Cryptococcus from Blastomyces and Histoplasma.
- Cryptococcal infections are usually accompanied by very little inflammation.
- Cryptococcus stain positive with methenamine silver, Alcian blue, and PAS (may be confused with corpora amylacea in the CNS).[4]
Multimedia
Cryptococcosis (PAS stain)
{{#ev:youtube|ZG0AcmtBLe4}}
References
- ↑ Brizendine KD, Baddley JW, Pappas PG (2011). "Pulmonary cryptococcosis". Semin Respir Crit Care Med. 32 (6): 727–34. doi:10.1055/s-0031-1295720. PMID 22167400.
- ↑ May RC, Stone NR, Wiesner DL, Bicanic T, Nielsen K (2015). "Cryptococcus: from environmental saprophyte to global pathogen". Nat Rev Microbiol. doi:10.1038/nrmicro.2015.6. PMID 26685750.
- ↑ Zerpa R, Huicho L, Guillén A (1996). "Modified India ink preparation for Cryptococcus neoformans in cerebrospinal fluid specimens". J Clin Microbiol. 34 (9): 2290–1. PMC 229234. PMID 8862601.
- ↑ Fungi. Libre Pathology (2015). http://librepathology.org/wiki/index.php/Fungi#Cryptococcosis. Accessed on December 31, 2015.