Chlamydia trachomatis: Difference between revisions
No edit summary |
No edit summary |
||
| Line 58: | Line 58: | ||
:::* Alternative regimen (2):[[ Erythromycin]] base 500 mg PO qid for 7 days {{or}} [[Erythromycin]]base 250 mg PO qid for 14 days | :::* Alternative regimen (2):[[ Erythromycin]] base 500 mg PO qid for 7 days {{or}} [[Erythromycin]]base 250 mg PO qid for 14 days | ||
:::* Alternative regimen (3):[[ Erythromycin]] ethylsuccinate 800 mg PO qid for 7 days {{or}} [[Erythromycin]] ethylsuccinate 400 mg PO four qid for 14days | :::* Alternative regimen (3):[[ Erythromycin]] ethylsuccinate 800 mg PO qid for 7 days {{or}} [[Erythromycin]] ethylsuccinate 400 mg PO four qid for 14days | ||
::* Chlamydial infection among neonates | |||
::*Ophthalmia Neonatorum | |||
:::* Preferred regimen :[[ Erythromycin]] base or ethylsuccinate ,PO 50 mg/kg/ day divided into 4 doses daily for 14 days | |||
:::* Alternative regimen : [[Azithromycin ]]suspension, PO 20 mg/kg /day qd for 3 days | |||
::*Infant Pneumonia | |||
:::* Preferred regimen :[[ Erythromycin]] base or ethylsuccinate PO 50 mg/kg/ day divided into 4 doses daily for 14 days | |||
:::* Alternative regimen : [[Azithromycin ]]suspension, PO 20 mg/kg /day qd for 3 days | |||
Revision as of 19:10, 24 June 2015
| Chlamydia trachomatis | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
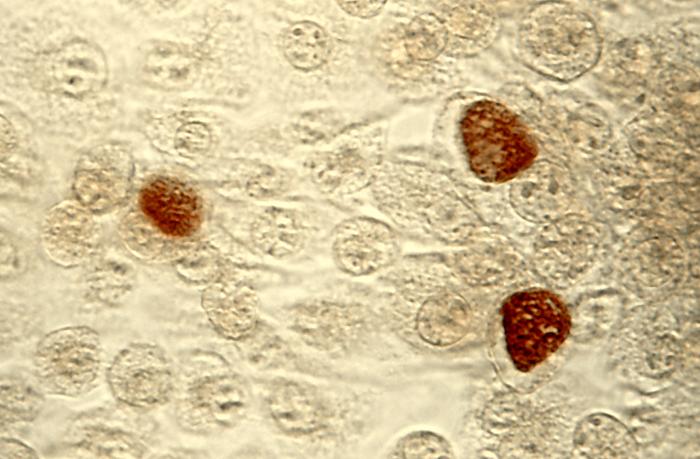 C. trachomatis inclusion bodies (brown) in a McCoy cell culture.
| ||||||||||||
| Scientific classification | ||||||||||||
| ||||||||||||
| Binomial name | ||||||||||||
| Chlamydia trachomatis Busacca, 1935 |
Chlamydia trachomatis is one of three bacterial species in the genus Chlamydia, family Chlamydiaceae, class Chlamydiae, phylum Chlamydiae, domain Bacteria. C. trachomatis has only been found living inside the cells of humans, causing the following conditions:
In men
In women
- Cervicitis
- Pelvic inflammatory disease (PID)
- Premature birth
- Ectopic pregnancy
- Pelvic pain, chronic or acute
- Newborn eye (trachoma) or lung infection
In both sexes
- Lymphogranuloma venereum
- Urethritis
- Infertility
- Proctitis (rectal disease and bleeding)
- Reactive arthritis
- Trachoma
C. trachomatis has also been detected in some patients with temporomandibular joint (TMJ) disease. It may be treated with any of several antibiotics: azithromycin, erythromycin or doxycycline/tetracycline.
C. trachomatis was the first chlamydial agent discovered in humans. It comprises two human biovars: trachoma and lymphogranuloma venereum (LGV). Many, but not all, C. trachomatis strains have an extrachromosomal plasmid. Chlamydia species are readily identified and distinguished from other chlamydial species using DNA-based tests. Most strains of C. trachomatis are recognized by monoclonal antibodies [mAbs] to epitopes in the VS4 region of MOMP. However, these mAbs may also crossreact with the other two Chlamydia species, Chlamydia suis and Chlamydia muridarum.
- Chlamydophila pneumoniae
- Chlamydophila pneumoniae
- Pneumonia[1]
- Chlamydial Infections in Adolescents and Adults
- Preferred regimen : Doxycycline 100 mg PO bid for 7 days OR Azithromycin 1 g PO in a single dose
- Alternative regimen (1): Erythromycin base 500 mg PO qid for 7 days OR Erythromycin ethylsuccinate 800 mg PO qid for 7 days
- Alternative regimen (2): Levofloxacin 500 mg PO qd for 7 days OR Ofloxacin 300 mg PO bid for 7 days.
- Pregancy
- Preferred regimen :Azithromycin 1 g PO in a single dose
- Alternative regimen (1):Amoxicillin 500 mg PO tid for 7 days
- Alternative regimen (2):Erythromycin base 500 mg PO qid for 7 days OR Erythromycinbase 250 mg PO qid for 14 days
- Alternative regimen (3):Erythromycin ethylsuccinate 800 mg PO qid for 7 days OR Erythromycin ethylsuccinate 400 mg PO four qid for 14days
- Chlamydial infection among neonates
- Ophthalmia Neonatorum
- Preferred regimen :Erythromycin base or ethylsuccinate ,PO 50 mg/kg/ day divided into 4 doses daily for 14 days
- Alternative regimen : Azithromycin suspension, PO 20 mg/kg /day qd for 3 days
- Infant Pneumonia
- Preferred regimen :Erythromycin base or ethylsuccinate PO 50 mg/kg/ day divided into 4 doses daily for 14 days
- Alternative regimen : Azithromycin suspension, PO 20 mg/kg /day qd for 3 days
Gallery
-
Photomicrograph of Chlamydia trachomatis taken from a urethral scrape. From Public Health Image Library (PHIL). [2]
-
McCoy cell monolayers with Chlamydia trachomatis inclusion bodies (200X mag). From Public Health Image Library (PHIL). [2]
-
McCoy cell monolayers with Chlamydia trachomatis inclusion bodies (50X mag). From Public Health Image Library (PHIL). [2]
-
Photomicrograph depicts HeLa cells infected with Type-A Chlamydia trachomatis (400X mag). From Public Health Image Library (PHIL). [2]
-
Patient’s left eye with the upper lid retracted in order to reveal the inflamed conjunctival membrane lining the inside of both the upper and lower lids, due to what was determined to be a case of inclusion conjunctivitis caused by the bacterium, Chlamydia trachomatis. From Public Health Image Library (PHIL). [2]
External links
- Chlamydiae.com [1]
- Template:GPnotebook
- article at reuters.com
ar:تراخوما da:Klamydia de:Chlamydia trachomatis nl:Chlamydia trachomatis no:Chlamydia trachomatis uk:Chlamydia trachomatis
- ↑ Bennett, John (2015). Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Philadelphia, PA: Elsevier/Saunders. ISBN 978-1455748013.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 "Public Health Image Library (PHIL)".
![Photomicrograph of Chlamydia trachomatis taken from a urethral scrape. From Public Health Image Library (PHIL). [2]](/images/2/21/Chlamydia15.jpeg)
![McCoy cell monolayers with Chlamydia trachomatis inclusion bodies (200X mag). From Public Health Image Library (PHIL). [2]](/images/8/88/Chlamydia11.jpeg)
![McCoy cell monolayers with Chlamydia trachomatis inclusion bodies (50X mag). From Public Health Image Library (PHIL). [2]](/images/e/e2/Chlamydia10.jpeg)
![Photomicrograph depicts HeLa cells infected with Type-A Chlamydia trachomatis (400X mag). From Public Health Image Library (PHIL). [2]](/images/2/29/Chlamydia09.jpeg)
![Patient’s left eye with the upper lid retracted in order to reveal the inflamed conjunctival membrane lining the inside of both the upper and lower lids, due to what was determined to be a case of inclusion conjunctivitis caused by the bacterium, Chlamydia trachomatis. From Public Health Image Library (PHIL). [2]](/images/3/3c/Chlamydia03.jpeg)
![From Public Health Image Library (PHIL). [2]](/images/0/01/Chlamydia04.jpeg)