Congenital adrenal hyperplasia Overview
|
Congenital adrenal hyperplasia main page |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mehrian Jafarizade, M.D [2]
Synonyms and keywords: Congenital adrenal hyperplasia, CAH, Adrenal hyperplasia
Overview
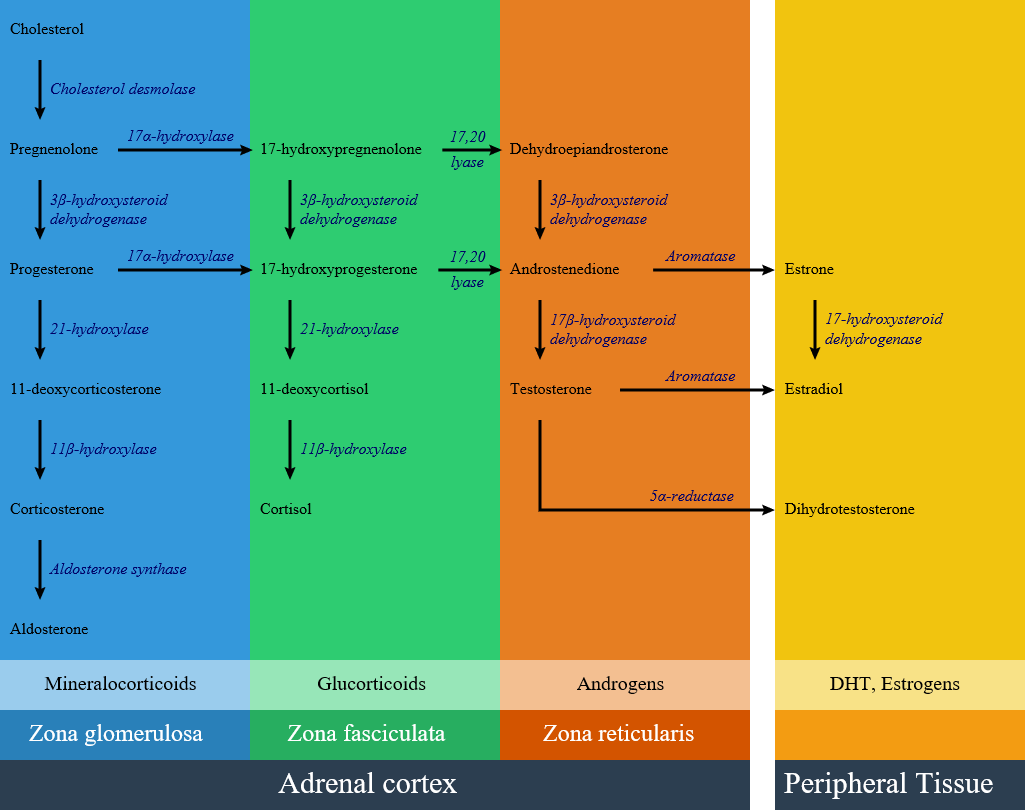
Congenital adrenal hyperplasia (CAH) refers to any of several autosomal recessive conditions resulting from biochemical paths of the steroidogenesis of cortisol from cholesterol by the adrenal glands. Most of these conditions involve greater or lesser production of sex steroids and can alter development of primary or secondary sex characteristics in affected infants, children, and adults. Only a small minority of people with CAH can be said to have an intersex condition, but this attracted American public attention in the late 1990s and many accounts of varying accuracy have appeared in the popular media. Approximately 95% of cases of CAH are due to 21-hydroxylase deficiency. Prenatal diagnosis can be made in both of these disorders by chorionic villous sampling, but this can only be done at 8-10 weeks. In order to prevent the deleterious effect of excess androgens on genital (and brain!) development, therapy must be started earlier. This is most often considered if there is an affected sibling. Treatment is dexamethasone, which is not degraded by the placenta, but is associated with significant maternal weight gain, hypertension, and edema.
Pathophisiology
Classification
Congenital adrenal hyperplasia is classified into seven types based on the genetic causes that lead to hyperplasia and hormonal imbalance.
| Disease | History and symptoms | Laboratory findings | Defective gene | |||
|---|---|---|---|---|---|---|
| Blood pressure | Genitalia | K levels | ||||
| 21-hydroxylase deficiency | Classic type |
|
|
Increased:
Decreased:
|
|
|
| Non-classic type |
|
|
Increased:
response to ACTH |
|
| |
| 17a-Hydroxylase deficiency |
|
|
|
|
| |
| 11β-hydroxylase deficiency |
|
|
|
|
| |
| 3-beta-hydroxysteroid dehydrogenase | Increased:
Decreased:
|
|
||||
| Cytochrome P450-oxidoreductase (POR) deficiency (ORD) | ||||||
| Congenital lipoid adrenal hyperplasia | ||||||
| Cholesterol side-chain cleavage enzyme deficiency | ||||||