|
|
| (43 intermediate revisions by 4 users not shown) |
| Line 1: |
Line 1: |
| | __NOTOC__ |
| {{Infobox_Disease | | {{Infobox_Disease |
| | Name = {{PAGENAME}} | | | Name = {{PAGENAME}} |
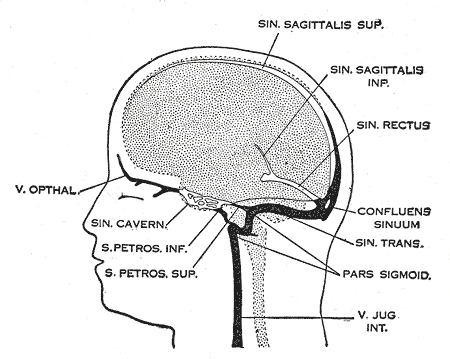
| | Image = Gray488.png | | | Image = Gray488.png |
| | Caption = Dural veins | | | Caption = Dural veins |
| | DiseasesDB = 2242
| |
| | ICD10 = {{ICD10|I|63|6|i|60}}, {{ICD10|I|67|6|i|60}}
| |
| | ICD9 = {{ICD9|325}}, {{ICD9|437.6}}
| |
| | ICDO =
| |
| | OMIM =
| |
| | MedlinePlus =
| |
| | eMedicineSubj =
| |
| | eMedicineTopic =
| |
| | eMedicine_mult = |
| |
| | MeshID =
| |
| }} | | }} |
| {{CMG}} | | {{CMG}}; {{AE}} {{KD}}{{SharmiB}} |
| {{Cerebral venous sinus thrombosis}} | | {{Cerebral venous sinus thrombosis}} |
| | |
| '''''Keywords and synonyms:''''' Cerebral venous thrombosis, cerebral sinus thrombosis, superior sagittal sinus thrombosis, dural sinus thrombosis and intracranial venous thrombosis | | '''''Keywords and synonyms:''''' Cerebral venous thrombosis, cerebral sinus thrombosis, superior sagittal sinus thrombosis, dural sinus thrombosis and intracranial venous thrombosis |
|
| |
|
| ==Overview== | | ==[[Cerebral venous sinus thrombosis overview|Overview]]== |
| | |
| ==Pathophysiology==
| |
| The [[vein]]s of the brain, both the superficial veins and the deep venous system, empty into the [[dural venous sinuses]], which carry blood back to the [[jugular vein]]. In cerebral venous sinus thrombosis, blood clots usually form both in the veins of the brain and the venous sinuses. The thrombosis of the veins themselves causes [[cerebral edema|cerebral oedema]] (both ''vasogenic'' and ''cytotoxic'' oedema) through back pressure, and small [[petechia]]l haemorrhages that may merge into large haematomas. Thrombosis of the sinuses is the main mechanism behind the increase in intracranial pressure due to decreased resorption of [[cerebrospinal fluid]] (CSF). Because this process is generalised, the condition does not lead to [[hydrocephalus]].<ref name=Stam2005/>
| |
| | |
| Any blood clot forms due to an imbalance between [[coagulation]] (the formation of the insoluble blood protein [[fibrin]]) and [[fibrinolysis]]. The three major mechanisms for such an imbalance are enumerated in [[Virchow's triad]]: alterations in normal blood flow, injury to the blood vessel wall, and alterations in the constitution of blood (hypercoagulability). Most cases of cerebral venous sinus thrombosis are due to hypercoagulability.<ref name=Stam2005/>
| |
| | |
| It is possible for the clot to break off and migrate ([[embolism]]) to the [[lung]]s, causing a [[pulmonary embolism]].<ref name=Stam2005/><ref name=EFNS/> An analysis of previous case reports concludes that this occurs in about 10% of cases, but has a very poor prognosis.<ref>{{cite journal |author=Diaz JM, Schiffman JS, Urban ES, Maccario M |title=Superior sagittal sinus thrombosis and pulmonary embolism: a syndrome rediscovered |journal=Acta Neurol. Scand. |volume=86 |issue=4 |pages=390–6 |year=1992 |pmid=1455986 |doi=}}</ref>
| |
| ==Epidemiology and Demographics==
| |
| Cerebral venous sinus thrombosis is rare, with 3-4 per million annual incidence in adults and 7 per million incidence in children (predominantly in the newborn<ref name=EFNS/>). 75% of cases are in women; some historical evidence suggests that the use of [[oral contraceptive]]s in women is behind the disparity between the sexes.<ref name=Stam2005/> In adults, the disease occurs most often in the third decade.<ref name=EFNS/>
| |
|
| |
|
| ==Risk factors== | | ==[[Cerebral venous sinus thrombosis historical perspective|Historical Perspective]]== |
| Cerebral venous sinus thrombosis is more common in particular situations. 85% of patients have at least one of these risk factors:<ref name=Stam2005/> | |
| * [[Thrombophilia]] (a tendency to develop blood clots due to abnormalities in [[coagulation]], e.g. deficiency of [[protein C]], [[protein S]], [[antithrombin]] or related problems)
| |
| * [[Nephrotic syndrome]] (a kidney problem causing protein loss in the urine)
| |
| * Chronic inflammatory diseases ([[inflammatory bowel disease]], [[Lupus erythematosus|lupus]], [[Behçet's disease]])
| |
| * [[Pregnancy]] and [[puerperium]] (the period after giving birth)
| |
| * Particular blood disorders, especially [[polycythemia vera]] and [[paroxysmal nocturnal hemoglobinuria]]
| |
| * Use of the [[oral contraceptives|contraceptive pill]]
| |
| * [[Meningitis]] and infections of the ear, nose and throat area ([[mastoiditis]], [[sinusitis]])
| |
| * Direct injury to the venous sinuses, and medical procedures in the area
| |
|
| |
|
| Other less well understood situations that increase the risk for cerebral sinus thrombosis are [[hyperthyroidism]]<ref name="pmid17895204">{{cite journal |author=Dai A, Wasay M, Dubey N, Giglio P, Bakshi R |title=Superior sagittal sinus thrombosis secondary to hyperthyroidism |journal=Journal of stroke and cerebrovascular diseases : the official journal of National Stroke Association |volume=9 |issue=2 |pages=89–90 |year=2000 |pmid=17895204 |doi=10.1053/jscd.2000.0090089}}</ref> and [[myelodysplastic syndrome]].<ref name="pmid17895084">{{cite journal |author=Finelli PF, Harrison RB, Uphoff DF |title=Myelodysplastic syndrome and sagittal sinus thrombosis |journal=Journal of stroke and cerebrovascular diseases : the official journal of National Stroke Association |volume=7 |issue=3 |pages=211–2 |year=1998 |pmid=17895084 |doi=}}</ref>
| | ==[[Cerebral venous sinus thrombosis classification|Classification]]== |
|
| |
|
| ==Natural History, Complications and Prognosis== | | ==[[Cerebral venous sinus thrombosis pathophysiology|Pathophysiology]]== |
| In 2004 the first adequately large scale study on the natural history and long-term prognosis of this condition was reported and showed that at 16 months followup: 57.1% of patients had full recovery, 29.5%/2.9%/2.2% had respectively minor/moderate/severe symptoms or impairments, and 8.3% had died. Severe impairment or death were more likely in those aged over 37 years, male, affected by coma, mental status disorder, intracerebral hemorrhage, thrombosis of the deep cerebral venous system, central nervous system infection and cancer.<ref name="pmid14976332">{{cite journal |author=Ferro JM, Canhão P, Stam J, Bousser MG, Barinagarrementeria F |title=Prognosis of cerebral vein and dural sinus thrombosis: results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT) |journal=Stroke |volume=35 |issue=3 |pages=664–70 |year=2004 |pmid=14976332 |doi=10.1161/01.STR.0000117571.76197.26 |url=http://stroke.ahajournals.org/cgi/content/full/35/3/664}}</ref> A subsequent [[systematic review]] of nineteen studies in 2006 showed that mortality is about 5.6% during hospitalisation and 9.4% in total, while of the survivors 88% make a total or near-total recovery. After several months, two thirds of the cases has resolution ("recanalisation") of the clot. The rate of recurrence was low (2.8%).<ref>{{cite journal |author=Dentali F, Gianni M, Crowther MA, Ageno W |title=Natural history of cerebral vein thrombosis: a systematic review |journal=Blood |volume=108 |issue=4 |pages=1129–34 |year=2006 |pmid=16609071 |doi=10.1182/blood-2005-12-4795}}</ref>
| |
|
| |
|
| ==Diagnosis== | | ==[[Cerebral venous sinus thrombosis causes|Causes]]== |
| ===Symptoms===
| |
| Headache is a common presentation (present in 90% of cases); it tends to worsen over a period of several days, but may also develop suddenly ([[thunderclap headache]]).<ref name=Stam2005/> The headache may be the only symptom of cerebral venous sinus thrombosis.<ref name=Cumurciuc2005>{{cite journal |author=Cumurciuc R, Crassard I, Sarov M, Valade D, Bousser MG |title=Headache as the only neurological sign of cerebral venous thrombosis: a series of 17 cases |journal=J. Neurol. Neurosurg. Psychiatr. |volume=76 |issue=8 |pages=1084–7 |year=2005 |pmid=16024884 |doi=10.1136/jnnp.2004.056275}}</ref> Many patients have symptoms of [[stroke]]: inability to move one or more limbs, weakness on one side of the face or [[aphasia|difficulty speaking]]. This does not necessarily affect one side of the body as in "arterial" stroke.<ref name=Stam2005/> 40% of all patients have [[seizure]]s (more in women before and after birth<ref name=EFNS>{{cite journal |author=Einhäupl K, Bousser MG, de Bruijn SF, ''et al'' |title=EFNS guideline on the treatment of cerebral venous and sinus thrombosis |journal=Eur. J. Neurol. |volume=13 |issue=6 |pages=553–9 |year=2006 |pmid=16796579 |doi=10.1111/j.1468-1331.2006.01398.x}}</ref>), mostly [[Focal seizures|focal]] but often [[Tonic-clonic seizure|generalised]] and sometimes leading to [[status epilepticus]].<ref name=Stam2005/> In the elderly, many of the aforementioned symptoms may not occur. Common symptoms in the elderly with this condition are a [[coma|depressed level of consciousness]] and otherwise unexplained changes in [[mental status]].<ref>{{cite journal |author=Ferro JM, Canhão P, Bousser MG, Stam J, Barinagarrementeria F |title=Cerebral vein and dural sinus thrombosis in elderly patients |journal=Stroke |volume=36 |issue=9 |pages=1927–32 |year=2005 |pmid=16100024 |doi=10.1161/01.STR.0000177894.05495.54}}</ref>
| |
|
| |
|
| ===Physical Examination=== | | ==[[Cerebral venous sinus thrombosis differential diagnosis|Differentiating Cerebral venous sinus thrombosis from other Diseases]]== |
| The [[intracranial pressure]] (pressure around the brain) may rise, causing [[papilledema|papilloedema]] (swelling of the [[optic disc]], leading to visual obscurations). In severely raised intracranial pressure, there may be signs of [[coma|depressed level of consciousness]], rising [[blood pressure]], [[bradycardia|falling heart rate]] and abnormal posturing.<ref name=Stam2005/>
| |
|
| |
|
| ===Laboratory Findings=== | | ==[[Cerebral venous sinus thrombosis epidemiology and demographics|Epidemiology and Demographics]]== |
| The diagnosis may be suspected on the basis of the symptoms (e.g. the combination of headache, signs of raised [[intracranial pressure]] and focal neurological abnormalities), or when alternative causes of headache and neurological abnormalities (such as a [[subarachnoid hemorrhage]]) have been excluded.<ref name=Stam2005/>
| |
|
| |
|
| ;CT, MRI and angiography
| | ==[[Cerebral venous sinus thrombosis risk factors|Risk Factors]]== |
| There are various investigations that may detect cerebral sinus thrombosis. [[Cerebral oedema]] and venous infarction may be apparent on any modality, but for the detection of the thrombus itself, the most commonly used tests are [[computed tomography]] (CT) and [[magnetic resonance imaging]] (MRI), both using various types of [[radiocontrast]] to perform a [[venogram]]. [[Cerebral angiography]] may demonstrate smaller clots, and obstructed veins may give the "corkscrew appearance".<ref name=Stam2005/>
| |
|
| |
|
| [[Computed tomography]], with [[radiocontrast]] in the venous phase (''CT venography'' or CTV), has a detection rate that in some regards exceeds that of MRI. The test involves injection into a vein (usually in the arm) of a radioopaque substance, and time is allowed for the bloodstream to carry it to the cerebral veins - at which point the scan is performed. It has a [[sensitivity (tests)|sensitivity]] of 75-100% (it detects 75-100% of all clots present), and a [[specificity (tests)|specificity]] of 81-100% (it would be incorrectly positive in 0-19%). In the first two weeks, the "empty delta sign" may be observed (in later stages, this sign may disappear).<ref name=Smith2007>{{cite journal |author=Smith R, Hourihan MD |title=Investigating suspected cerebral venous thrombosis |journal=BMJ |volume=334 |issue=7597 |pages=794–5 |year=2007 |pmid=17431266 |doi=10.1136/bmj.39154.636968.47}}</ref> | | ==[[Cerebral venous sinus thrombosis natural history|Natural History, Complications and Prognosis]]== |
|
| |
|
| [[Magnetic resonance angiography|Magnetic resonance venography]] employs the same principles, but uses MRI as a scanning modality. MRI has the advantage of being better at detecting damage to the brain itself as a result of the increased pressure on the obstructed veins, but it is not readily available in many hospitals and the interpretation may be difficult.<ref name=Smith2007/>
| | ==Diagnosis== |
|
| |
|
| ;D-dimer
| | [[Cerebral venous sinus thrombosis history and symptoms| History and Symptoms]] | [[Cerebral venous sinus thrombosis physical examination | Physical Examination]] | [[Cerebral venous sinus thrombosis laboratory findings |Laboratory Findings]] | [[Cerebral venous sinus thrombosis CT|CT]] | [[Cerebral venous sinus thrombosis MRI|MRI]] | [[Cerebral venous sinus thrombosis other imaging findings|Other Imaging Findings]] | [[Cerebral venous sinus thrombosis other diagnostic studies|Other Diagnostic Studies]] |
| A 2004 German study suggested that the [[D-dimer]] blood test, already in use for the diagnosis of other forms of thrombosis, was abnormal (above 500 μg/l) in 34 out of 35 patients with cerebral sinus thrombosis, giving it a [[sensitivity (test)|sensitivity]] of 97.1%, a [[negative predictive value]] of 99.6%, a [[specificity]] of 91.2%, and a positive predictive value of 55.7%. Furthermore, the level of the D-dimer correlated with the extent of the thrombosis.<ref>{{cite journal |author=Kosinski CM, Mull M, Schwarz M, ''et al'' |title=Do normal D-dimer levels reliably exclude cerebral sinus thrombosis? |journal=Stroke |volume=35 |issue=12 |pages=2820–5 |year=2004 |pmid=15514174 |doi=10.1161/01.STR.0000147045.71923.18}}</ref> A subsequent 2005 study performed in France showed that 10% of patients with confirmed thrombosis had a normal D-dimer, and in those who had presented with only a headache 26% had a normal D-dimer. The study concludes that D-dimer is not useful in the situations where it would make the most difference (low-probability settings).<ref>{{cite journal |author=Crassard I, Soria C, Tzourio C, ''et al'' |title=A negative D-dimer assay does not rule out cerebral venous thrombosis: a series of seventy-three patients |journal=Stroke |volume=36 |issue=8 |pages=1716–9 |year=2005 |pmid=16020765 |doi=10.1161/01.STR.0000173401.76085.98}}</ref>
| |
| | |
| ===Further tests===
| |
| In most patients, the direct cause for the cerebral sinus thrombosis is not readily apparent. Identifying a source of infection is crucial, but it is common practice to screen for various forms of [[thrombophilia]] (a propensity to form blood clots).<ref name=Stam2005/>
| |
|
| |
|
| ==Treatment== | | ==Treatment== |
| Various studies have investigated the use of [[anticoagulation]] (suppression of blood clot formation) in cerebral venous sinus thrombosis. Before these trials, there was a concern that small areas of hemorrhage would bleed further as a result of treatment. The European Federation of Neurological Societies (EFNS) recommends [[heparin]] or [[low molecular weight heparin]] in the initial treatment, followed by [[warfarin]], provided there are no other bleeding risks that would make these treatments unsuitable.<ref name=EFNS/> The duration of warfarin treatment depends on the circumstances and underlying causes of the condition. If the thrombosis developed under temporary circumstances (e.g. pregnancy), three months are regarded as sufficient. If the condition was unprovoked but there are no clear causes or a "mild" form of thrombophilia, 6 to 12 months is advised. If there is a severe underlying thrombosis disorder, warfarin treatment may need to continue indefinitely.<ref name=EFNS/>
| |
|
| |
| [[Thrombolysis]] (removal of the blood clot with "clot buster" medication) has been described, either systemically by injection into a vein or directly into the clot during angiography. The 2006 EFNS guideline recommends that thrombolysis is only used in patients who deteriorate despite adequate treatment, and other causes of deterioration have been eliminated. It is unclear which drug and which mode of administration is the most effective. Bleeding into the brain and in other sites of the body is a major concern in the use of thrombolysis.<ref name=EFNS/>
| |
|
| |
|
| Raised intracranial pressure, if severe or threatening vision, may require therapeutic [[lumbar puncture]] (removal of excessive [[cerebrospinal fluid]]), medication ([[acetazolamide]]), or surgical treatment (optic nerve sheath fenestration or [[Cerebral shunt|shunting]]).<ref name=Stam2005/> In certain situations, anticonvulsants may be used prophylactically (i.e. to prevent seizures); these are focal neurological problems (e.g. inability to move a limb) and/or focal changes of the brain tissue on CT or MRI scan.<ref name=EFNS/>
| | [[Cerebral venous sinus thrombosis medical therapy| Medical Therapy]] | [[Cerebral venous sinus thrombosis surgery| Surgery]] | [[Cerebral venous sinus thrombosis primary prevention|Primary Prevention]] | [[Cerebral venous sinus thrombosis secondary prevention|Secondary Prevention]] | [[Cerebral venous sinus thrombosis cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Cerebral venous sinus thrombosis future or investigational therapies|Future or Investigational Therapies]] |
|
| |
|
| ==References== | | ==Case Studies== |
| {{reflist|2}}
| | [[Cerebral venous sinus thrombosis case study one|Case #1]] |
|
| |
|
| [[Category:Neurology]] | | [[Category:Neurology]] |
| | [[Category: Disease]] |
|
| |
|
| {{WH}} | | {{WH}} |
| {{WS}} | | {{WS}} |