Crohn's disease pathophysiology: Difference between revisions
Usama Talib (talk | contribs) No edit summary |
m (Bot: Removing from Primary care) |
||
| (14 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
<div style="-webkit-user-select: none;"> | |||
{| class="infobox" style="position: fixed; top: 65%; right: 10px; margin: 0 0 0 0; border: 0; float: right;" | |||
|- | |||
| {{#ev:youtube|https://https://www.youtube.com/watch?v=thzOJV-CHRo|350}} | |||
|- | |||
|} | |||
__NOTOC__ | __NOTOC__ | ||
{{Crohn's disease}} | {{Crohn's disease}} | ||
{{CMG}} ; {{AE}} {{ADG}} | {{CMG}}; {{AE}} {{ADG}} | ||
==Overview== | ==Overview== | ||
[[Genetic]] and environmental factors play a key role in the pathogenesis of Crohn's disease. [[Mutation]]s in the [[NOD2|CARD15]] gene (also known as the NOD2 [[gene]]) are associated with Crohn's disease and with susceptibility to certain phenotypes of disease location and activity. Environmental factors include autoimmune Disease and dysregulated Immune Response to Commensal Bacteria. Characteristic features of the [[pathology]] that point toward Crohn's disease are transmural pattern of [[inflammation]] and skip lesions. Under microscopy [[Granuloma]]s are seen, which are aggregates of [[macrophage]] derivatives known as giant cells, are found in 50% of cases and are most specific for Crohn's disease. | [[Genetic]] and environmental factors play a key role in the pathogenesis of Crohn's disease. [[Mutation]]s in the [[NOD2|CARD15]] gene (also known as the NOD2 [[gene]]) are associated with Crohn's disease and with susceptibility to certain phenotypes of disease location and activity. Environmental factors include autoimmune Disease and dysregulated Immune Response to Commensal Bacteria. Characteristic features of the [[pathology]] that point toward Crohn's disease are transmural pattern of [[inflammation]] and skip lesions. Under microscopy [[Granuloma]]s are seen, which are aggregates of [[macrophage]] derivatives known as giant cells, are found in 50% of cases and are most specific for Crohn's disease. | ||
==Pathophysiology== | ==Pathophysiology== | ||
The exact pathogenesis of Crohn's disease is not clearly understood. However, 4 components have been proved to play a key role in the pathogenesis of Crohn's disease. | |||
=== | *Genetic component | ||
*Stress and environmental component | |||
-->{{cite journal | author = Cuthbert A, Fisher S, Mirza M, ''et al.'' | title = The contribution of NOD2 gene mutations to the risk and site of disease in inflammatory bowel disease. | journal = Gastroenterology | volume = 122 | issue = 4 | pages = 867-74 | year = 2002 | id = PMID 11910337}}</ref | *Microbial component | ||
*Inflammatory component | |||
===Genetic Component=== | |||
There are several genes involved in the pathogenesis of Crohn's disease. Mutation of any of these genes disrupts the normal function of cells triggering an inflammatory response. Some common and most important genes are as follows:.<ref><!-- | |||
*The most recent gene to be implicated in Crohn's disease is [[ATG16L1]], which may reduce the effectiveness of [[autophagy]], and hinder the body's ability to attack invasive bacteria | -->{{cite journal | author = Cuthbert A, Fisher S, Mirza M, ''et al.'' | title = The contribution of NOD2 gene mutations to the risk and site of disease in inflammatory bowel disease. | journal = Gastroenterology | volume = 122 | issue = 4 | pages = 867-74 | year = 2002 | id = PMID 11910337}}</ref><ref>Ogura Y, Bonen DK, Inohara N, ''et al.'' A frameshift mutation in NOD2 associated with susceptibility to Crohn's disease. ''Nature''. 2001 May 31;411(6837):603-6.</ref><ref>Prescott NJ, Fisher SA, Franke A, Hampe J, Onnie CM, Soars D, Bagnall R, Mirza MM, Sanderson J, Forbes A, Mansfield JC, Lewis CM, Schreiber S, Mathew CG. A nonsynonymous SNP in ATG16L1 predisposes to ileal Crohn's disease and is independent of CARD15 and IBD5. ''Gastroenterology.'' 2007 May;132(5):1665-71. PMID: 17484864.</ref><ref>Cobrin GM, Abreu MT. Defects in mucosal immunity leading to Crohn's disease. ''Immunol Rev.'' 2005 Aug;206:277-95. PMID 16048555</ref> | ||
=== | *NOD2/CARD15 gene | ||
*OCTN1 gene | |||
* | *DLG5 gene | ||
* | *TLR4 gene | ||
==== | <u>'''The following tables summarizes the most important genes involved in the pathogenesis of Crohn's disease'''</u> | ||
* | {| class="wikitable" | ||
* | !Genes | ||
* | ! colspan="2" |Chromosome | ||
!Function | |||
* | !Mutation | ||
* | |- | ||
* | |NOD2/CARD15 | ||
* | |16 | ||
|16q12.1 | |||
|Encodes a scaffolding protein important for maintaining epithelial integrity | |||
|Disrupts normal epithelial integrity | |||
|- | |||
|OCTN1 | |||
|05 | |||
|5q31 | |||
|Ecodes an ion channel | |||
|Alters the function of cation transporters and cell-to-cell signaling | |||
|- | |||
|DLG5 | |||
|10 | |||
|10q22.3 | |||
|Interact additively with the NOD2/CARD15 gene | |||
|Iincrease susceptibility to CD along with CARD15 | |||
|- | |||
|TLR4 | |||
|09 | |||
|9q33.1 | |||
|Lipopolysaccharide signaling, bacterial recognition, and subsequent immune response | |||
|Altered immune response to pathogens and a subsequent increase in inflammation. | |||
|} | |||
* The most recent gene to be implicated in Crohn's disease is [[ATG16L1]], which may reduce the effectiveness of [[autophagy]], and hinder the body's ability to attack invasive bacteria | |||
===Stress and Environmental Component=== | |||
*Stress signals are perceived by the central nervous system (CNS), triggering the hypothalamic-pituitary-adrenal axis and the sympathetic-adrenal-medullary axis. | |||
*Neuroendocrine mediators released in response to stress not only modulate secretory, absorptive, and barrier functions in the gut but also increase the gut permeability. | |||
*Stress increases gut permeability along with other factors which inlude | |||
**Corticotropin-releasing factor | |||
**Autonomic nervous system | |||
**Enteric nervous system | |||
===Microbial Component=== | |||
The possible mechanisms for a bacterial etiology in the development of CD include: | |||
*Initial immune response to a specific pathogen resulting in intestinal infection | |||
*Alterations in normal bacterial flora of the intestinal tract | |||
*Defective mucosal barrier and overwhelming exposure to resident bacteria and their antigens and endotoxins | |||
*Alterations to the intestinal immune response | |||
{| border="1" cellpadding="5" cellspacing="0" align="center" |class="wikitable" | |||
! style="background:#efefef;" |Infectious Pathogens Implicated in Crohn’s Disease | |||
|- | |||
| | |||
*Escherichia coli<br> | |||
*Listeria monocytogenes<br> | |||
*Yersinia enterocolitica<br> | |||
*Mycobacterium avium subspecies paratuberculosis<br> | |||
*Measles virus | |||
|} | |||
=== Immune Component === | |||
*'''<u>Altered immune response</u>''': | |||
** An abnormal antibody response to an unspecified bacterial antigen is mainly responsible for inflammation in Crohn's disease. | |||
** The inflammatory response is believed to be triggered when elimination of specified microbial antigen was unsuccessful leading to altered immune response | |||
** Dysregulation of normal mucosal immune response results in failure of phagocytosis leading to antigen persistence. | |||
** Antigen persistance leads to antibodies production against all the normal gut flora. | |||
** Activation resulted in secretion of tumor necrosis factor-alpha (TNF-alpha) and subsequent epithelial changes. | |||
*'''<u>Cytokine response</u>''': | |||
**The primary precipitating event in Crohn's disease is T-cell mediated immune response. | |||
**Activated T cells are responsible for the release of cytokines. | |||
**The production of inflammatory cytokines results in ulceration and increased intestinal permeability. | |||
**The characteristic granulomatous lesion seen in Crohn’s disease is evidence of a cell-mediated immune response. | |||
**The early lesions of Crohn's disease are characterized by elevations in interleukin-4 (IL-4) and decrease in IFN-gamma, a pattern more consistent with an overactive Th2 immune response. | |||
**Chronic lesions are associated with high levels of interleukin-2 (IL-2), interferon gamma (IFN-gamma), TNF-alpha, and interleukin-12 and -18 (IL-12 and IL-18) consistent with an Th1 immune response. | |||
**Tumor necrosis factor appears to play a significant role in the pathogenesis of CD. | |||
***TNF-alpha induces expression of adhesion factors that allow for inflammatory cells to infiltrate and activates macrophages to promote release of other pro-inflammatory mediators such as IFN-gamma. | |||
***Neutralization of TNF resulted in significant decrease in inflammation. | |||
***TNF-alpha concentrations in the stool can be used to monitor disease activity in both CD and UC. | |||
===Gross Pathology=== | ===Gross Pathology=== | ||
Characteristic features of | Characteristic features of Crohn's disease on gross pathology include: | ||
* | * Creeping fat | ||
* | * Thick/rubbery intestinal wall | ||
* | * [[Strictures]] (string sign on barium enema) | ||
* Skip areas | |||
* [[Aphthous ulcers|Aphthous mucosal ulcers]] | |||
===Microscopic Pathology=== | ===Microscopic Pathology=== | ||
On microscopic analysis of the affected colon may show [[mucosa]]l inflammation. Histo-pathological finding include | |||
*Transmural [[inflammation]] | *Transmural [[inflammation]] | ||
*[[Granuloma]]s | *Lymphoid aggregates throughout the wall of the colon. | ||
* | *Focal infiltration of [[neutrophils]] along with [[lymphocyte|mononuclear cells]], may infiltrate into the [[Crypts of Lieberkühn|crypts]] leading to inflammation (crypititis) or abscess (crypt abscess). | ||
*Non- caseating [[Granuloma]]s (aggregates of [[macrophage]] derivatives) known as giant cells, are found in 50% of cases and are most specific for Crohn's disease. | |||
* | *Blunting of the intestinal [[villus|villi]] | ||
*Atypical branching of the crypts | |||
*''Paneth cell metaplasia'' <ref name="Robbins">Crawford JM. "The Gastrointestinal tract, Chapter 17". In Cotran RS, Kumar V, Robbins SL. ''Robbins Pathologic Basis of Disease: 5th Edition''. W.B. Saunders and Company, Philadelphia, 1994.</ref> | |||
[[Image:Crohn's transmural path. | [[Image:Crohn's transmural path 1.png|thumb|center|400px|H and E section of [[colectomy]] showing transmural inflammation.<br>Source:By The original uploader was Samir at English Wikipedia [GFDL (http://www.gnu.org/copyleft/fdl.html) or CC-BY-SA-3.0 (http://creativecommons.org/licenses/by-sa/3.0/)], via Wikimedia Commons]] | ||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
{{WH}} | |||
{{WS}} | |||
[[Category:Disease]] | [[Category:Disease]] | ||
[[Category:Autoimmune diseases]] | [[Category:Autoimmune diseases]] | ||
| Line 53: | Line 134: | ||
[[Category:Conditions diagnosed by stool test]] | [[Category:Conditions diagnosed by stool test]] | ||
[[Category:Abdominal pain]] | [[Category:Abdominal pain]] | ||
[[Category:Needs overview]] | [[Category:Needs overview]] | ||
Latest revision as of 21:10, 29 July 2020
| https://https://www.youtube.com/watch?v=thzOJV-CHRo%7C350}} |
|
Crohn's disease |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Crohn's disease pathophysiology On the Web |
|
American Roentgen Ray Society Images of Crohn's disease pathophysiology |
|
Risk calculators and risk factors for Crohn's disease pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Aditya Ganti M.B.B.S. [2]
Overview
Genetic and environmental factors play a key role in the pathogenesis of Crohn's disease. Mutations in the CARD15 gene (also known as the NOD2 gene) are associated with Crohn's disease and with susceptibility to certain phenotypes of disease location and activity. Environmental factors include autoimmune Disease and dysregulated Immune Response to Commensal Bacteria. Characteristic features of the pathology that point toward Crohn's disease are transmural pattern of inflammation and skip lesions. Under microscopy Granulomas are seen, which are aggregates of macrophage derivatives known as giant cells, are found in 50% of cases and are most specific for Crohn's disease.
Pathophysiology
The exact pathogenesis of Crohn's disease is not clearly understood. However, 4 components have been proved to play a key role in the pathogenesis of Crohn's disease.
- Genetic component
- Stress and environmental component
- Microbial component
- Inflammatory component
Genetic Component
There are several genes involved in the pathogenesis of Crohn's disease. Mutation of any of these genes disrupts the normal function of cells triggering an inflammatory response. Some common and most important genes are as follows:.[1][2][3][4]
- NOD2/CARD15 gene
- OCTN1 gene
- DLG5 gene
- TLR4 gene
The following tables summarizes the most important genes involved in the pathogenesis of Crohn's disease
| Genes | Chromosome | Function | Mutation | |
|---|---|---|---|---|
| NOD2/CARD15 | 16 | 16q12.1 | Encodes a scaffolding protein important for maintaining epithelial integrity | Disrupts normal epithelial integrity |
| OCTN1 | 05 | 5q31 | Ecodes an ion channel | Alters the function of cation transporters and cell-to-cell signaling |
| DLG5 | 10 | 10q22.3 | Interact additively with the NOD2/CARD15 gene | Iincrease susceptibility to CD along with CARD15 |
| TLR4 | 09 | 9q33.1 | Lipopolysaccharide signaling, bacterial recognition, and subsequent immune response | Altered immune response to pathogens and a subsequent increase in inflammation. |
- The most recent gene to be implicated in Crohn's disease is ATG16L1, which may reduce the effectiveness of autophagy, and hinder the body's ability to attack invasive bacteria
Stress and Environmental Component
- Stress signals are perceived by the central nervous system (CNS), triggering the hypothalamic-pituitary-adrenal axis and the sympathetic-adrenal-medullary axis.
- Neuroendocrine mediators released in response to stress not only modulate secretory, absorptive, and barrier functions in the gut but also increase the gut permeability.
- Stress increases gut permeability along with other factors which inlude
- Corticotropin-releasing factor
- Autonomic nervous system
- Enteric nervous system
Microbial Component
The possible mechanisms for a bacterial etiology in the development of CD include:
- Initial immune response to a specific pathogen resulting in intestinal infection
- Alterations in normal bacterial flora of the intestinal tract
- Defective mucosal barrier and overwhelming exposure to resident bacteria and their antigens and endotoxins
- Alterations to the intestinal immune response
| Infectious Pathogens Implicated in Crohn’s Disease |
|---|
|
Immune Component
- Altered immune response:
- An abnormal antibody response to an unspecified bacterial antigen is mainly responsible for inflammation in Crohn's disease.
- The inflammatory response is believed to be triggered when elimination of specified microbial antigen was unsuccessful leading to altered immune response
- Dysregulation of normal mucosal immune response results in failure of phagocytosis leading to antigen persistence.
- Antigen persistance leads to antibodies production against all the normal gut flora.
- Activation resulted in secretion of tumor necrosis factor-alpha (TNF-alpha) and subsequent epithelial changes.
- Cytokine response:
- The primary precipitating event in Crohn's disease is T-cell mediated immune response.
- Activated T cells are responsible for the release of cytokines.
- The production of inflammatory cytokines results in ulceration and increased intestinal permeability.
- The characteristic granulomatous lesion seen in Crohn’s disease is evidence of a cell-mediated immune response.
- The early lesions of Crohn's disease are characterized by elevations in interleukin-4 (IL-4) and decrease in IFN-gamma, a pattern more consistent with an overactive Th2 immune response.
- Chronic lesions are associated with high levels of interleukin-2 (IL-2), interferon gamma (IFN-gamma), TNF-alpha, and interleukin-12 and -18 (IL-12 and IL-18) consistent with an Th1 immune response.
- Tumor necrosis factor appears to play a significant role in the pathogenesis of CD.
- TNF-alpha induces expression of adhesion factors that allow for inflammatory cells to infiltrate and activates macrophages to promote release of other pro-inflammatory mediators such as IFN-gamma.
- Neutralization of TNF resulted in significant decrease in inflammation.
- TNF-alpha concentrations in the stool can be used to monitor disease activity in both CD and UC.
Gross Pathology
Characteristic features of Crohn's disease on gross pathology include:
- Creeping fat
- Thick/rubbery intestinal wall
- Strictures (string sign on barium enema)
- Skip areas
- Aphthous mucosal ulcers
Microscopic Pathology
On microscopic analysis of the affected colon may show mucosal inflammation. Histo-pathological finding include
- Transmural inflammation
- Lymphoid aggregates throughout the wall of the colon.
- Focal infiltration of neutrophils along with mononuclear cells, may infiltrate into the crypts leading to inflammation (crypititis) or abscess (crypt abscess).
- Non- caseating Granulomas (aggregates of macrophage derivatives) known as giant cells, are found in 50% of cases and are most specific for Crohn's disease.
- Blunting of the intestinal villi
- Atypical branching of the crypts
- Paneth cell metaplasia [5]
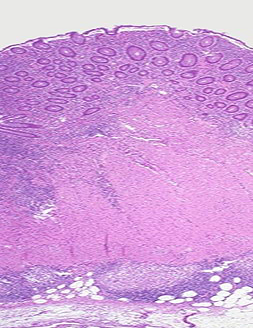
Source:By The original uploader was Samir at English Wikipedia [GFDL (http://www.gnu.org/copyleft/fdl.html) or CC-BY-SA-3.0 (http://creativecommons.org/licenses/by-sa/3.0/)], via Wikimedia Commons
References
- ↑ Cuthbert A, Fisher S, Mirza M; et al. (2002). "The contribution of NOD2 gene mutations to the risk and site of disease in inflammatory bowel disease". Gastroenterology. 122 (4): 867–74. PMID 11910337.
- ↑ Ogura Y, Bonen DK, Inohara N, et al. A frameshift mutation in NOD2 associated with susceptibility to Crohn's disease. Nature. 2001 May 31;411(6837):603-6.
- ↑ Prescott NJ, Fisher SA, Franke A, Hampe J, Onnie CM, Soars D, Bagnall R, Mirza MM, Sanderson J, Forbes A, Mansfield JC, Lewis CM, Schreiber S, Mathew CG. A nonsynonymous SNP in ATG16L1 predisposes to ileal Crohn's disease and is independent of CARD15 and IBD5. Gastroenterology. 2007 May;132(5):1665-71. PMID: 17484864.
- ↑ Cobrin GM, Abreu MT. Defects in mucosal immunity leading to Crohn's disease. Immunol Rev. 2005 Aug;206:277-95. PMID 16048555
- ↑ Crawford JM. "The Gastrointestinal tract, Chapter 17". In Cotran RS, Kumar V, Robbins SL. Robbins Pathologic Basis of Disease: 5th Edition. W.B. Saunders and Company, Philadelphia, 1994.