Congenital adrenal hyperplasia overview: Difference between revisions
No edit summary |
No edit summary |
||
| Line 2: | Line 2: | ||
{{Congenital adrenal hyperplasia}} | {{Congenital adrenal hyperplasia}} | ||
{{CMG}}; | {{CMG}}; {{AE}}{{MJ}} | ||
==Overview== | ==Overview== | ||
Congenital adrenal hyperplasia (CAH) refers to any of several autosomal recessive conditions resulting from biochemical paths of the steroidogenesis of cortisol from cholesterol by the adrenal glands. Most of these conditions involve greater or lesser production of sex steroids and can alter development of primary or secondary sex characteristics in affected infants, children, and adults. Only a small minority of people with CAH can be said to have an intersex condition, but this attracted American public attention in the late 1990s and many accounts of varying accuracy have appeared in the popular media. Approximately 95% of cases of CAH are due to 21-hydroxylase deficiency. | |||
Most of these conditions involve greater or lesser production of | Prenatal diagnosis can be made in both of these disorders by chorionic villous sampling, but this can only be done at 8-10 weeks. In order to prevent the deleterious effect of excess androgens on genital (and brain!) development, therapy must be started earlier. This is most often considered if there is an affected sibling. Treatment is dexamethasone, which is not degraded by the placenta, but is associated with significant maternal weight gain, hypertension, and edema. | ||
==Pathophisiology== | |||
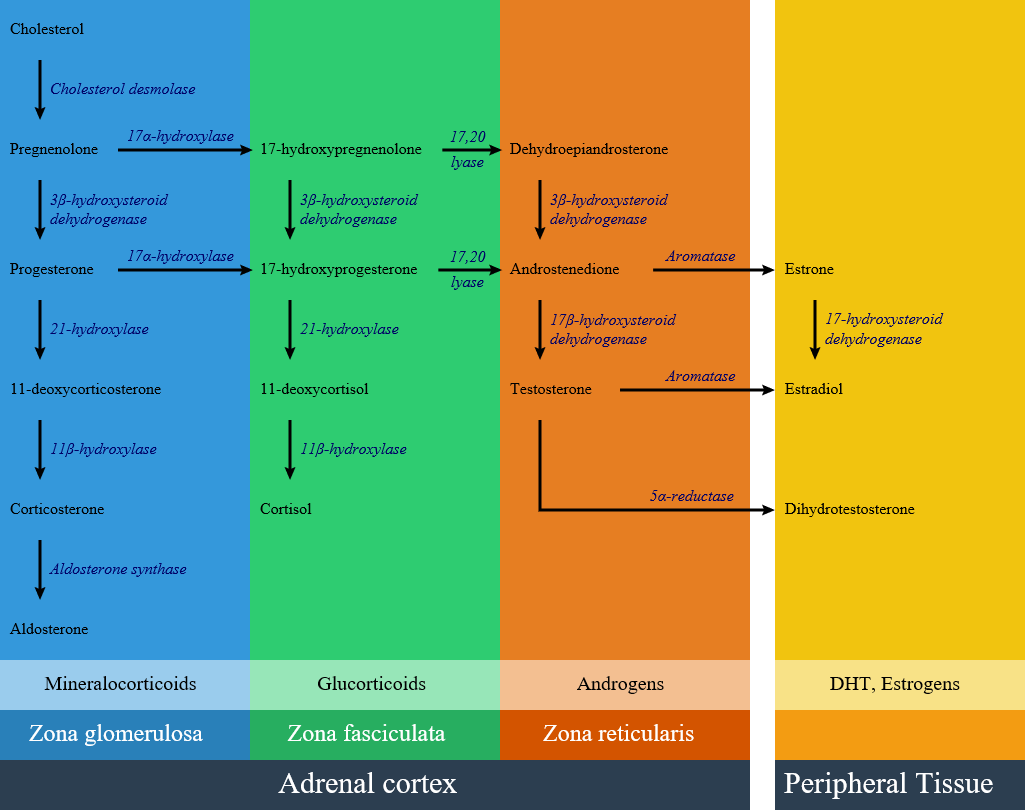
[[image:Adrenal Steroids.png|600px]] | |||
==Classification== | |||
Congenital adrenal hyperplasia is classified into seven types based on the genetic causes that lead to hyperplasia and hormonal imbalance. | |||
{| align="center" class="wikitable" style="border: 0px; font-size: 90%; margin: 3px;" | |||
! align="center" style="background:#DCDCDC;" rowspan="2" colspan="2" |Disease | |||
! align="center" style="background:#DCDCDC;" colspan="2" |History and symptoms | |||
! align="center" style="background:#DCDCDC;" colspan="2" |Laboratory findings | |||
! align="center" style="background:#DCDCDC;" |Defective gene | |||
|- | |||
!Blood pressure | |||
!Genitalia | |||
! | |||
!K levels | |||
! | |||
|- | |||
| align="center" style="padding: 5px 5px; background: #DCDCDC;" rowspan="2" |[[21-hydroxylase deficiency]] | |||
|Classic type | |||
| | |||
* Low in salt-wasting | |||
* Normal in non-salt-wasting | |||
| | |||
* Female: ambiguous | |||
* Male: normal or scrotal pigmentation and large phallus | |||
| | |||
Increased: | |||
* 17-OHP | |||
* Progesterone | |||
* Androstenedione | |||
* DHEA | |||
Decreased: | |||
* Aldosterone | |||
* Corticosterone (salt-wasting) | |||
* Cortisol (simple virilizing) | |||
| | |||
* High in salt wasting type | |||
* Normal in non salt wasting | |||
| | |||
* CYP21A1 and CYP21A2 gene | |||
|- | |||
|Non-classic type | |||
| | |||
* Normal | |||
| | |||
* Female: virilization after puberty | |||
* Male: normal appearance | |||
|Increased: | |||
* 17-OHP | |||
* Exaggerated androstene-dione, DHEA, and 17-OHP | |||
response to ACTH | |||
| | |||
* Normal | |||
| | |||
* CYP21A1 and CYP21A2 gene | |||
|- | |||
| align="center" style="padding: 5px 5px; background: #DCDCDC;" colspan="2" |17a-Hydroxylase deficiency | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
* Hypertension | |||
| | |||
* Female: normal | |||
* Male: ambiguous | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
* Increased DOC, corticosterone | |||
* Decreased 17OH-steroids, cortisol, aldosterone, androgens and estrogens | |||
| | |||
* Low | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
* ''CYP17A1'' | |||
|- | |||
| align="center" style="padding: 5px 5px; background: #DCDCDC;" colspan="2" |11β-hydroxylase deficiency | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
* Hypertension | |||
| | |||
* Female: ambiguous | |||
* Male: normal or scrotal pigmentation and large phallus | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
* Indreased DOC, 11-deoxycortisol | |||
* Decreased corticosterone, cortisol, aldosterone, androgens | |||
| | |||
* Low | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
* ''CYP11B1'' | |||
|- | |||
| align="center" style="padding: 5px 5px; background: #DCDCDC;" colspan="2" |3-beta-hydroxysteroid dehydrogenase | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
| | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" |Increased: | |||
* DHEA | |||
* 17-OH pregneno-lone | |||
* Pregnenolone | |||
Decreased: | |||
* Cortisol | |||
* Aldosterone | |||
| | |||
* High | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
|- | |||
| align="center" style="padding: 5px 5px; background: #DCDCDC;" colspan="2" |Cytochrome P450-oxidoreductase (POR) deficiency (ORD) | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
| | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
| | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
|- | |||
| align="center" style="padding: 5px 5px; background: #DCDCDC;" colspan="2" |Congenital lipoid adrenal hyperplasia | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
| | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
| | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
|- | |||
| align="center" style="padding: 5px 5px; background: #DCDCDC;" colspan="2" |Cholesterol side-chain cleavage enzyme deficiency | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
| | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
| | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
|} | |||
==Diagnosis== | |||
==Prevention== | |||
==References== | |||
{{ | {{reflist|2}} | ||
Revision as of 15:31, 26 July 2017
|
Congenital adrenal hyperplasia main page |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mehrian Jafarizade, M.D [2]
Overview
Congenital adrenal hyperplasia (CAH) refers to any of several autosomal recessive conditions resulting from biochemical paths of the steroidogenesis of cortisol from cholesterol by the adrenal glands. Most of these conditions involve greater or lesser production of sex steroids and can alter development of primary or secondary sex characteristics in affected infants, children, and adults. Only a small minority of people with CAH can be said to have an intersex condition, but this attracted American public attention in the late 1990s and many accounts of varying accuracy have appeared in the popular media. Approximately 95% of cases of CAH are due to 21-hydroxylase deficiency. Prenatal diagnosis can be made in both of these disorders by chorionic villous sampling, but this can only be done at 8-10 weeks. In order to prevent the deleterious effect of excess androgens on genital (and brain!) development, therapy must be started earlier. This is most often considered if there is an affected sibling. Treatment is dexamethasone, which is not degraded by the placenta, but is associated with significant maternal weight gain, hypertension, and edema.
Pathophisiology
Classification
Congenital adrenal hyperplasia is classified into seven types based on the genetic causes that lead to hyperplasia and hormonal imbalance.
| Disease | History and symptoms | Laboratory findings | Defective gene | |||
|---|---|---|---|---|---|---|
| Blood pressure | Genitalia | K levels | ||||
| 21-hydroxylase deficiency | Classic type |
|
|
Increased:
Decreased:
|
|
|
| Non-classic type |
|
|
Increased:
response to ACTH |
|
| |
| 17a-Hydroxylase deficiency |
|
|
|
|
| |
| 11β-hydroxylase deficiency |
|
|
|
|
| |
| 3-beta-hydroxysteroid dehydrogenase | Increased:
Decreased:
|
|
||||
| Cytochrome P450-oxidoreductase (POR) deficiency (ORD) | ||||||
| Congenital lipoid adrenal hyperplasia | ||||||
| Cholesterol side-chain cleavage enzyme deficiency | ||||||