Cervical cancer pathophysiology: Difference between revisions
Nima Nasiri (talk | contribs) |
Nima Nasiri (talk | contribs) |
||
| Line 9: | Line 9: | ||
=== '''Pathogenesis:''' === | === '''Pathogenesis:''' === | ||
A range of putative cofactors has been implicated in progression: HLA type, immunosuppression, sex steroid hormones, and smoking; most of these cofactors | |||
Infection with Human papilloma virus is the main cause of cervical cancer, only certain strain of high risk HPV can cause cervical cancer. <ref name="pmid12525422">{{cite journal |vauthors=Burd EM |title=Human papillomavirus and cervical cancer |journal=Clin. Microbiol. Rev. |volume=16 |issue=1 |pages=1–17 |date=January 2003 |pmid=12525422 |pmc=145302 |doi= |url=}}</ref> | Infection with Human papilloma virus is the main cause of cervical cancer, only certain strain of high risk HPV can cause cervical cancer. <ref name="pmid12525422">{{cite journal |vauthors=Burd EM |title=Human papillomavirus and cervical cancer |journal=Clin. Microbiol. Rev. |volume=16 |issue=1 |pages=1–17 |date=January 2003 |pmid=12525422 |pmc=145302 |doi= |url=}}</ref> | ||
| Line 15: | Line 15: | ||
*Two major viral oncogenes, E6 and E7, directly coupled to viral enhancers and promoters, allowing their continued expression after integration. High risk HPV E7 proteins bind and inactivate the Rb protein, whereas E6 proteins bind p53 and direct its rapid degradation. | *Two major viral oncogenes, E6 and E7, directly coupled to viral enhancers and promoters, allowing their continued expression after integration. High risk HPV E7 proteins bind and inactivate the Rb protein, whereas E6 proteins bind p53 and direct its rapid degradation. | ||
* Important factors in causing cervical cancer: | * Important factors in causing cervical cancer: | ||
** HLA type | |||
** Immunosuppression | |||
** Sex steroid hormones | |||
** Smoking | |||
== Genetic: == | == Genetic: == | ||
Revision as of 20:52, 8 February 2019
|
Cervical cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Cervical cancer pathophysiology On the Web |
|
American Roentgen Ray Society Images of Cervical cancer pathophysiology |
|
Risk calculators and risk factors for Cervical cancer pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]}Associate Editor(s)-in-Chief: Monalisa Dmello, M.B,B.S., M.D. [2] Aida Javanbakht, M.D.
Overview
It is estalished that human papillomavirus (HPV) is central to the development of cervical neoplasia, only high risk strain of HPV can cause cervical cancer among women whom are affected. This is mainly because of HPV produced proteins E7 which alters epithelium of cervix mainly at junctional zone.
Pathophysiology
Pathogenesis:
A range of putative cofactors has been implicated in progression: HLA type, immunosuppression, sex steroid hormones, and smoking; most of these cofactors
Infection with Human papilloma virus is the main cause of cervical cancer, only certain strain of high risk HPV can cause cervical cancer. [1]
- Human papillomaviruses, a sexually transmitted virus, subtypes 16 and 18 (High risk) play an important role in the pathogenesis of cervical cancer. Once HPV enters an epithelial cell, begins to make the proteins.
- Two major viral oncogenes, E6 and E7, directly coupled to viral enhancers and promoters, allowing their continued expression after integration. High risk HPV E7 proteins bind and inactivate the Rb protein, whereas E6 proteins bind p53 and direct its rapid degradation.
- Important factors in causing cervical cancer:
- HLA type
- Immunosuppression
- Sex steroid hormones
- Smoking
Genetic:
Associated Conditions:
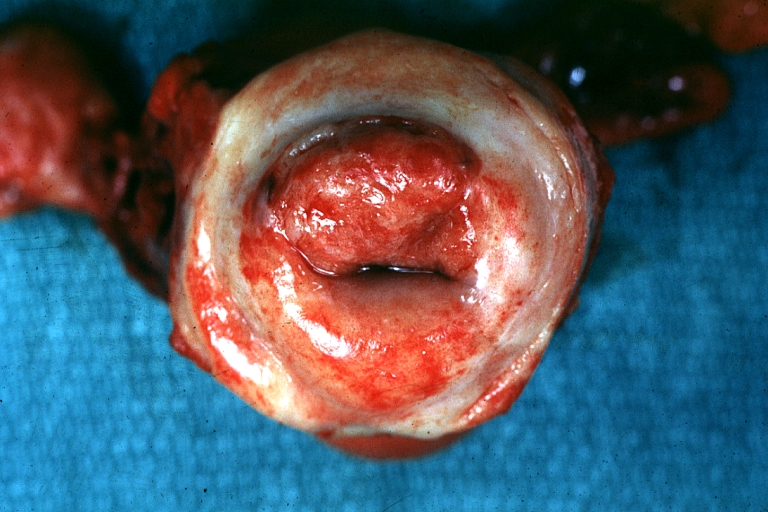
Gross Pathology:
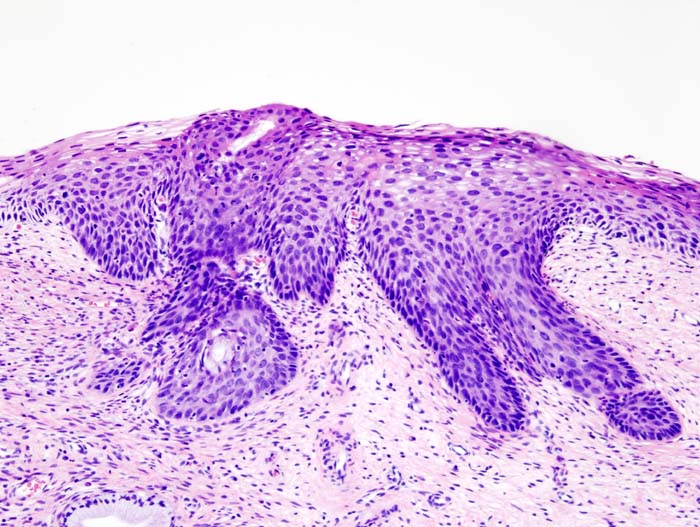
Microscopic pathology
- Prominent nucleoli.
- Blurred or scalloped epithelial-stromal interface.
- Loss of nuclear polarity.
- Pseudoglandular pattern because of acantholysis and central necrosis.
-
Uterus: Cervical Carcinoma: Gross, an excellent example of tumor (labeled as invasive)
Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology -
Histopathologic image (H&E stain) of cervical intraepithelial neoplasia.
Video
{{#ev:youtube|J3kULzKGzws}}