Colorectal cancer screening: Difference between revisions
(Mahshid) |
|||
| Line 6: | Line 6: | ||
==Overview== | ==Overview== | ||
Current guidelines recommend that colonoscopy is the optimal screening tool for colon cancer since it detects 98-99% of the cases. | Current guidelines recommend that [[colonoscopy]] is the optimal screening tool for colon cancer since it detects 98-99% of the cases. High risk individuals include a first-degree relative with colorectal cancer. A [[colonoscopy]] every 10 years reduces the risk of left-sided colon cancer. Right sided colon cancers are more likely to be missed because they are harder to reach and they could be flat, which means they would be harder to detect. Flat growths (non-polypoid) are difficult to detect and are more likely to progress to colon cancer compared to cylindrical [[polyps]]. | ||
==Colorectal Cancer Screening== | ==Colorectal Cancer Screening== | ||
| Line 12: | Line 12: | ||
Colorectal cancer may take several years to develop. If colorectal cancer is detected early, the chances of a cure is greatly improved. The patient population can be divided into average, moderate, and high risk. | Colorectal cancer may take several years to develop. If colorectal cancer is detected early, the chances of a cure is greatly improved. The patient population can be divided into average, moderate, and high risk. | ||
The | The algorithm below demonstrates a screening protocol for '''average risk''' patients.<ref>https://www.rmf.harvard.edu/~/media/Files/_Global/KC/PDFs/RMFCRC.pdf</ref> | ||
[[Image:Average risk CRC.jpg| | <figure-inline>[[Image:Average risk CRC.jpg|800x800px]]</figure-inline> | ||
The | The algorithm below demonstrates a screening protocol for '''moderate risk''' patients.<ref>https://www.rmf.harvard.edu/~/media/Files/_Global/KC/PDFs/RMFCRC.pdf</ref> | ||
[[Image:Moderate risk CRC.jpg| | <figure-inline>[[Image:Moderate risk CRC.jpg|800x800px]]</figure-inline> | ||
The | The algorithm below demonstrates a screening protocol for '''high risk''' patients.<ref>https://www.rmf.harvard.edu/~/media/Files/_Global/KC/PDFs/RMFCRC.pdf</ref> | ||
[[Image:High risk CRC.jpg| | <figure-inline>[[Image:High risk CRC.jpg|800x800px]]</figure-inline> | ||
The most common indicator of high risk is a first-degree relative with colorectal cancer a personal history of inflammatory bowel disease<ref name="Lieberman2009">{{cite journal|last1=Lieberman|first1=David A.|title=Screening for Colorectal Cancer|journal=New England Journal of Medicine|volume=361|issue=12|year=2009|pages=1179–1187|issn=0028-4793|doi=10.1056/NEJMcp0902176}}</ref> | The most common indicator of high risk is a first-degree relative with colorectal cancer, a personal history of [[inflammatory bowel disease]].<ref name="Lieberman2009">{{cite journal|last1=Lieberman|first1=David A.|title=Screening for Colorectal Cancer|journal=New England Journal of Medicine|volume=361|issue=12|year=2009|pages=1179–1187|issn=0028-4793|doi=10.1056/NEJMcp0902176}}</ref> | ||
*If the first-degree relative was diagnosed with CRC before 50 years of age | *If the first-degree relative was diagnosed with CRC before 50 years of age | ||
:*The individual should be suspected of a hereditary syndrome | :*The individual should be suspected of a hereditary syndrome | ||
:*A complete family history, genetic counseling and testing, and an appropriate timing for endoscopic surveillance should be obtained | :*A complete family history, genetic counseling and testing, and an appropriate timing for [[endoscopic]] surveillance should be obtained | ||
*If a first-degree relative was diagnosed with CRC at 50 years of age or older the lifetime risk of CRC nearly doubles among his or her family members | *If a first-degree relative was diagnosed with CRC at 50 years of age or older the lifetime risk of CRC nearly doubles among his or her family members | ||
===Clinical practice guidelines=== | ===Clinical practice guidelines=== | ||
'''[[Clinical practice guideline]]s by the United States Preventive Service Task Force ([[USPSTF]]) in 2008 stated:'''<ref name="pmid18838716">{{cite journal| author=U.S. Preventive Services Task Force| title=Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement. | journal=Ann Intern Med | year= 2008 | volume= 149 | issue= 9 | pages= 627-37 | pmid=18838716 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18838716 }} </ref> | '''[[Clinical practice guideline]]s by the United States Preventive Service Task Force ([[USPSTF]]) in 2008 stated:'''<ref name="pmid18838716">{{cite journal| author=U.S. Preventive Services Task Force| title=Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement. | journal=Ann Intern Med | year= 2008 | volume= 149 | issue= 9 | pages= 627-37 | pmid=18838716 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18838716 }} </ref> | ||
*"The USPSTF recommends screening for colorectal cancer using fecal occult blood testing, sigmoidoscopy, or colonoscopy in adults, beginning at age 50 years and continuing until age 75 years" | *"The USPSTF recommends screening for colorectal cancer using [[Fecal occult blood test|fecal occult blood testing]], [[sigmoidoscopy]], or [[colonoscopy]] in adults, beginning at age 50 years and continuing until age 75 years" | ||
*"The USPSTF recommends against routine screening for colorectal cancer in adults 76 to 85 years of age. There may be considerations that support colorectal cancer screening in an individual patient" | *"The USPSTF recommends against routine screening for colorectal cancer in adults 76 to 85 years of age. There may be considerations that support colorectal cancer screening in an individual patient" | ||
*"The USPSTF recommends against screening for colorectal cancer in adults older than age 85 years" | *"The USPSTF recommends against screening for colorectal cancer in adults older than age 85 years" | ||
The USPSTF concludes that the evidence is insufficient to assess the benefits and harms of computed | The USPSTF concludes that the evidence is insufficient to assess the benefits and harms of [[Computed tomographic imaging|computed topographic colonography]] and fecal DNA testing as screening modalities for colorectal cancer. | ||
'''The American College of Gastroenterology recommends:'''<ref>Rex DK, Johnson DA, Anderson JC, et al. American College of Gastroenterology guidelines for colorectal cancer screening 2009.Am J Gastroenterol. 2009 Mar;104(3):739-50.</ref> | '''The American College of Gastroenterology recommends:'''<ref>Rex DK, Johnson DA, Anderson JC, et al. American College of Gastroenterology guidelines for colorectal cancer screening 2009.Am J Gastroenterol. 2009 Mar;104(3):739-50.</ref> | ||
* Screening in African Americans should begin at age 45 years | * Screening in African Americans should begin at age 45 years | ||
* CT colonography every 5 years is the radiographic screening alternative, when patients decline colonoscopy | * [[Computed tomography|CT colonography]] every 5 years is the radiographic screening alternative, when patients decline [[colonoscopy]] | ||
* Fecal immunochemical test for blood (FIT) is preferred over guaiac-based fecal occult blood testing | * Fecal immunochemical test for blood (FIT) is preferred over guaiac-based [[Fecal occult blood test|fecal occult blood testing]] | ||
===Types of Screening Methods=== | ===Types of Screening Methods=== | ||
| Line 50: | Line 50: | ||
====Endoscopy==== | ====Endoscopy==== | ||
*A [[sigmoidoscopy]] is a lighted probe (sigmoidoscope) that is inserted into the rectum and lower colon to check for polyps and other abnormalities | *A [[sigmoidoscopy]] is a lighted probe ([[sigmoidoscope]]) that is inserted into the [[rectum]] and lower [[colon]] to check for [[polyps]] and other abnormalities | ||
*A [[colonoscopy]] is a lighted probe (colonoscope) that is inserted into the rectum and the entire colon to look for [[polyp (medicine)|polyp]]s and other abnormalities that may be caused by cancer. A colonoscopy has the advantage that if [[polyp (medicine)|polyp]]s are found during the procedure they can be immediately removed, and the tissue can also be taken for [[biopsy]]. The [http://www.asge.org/ American Society for Gastrointestinal Endoscopy] has released quality indicators for screening colonoscopy, which include:<ref name="pmid16635231">{{cite journal| author=Rex DK, Petrini JL, Baron TH, Chak A, Cohen J, Deal SE et al.| title=Quality indicators for colonoscopy. | journal=Am J Gastroenterol | year= 2006 | volume= 101 | issue= 4 | pages= 873-85 | pmid=16635231 | doi=10.1111/j.1572-0241.2006.00673.x | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16635231 }} </ref> | *A [[colonoscopy]] is a lighted probe ([[colonoscope]]) that is inserted into the [[rectum]] and the entire [[colon]] to look for [[polyp (medicine)|polyp]]s and other abnormalities that may be caused by [[cancer]]. A [[colonoscopy]] has the advantage that if [[polyp (medicine)|polyp]]s are found during the procedure they can be immediately removed, and the tissue can also be taken for [[biopsy]]. The [http://www.asge.org/ American Society for Gastrointestinal Endoscopy] has released quality indicators for screening [[colonoscopy]], which include:<ref name="pmid16635231">{{cite journal| author=Rex DK, Petrini JL, Baron TH, Chak A, Cohen J, Deal SE et al.| title=Quality indicators for colonoscopy. | journal=Am J Gastroenterol | year= 2006 | volume= 101 | issue= 4 | pages= 873-85 | pmid=16635231 | doi=10.1111/j.1572-0241.2006.00673.x | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16635231 }} </ref> | ||
:*Documentation of prep quality | :*Documentation of prep quality | ||
:*Photo documentation of cecal intubation | :*Photo documentation of [[Cecum|cecal]] [[intubation]] | ||
:*Withdrawal time of 6 minutes or more | :*Withdrawal time of 6 minutes or more | ||
:*Adenoma detection rate of greater than 25% in males and 15% in females greater than 50 years old. | :*[[Adenoma]] detection rate of greater than 25% in males and 15% in females greater than 50 years old. | ||
[[Image:Colorectal cancer endo 2.jpg| | <figure-inline>[[Image:Colorectal cancer endo 2.jpg|473x473px]]</figure-inline> | ||
====Genetic Testing==== | ====Genetic Testing==== | ||
| Line 64: | Line 64: | ||
====Other Screening Techniques==== | ====Other Screening Techniques==== | ||
*Double contrast barium enema (DCBE) | *Double contrast barium enema (DCBE) | ||
:*First, an overnight preparation is taken to cleanse the colon. An [[enema]] containing [[barium sulfate]] is administered, then air is insufflated into the colon, distending it. The result is a thin layer of barium over the inner lining of the colon which is visible on X-ray films. A cancer or a precancerous polyp can be detected this way. This technique can miss the (less common) flat polyp. | :*First, an overnight preparation is taken to cleanse the colon. | ||
:*An [[enema]] containing [[barium sulfate]] is administered, then air is insufflated into the [[colon]], distending it. | |||
:*The result is a thin layer of [[barium]] over the inner lining of the [[colon]] which is visible on X-ray films. | |||
:*A [[cancer]] or a [[Precancerous|precancerous polyp]] can be detected this way. | |||
:*This technique can miss the (less common) flat [[polyp]]. | |||
*[[Virtual colonoscopy]] | *[[Virtual colonoscopy]] | ||
:* This is also known as CT colonography | :* This is also known as CT colonography | ||
:* This replaces X-ray films in the double contrast barium enema (above) with a special [[computed tomography]] scan | :* This replaces [[X-ray]] films in the double contrast barium enema (above) with a special [[computed tomography]] scan. | ||
:* It requires special workstation software in order for the [[radiologist]] to interpret. | |||
:* This technique is approaching [[colonoscopy]] in sensitivity for [[polyps]]. However, any polyps found must still be removed by standard [[colonoscopy]]. | |||
*[[Blood tests]] | *[[Blood tests]] | ||
:*The measurement of the patient's blood for elevated levels of certain [[proteins]] can give an indication of tumor load. | :*The measurement of the patient's blood for elevated levels of certain [[proteins]] can give an indication of tumor load. | ||
:*High levels of [[carcinoembryonic antigen]] (CEA) in the blood can indicate [[metastasis]] of [[adenocarcinoma]]. | |||
:*These tests are frequently [[Type I and type II errors|false positive]] or [[Type I and type II errors|false negative]], and are not recommended for screening, it can be useful to assess disease recurrence. | |||
* Stool DNA testing | * Stool DNA testing | ||
:* This detects DNA that sheds into the stool from the cells of pre-malignant adenomas and cancers. The DNA is not degraded during the digestive process and remains in the stool. | :* This detects DNA that sheds into the stool from the cells of [[Precancerous|pre-malignant]] [[adenomas]] and [[cancers]]. | ||
:* The DNA is not degraded during the digestive process and remains in the stool. | |||
==References== | ==References== | ||
Revision as of 18:37, 15 December 2017
|
Colorectal cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Colorectal cancer screening On the Web |
|
American Roentgen Ray Society Images of Colorectal cancer screening |
|
Risk calculators and risk factors for Colorectal cancer screening |
To view the screening of familial adenomatous polyposis (FAP), click here
To view the screening of hereditary nonpolyposis colorectal cancer (HNPCC), click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Elliot B. Tapper, M.D.; Saarah T. Alkhairy, M.D.
Overview
Current guidelines recommend that colonoscopy is the optimal screening tool for colon cancer since it detects 98-99% of the cases. High risk individuals include a first-degree relative with colorectal cancer. A colonoscopy every 10 years reduces the risk of left-sided colon cancer. Right sided colon cancers are more likely to be missed because they are harder to reach and they could be flat, which means they would be harder to detect. Flat growths (non-polypoid) are difficult to detect and are more likely to progress to colon cancer compared to cylindrical polyps.
Colorectal Cancer Screening
Colorectal cancer may take several years to develop. If colorectal cancer is detected early, the chances of a cure is greatly improved. The patient population can be divided into average, moderate, and high risk.
The algorithm below demonstrates a screening protocol for average risk patients.[1]
<figure-inline>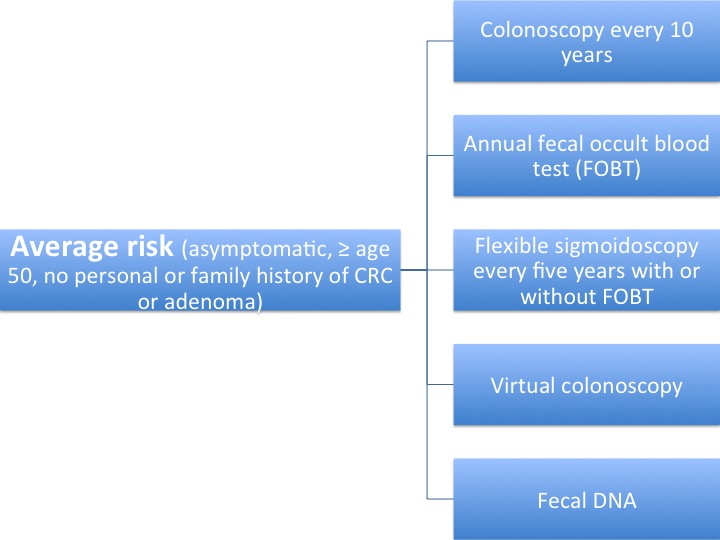 </figure-inline>
</figure-inline>
The algorithm below demonstrates a screening protocol for moderate risk patients.[2]
<figure-inline> </figure-inline>
</figure-inline>
The algorithm below demonstrates a screening protocol for high risk patients.[3]
<figure-inline> </figure-inline>
</figure-inline>
The most common indicator of high risk is a first-degree relative with colorectal cancer, a personal history of inflammatory bowel disease.[4]
- If the first-degree relative was diagnosed with CRC before 50 years of age
- The individual should be suspected of a hereditary syndrome
- A complete family history, genetic counseling and testing, and an appropriate timing for endoscopic surveillance should be obtained
- If a first-degree relative was diagnosed with CRC at 50 years of age or older the lifetime risk of CRC nearly doubles among his or her family members
Clinical practice guidelines
Clinical practice guidelines by the United States Preventive Service Task Force (USPSTF) in 2008 stated:[5]
- "The USPSTF recommends screening for colorectal cancer using fecal occult blood testing, sigmoidoscopy, or colonoscopy in adults, beginning at age 50 years and continuing until age 75 years"
- "The USPSTF recommends against routine screening for colorectal cancer in adults 76 to 85 years of age. There may be considerations that support colorectal cancer screening in an individual patient"
- "The USPSTF recommends against screening for colorectal cancer in adults older than age 85 years"
The USPSTF concludes that the evidence is insufficient to assess the benefits and harms of computed topographic colonography and fecal DNA testing as screening modalities for colorectal cancer.
The American College of Gastroenterology recommends:[6]
- Screening in African Americans should begin at age 45 years
- CT colonography every 5 years is the radiographic screening alternative, when patients decline colonoscopy
- Fecal immunochemical test for blood (FIT) is preferred over guaiac-based fecal occult blood testing
Types of Screening Methods
Fecal Occult Blood Testing
- A fecal occult blood test (FOBT) is a test for blood in the stool
- There are two types of tests that can be used for detecting occult blood in stools: guaiac-based (chemical test) and immunochemical
Endoscopy
- A sigmoidoscopy is a lighted probe (sigmoidoscope) that is inserted into the rectum and lower colon to check for polyps and other abnormalities
- A colonoscopy is a lighted probe (colonoscope) that is inserted into the rectum and the entire colon to look for polyps and other abnormalities that may be caused by cancer. A colonoscopy has the advantage that if polyps are found during the procedure they can be immediately removed, and the tissue can also be taken for biopsy. The American Society for Gastrointestinal Endoscopy has released quality indicators for screening colonoscopy, which include:[7]
- Documentation of prep quality
- Photo documentation of cecal intubation
- Withdrawal time of 6 minutes or more
- Adenoma detection rate of greater than 25% in males and 15% in females greater than 50 years old.
<figure-inline>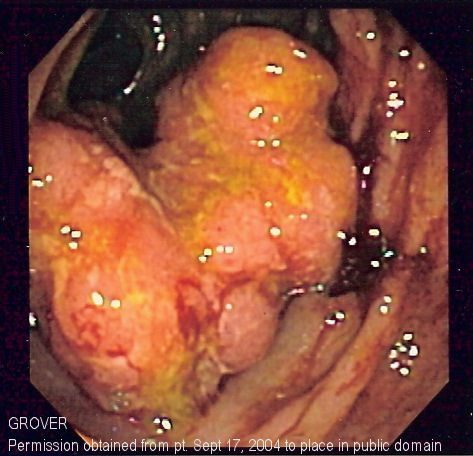 </figure-inline>
</figure-inline>
Genetic Testing
- Genetic counseling and genetic testing is a screening modality for families who may have a hereditary form of colon cancer, such as hereditary nonpolyposis colorectal cancer (HNPCC) or familial adenomatous polyposis (FAP)
Other Screening Techniques
- Double contrast barium enema (DCBE)
- First, an overnight preparation is taken to cleanse the colon.
- An enema containing barium sulfate is administered, then air is insufflated into the colon, distending it.
- The result is a thin layer of barium over the inner lining of the colon which is visible on X-ray films.
- A cancer or a precancerous polyp can be detected this way.
- This technique can miss the (less common) flat polyp.
- This is also known as CT colonography
- This replaces X-ray films in the double contrast barium enema (above) with a special computed tomography scan.
- It requires special workstation software in order for the radiologist to interpret.
- This technique is approaching colonoscopy in sensitivity for polyps. However, any polyps found must still be removed by standard colonoscopy.
- The measurement of the patient's blood for elevated levels of certain proteins can give an indication of tumor load.
- High levels of carcinoembryonic antigen (CEA) in the blood can indicate metastasis of adenocarcinoma.
- These tests are frequently false positive or false negative, and are not recommended for screening, it can be useful to assess disease recurrence.
- Stool DNA testing
- This detects DNA that sheds into the stool from the cells of pre-malignant adenomas and cancers.
- The DNA is not degraded during the digestive process and remains in the stool.
References
- ↑ https://www.rmf.harvard.edu/~/media/Files/_Global/KC/PDFs/RMFCRC.pdf
- ↑ https://www.rmf.harvard.edu/~/media/Files/_Global/KC/PDFs/RMFCRC.pdf
- ↑ https://www.rmf.harvard.edu/~/media/Files/_Global/KC/PDFs/RMFCRC.pdf
- ↑ Lieberman, David A. (2009). "Screening for Colorectal Cancer". New England Journal of Medicine. 361 (12): 1179–1187. doi:10.1056/NEJMcp0902176. ISSN 0028-4793.
- ↑ U.S. Preventive Services Task Force (2008). "Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement". Ann Intern Med. 149 (9): 627–37. PMID 18838716.
- ↑ Rex DK, Johnson DA, Anderson JC, et al. American College of Gastroenterology guidelines for colorectal cancer screening 2009.Am J Gastroenterol. 2009 Mar;104(3):739-50.
- ↑ Rex DK, Petrini JL, Baron TH, Chak A, Cohen J, Deal SE; et al. (2006). "Quality indicators for colonoscopy". Am J Gastroenterol. 101 (4): 873–85. doi:10.1111/j.1572-0241.2006.00673.x. PMID 16635231.