Cardiopulmonary resuscitation

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Cardiopulmonary resuscitation (CPR) is an emergency medical procedure for a victim of cardiac arrest or, in some circumstances, respiratory arrest.[1] CPR is performed in hospitals, or in the community by laypersons or by emergency response professionals.[2]
CPR consists of artificial blood circulation and artificial respiration[1] (i.e. chest compressions and lung ventilation).[3] CPR is generally continued, usually in the presence of advanced life support, until the patient regains a heart beat (called "return of spontaneous circulation" or "ROSC") or is declared dead.
CPR is unlikely to restart the heart, but rather its purpose is to maintain a flow of oxygenated blood to the brain and the heart, thereby delaying tissue death and extending the brief window of opportunity for a successful resuscitation without permanent brain damage. Defibrillation and advanced life support are usually needed to restart the heart.
Historical Perspective
- CPR has been known in theory, if not practice, for many hundreds or even thousands of years; some claim it is described in the Bible, discerning a superficial similarity to CPR in a passage from the Books of Kings (II 4:34), wherein the Hebrew prophet Elisha warms a dead boy's body and "places his mouth over his".
- In the 19th century, doctor H. R. Silvester described a method (The Silvester Method) of artificial respiration in which the patient is laid on their back, and their arms are raised above their head to aid inhalation and then pressed against their chest to aid exhalation.[4]
- The procedure is repeated sixteen times per minute. This type of artificial respiration is occasionally seen in films made in the early part of the 20th century.
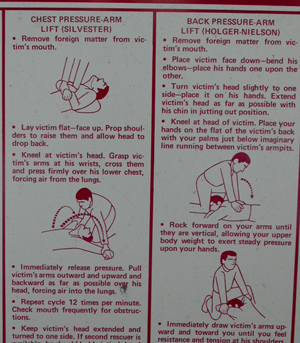
A second technique, called the Holger Neilson technique, described in the first edition of the Boy Scout Handbook in the United States in 1911, described a form of artificial respiration where the person was laid on their front, with their head to the side, and a process of lifting their arms and pressing on their back was utilized, essentially the Silvester Method with the patient flipped over. This form is seen well into the 1950s (it is used in an episode of Lassie during the Jeff Miller era), and was often used, sometimes for comedic effect, in theatrical cartoons of the time (see Tom and Jerry's "The Cat and the Mermouse"). This method would continue to be shown, for historical purposes, side-by-side with modern CPR in the Boy Scout Handbook until its ninth edition in 1979.
However it wasn't until the middle of the 20th century that the wider medical community started to recognise and promote it as a key part of resuscitation following cardiac arrest. Peter Safar wrote the book ABC of resuscitation in 1957. In the U.S., it was first promoted as a technique for the public to learn in the 1970s.
Use in Cardiac arrest
The medical term for the condition in which a person's heart has stopped is cardiac arrest[5] (also referred to as cardiorespiratory arrest). CPR is used on patients in cardiac arrest in order to oxygenate the blood and maintain a cardiac output to keep vital organs alive.
Blood circulation and oxygenation are absolute requirements in transporting oxygen to the tissues. The brain may sustain damage after blood flow has been stopped for about four minutes and irreversible damage after about seven minutes. If blood flow ceases for 1 or 2 hours, the cells of the body die unless they get an adequately gradual bloodflow, (provided by cooling and gradual warming, rarely, in nature [such as in a cold stream of water] or by an advanced medical team). Because of that CPR is generally only effective if performed within 7 minutes of the stoppage of blood flow.[6] The heart also rapidly loses the ability to maintain a normal rhythm. Low body temperatures as sometimes seen in drowning prolong the time the brain survives. Following cardiac arrest, effective CPR enables enough oxygen to reach the brain to delay brain death, and allows the heart to remain responsive to defibrillation attempts.
If the patient still has a pulse, but is not breathing, this is called respiratory arrest and artificial respiration is more appropriate. However, since people often have difficulty detecting a pulse, CPR may be used in both cases, especially when taught as first aid (see below).
First aid
CPR is part of the chain of survival, which includes early access (to emergency medical services), early CPR, early defibrillation, and early advanced care.[7] Some first aid trainers also advocate the performance of CPR as part of the choking protocol, if all else has failed.[8]
Sudden cardiac arrest is a leading cause of death, happening to approximately one in 8000 people per annum outside a hospital setting in the USA.[9] CPR can double or triple the victim's chances of survival when commenced immediately (see 'effectiveness' below). According to United States 'Annals of Emergency Medicine', only 25% of victims of a witnessed cardiac arrest are administered CPR by a bystander, with a further 33% receiving some CPR as a result of dispatcher instructions. This leaves 41% of victims receiving no CPR prior to the arrival of the emergency medical services.[10]
Rapid access to defibrillation is also vital. The most common cause of cardiac arrest outside of a hospital is ventricular fibrillation (VF), a potentially fatal arrhythmia that is usually (but not always) caused by a heart attack and is responsive to defibrillation. Other causes of cardiac arrest include drowning, drug overdose, poisoning, electrocution.
First aid training
CPR is taught to the general public in order to increase the chance to CPR being performed in the crucial few minutes before emergency personnel are available. Simple training is the goal of the 2005 guidelines to maximize the prospect that CPR will be performed successfully.
CPR is a practical skill and needs professional instruction followed up by regular practice on a resuscitation mannequin to gain and maintain full competency.
In most CPR classes, a simple mnemonic is used to aid memory of the clinical approach to the unconscious patient and CPR. The most common one used worldwide is ABC which stands for Airway, Breathing and Circulation. This may be built upon with extra information (and letters) and can reach complicated levels such as AcBCDEEEFG, explained further in the main article ABC (medical).
CPR skills are not confined to medical professionals, but are regularly taught to members of the public. Widespread knowledge of CPR has a community benefit, as CPR must be applied quickly after a patients heart has stopped. Early CPR in the community is essential to the prevention of brain damage during a cardiac arrest and increases the chance of survival. CPR maintains the blood flow and perfusion to the brain, buying time until a defibrillator and professional medical help arrives.
It is considered best to obtain training in CPR before a medical emergency occurs, although some modern ambulance dispatchers will talk an untrained lay rescuer through the process over the phone, whilst the crew is en-route. For the most effective results, hands-on training should be given by an expert. This will enable the person to perform CPR more safely and more effectively. Most organizations advocate regular retraining, in order to keep practice in the skills, and to ensure that the person is up to date with the latest guidelines, which change periodically based on the outputs from governing bodies.
First aid training, including CPR is often provided by a community organization or charity (with or without a fee), with international providers including the Red Cross and St. John Ambulance, or more local providers such as St. Andrew's Ambulance Association in Scotland or the American Heart Association in the United States. There are also many commercial organizations, who train members of the public or workers, where the course is paid for by employers who wish, or are required by law, to have trained first aiders on site.
Guidelines
In 2005, new CPR guidelines[11][12] were published by the International Resuscitation Councils, agreed at the 2005 International Consensus Conference on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science.[13][14] The primary goal of these changes was to simplify CPR for lay rescuers and healthcare providers alike, to maximise the potential for early resuscitation. The important changes for 2005 were:[9]
- A universal compression-ventilation ratio (30:2) recommended for all single rescuers of infant (less than one year old), child (1 year old to puberty), and adult (puberty and above) victims (excluding newborns).[15] The primary difference between the age groups is that with adults the rescuer uses two hands for the chest compressions, while with children it is only one, and with infants only two fingers (pointer and middle fingers). Whilst this simplification has been introduced, it has not been universally accepted, and especially amongst healthcare professionals, protocols may still vary.[16]
- The removal of the emphasis on lay rescuers assessing for pulse or signs of circulation for an unresponsive adult victim, instead taking the absence of normal breathing as the key indicator for commencing CPR.
- The removal of the protocol in which lay rescuers provide rescue breathing without chest compressions for an adult victim, with all cases such as these being subject to CPR.
Research[11] has shown that lay personnel cannot accurately detect a pulse in about 40% of cases and cannot accurately discern the absence of pulse in about 10%. The pulse check step has been removed from the CPR procedure completely for lay persons and de-emphasized for healthcare professionals.
Classification
Prevalence and Effectiveness
Chance of getting CPR
Various studies suggest that in out of home cardiac arrest, bystanders, lay persons or family members attempt CPR in between 14%[17] and 45%[18] of the time, with a median of 32%. This indicates that around 1/3 of out-of-home arrests have a CPR attempt made on them. However, the effectiveness of this CPR is variable, and the studies suggest only around half of bystander CPR is performed correctly.[19][20]
There is a clear correlation between age and the chance of CPR being commenced, with younger people being far more likely to have CPR attempted on them prior to the arrival of emergency medical services.[17][21] It was also found that CPR was more commonly given by a bystander in public, than when an arrest occurred in the patient's home, although health care professionals are responsible for more than half of out-of-hospital resuscitation attempts.[18] This is supported by further research, which suggests that people with no connection to the victim are more likely to perform CPR than a member of their family.[22]
There is also a correlation between the cause of arrest and the likelihood of bystander CPR being initiated. Lay persons are most likely to give CPR to younger cardiac arrest victims in a public place when it has a medical cause; victims in arrest from trauma, exsanguination or intoxication are less likely to receive CPR.[22]
Chance of getting CPR in time
CPR is only likely to be effective if commenced within 6 minutes after the blood flow stops,[23] because permanent brain cell damage occurs when fresh blood infuses the cells after that time, since the cells of the brain become dormant in as little as 4-6 minutes in an oxygen deprived environment and the cells are unable to survive the reintroduction of oxygen in a traditional resuscitation. Research using cardioplegic blood infusion resulted in a 79.4% survival rate with cardiac arrest intervals of 72±43 minutes, traditional methods achieve a 15% survival rate in this scenario, by comparison. New research is currently needed to determine what role CPR, electroshock, and new advanced gradual resuscitation techniques will have with this new knowledge[24] A notable exception is cardiac arrest occurring in conjunction with exposure to very cold temperatures. Hypothermia seems to protect the victim by slowing down metabolic and physiologic processes, greatly decreasing the tissues' need for oxygen.[25] There are cases where CPR, defibrillation, and advanced warming techniques have revived victims after substantial periods of hypothermia.[26]
Chance of surviving
Used alone, CPR will result in few complete recoveries, and those that do survive often develop serious complications. Estimates vary, but many organizations stress that CPR does not "bring anyone back," it simply preserves the body for defibrillation and advanced life support.[27] However, in the case of "non-shockable" rhythms such as Pulseless Electrical Activity (PEA), defibrillation is not indicated, and the importance of CPR rises. On average, only 5%-10% of people who receive CPR survive.[28] The purpose of CPR is not to "start" the heart, but rather to circulate oxygenated blood, and keep the brain alive until advanced care (especially defibrillation) can be initiated. As many of these patients may have a pulse that is impalpable by the layperson rescuer, the current consensus is to perform CPR on a patient that is not breathing. A pulse check is not required in basic CPR since it is so often missed when present, or even felt when absent, even by health care professionals.
Studies have shown the importance of immediate CPR followed by defibrillation within 3–5 minutes of sudden VF cardiac arrest improve survival. In cities such as Seattle where CPR training is widespread and defibrillation by EMS personnel follows quickly, the survival rate is about 30 percent. In cities such as New York City, without those advantages, the survival rate is only 1-2 percent.[29]
Type of Arrest ROSC Survival Source Witnessed In-Hospital Cardiac Arrest 48% 22% [30] Unwitnessed In-Hospital Cardiac Arrest 21% 1% [30] Bystander Cardiocerebral Resuscitation 40% 6% [31] Bystander Cardiopulmonary Resuscitation 40% 4% [31] No Bystander CPR (Ambulance CPR) 15% 2% [31] Defibrillation within 3-5 minutes 74% 30% [27][29]
Chest compression adjuncts
Several different devices have become available in order to help facilitate rescuers in getting the chest compressions completed correctly. These devices can be split in to three broad groups - timing devices, those that assist the rescuer to achieve the correct technique, especially depth and speed of compressions, and those which take over the process completely.
Timing devices
They can feature a metronome (an item carried by many ambulance crews) in order to assist the rescuer in getting the correct rate. The CPR trainer cited here has timed indicators for pressing on the chest, breathing and changing operators.
Manual Assist devices
These items can be devices to placed on top of the chest, with the rescuers hands going over the device, and a display giving information on depth or force.[32] Several published evaluations of one particular product, known as CPREzy, with these features show that the device can improve the performance of chest compressions.[33][34] More recently, these features have also been combined in to a wearable format, as a glove.[35] This glove also has additional features such as a basic electro-cardiogram device. This device was developed by students as part of their thesis, and has been named as one of the top ten inventions of 2007 in Popular Science magazine.[36]
Automatic devices
There are also some devices available which take over the chest compressions for the rescuer. These devices use techniques such as pneumatics to drive a compressing pad on to the chest of the patient. One such device, known as the LUCAS, was developed at Lund University, is powered by the compressed air cylinders or lines available in ambulances or in hospitals, and has undergone numerous clinical trials, showing a marked improvement in coronary perfusion pressure[37] and return of spontaneous circulation.[38]
Another system called the AutoPulse is electrically powered and uses a large band around the patients chest which contracts in rhythm in order to deliver chest compressions. This is also backed by clinical studies showing increased successful return of spontaneous circulation.[39][40]
Alternative Methods
Cardiocerebral Resuscitation
The International Liaison Committee on Resuscitation (ILCOR) approach described above has been challenged in recent years by advocates for Cardiocerebral Resuscitation (CCR). CCR is simply chest compressions without artificial respiration. The ventilation component of CPR has been a topic of major controversy over the past decade.
In March 2007, a Japanese study in the medical journal The Lancet presented strong evidence that compressing the chest, not MTM ventilation, is the key to helping someone recover from cardiac arrest.[41]
The CCR method is championed by the University of Arizona's Sarver Heart Center, and a recent study by the university,[42] claims a 300% greater success rate over standard CPR.[43] The exceptions were in the case of drowning or drug overdose.
The method of delivering chest compressions remains the same, as does the rate (100 per minute), but the rescuer delivers only the compression element which, the University of Arizona claims, keeps the blood flow moving without the interruption caused by insufflations.
An editorial by Gordon Ewy MD (a proponent of CCR) in the same issue of The Lancet calls for an interim revision of the AHA/ILCOR Guidelines based on the results of the Japanese study, but the next scheduled revision of the Guidelines is not until 2010. The initial response of the AHA was that no interim change is necessary.
Rhythmic Abdominal Compressions
Rhythmic abdominal compression-CPR works by forcing blood from the blood vessels around the abdominal organs, an area known to contain about 25 percent of the body's total blood volume. This blood is then redirected to other sites, including the circulation around the heart. Findings published in the September 2007 issue of the American Journal of Emergency Medicine using pigs found that 60 percent more blood was pumped to the heart using rhythmic abdominal compression-CPR than with standard chest compression-CPR, using the same amount of effort. There was no evidence that rhythmic abdominal compressions damaged the abdominal organs and the risk of rib fracture was avoided. Avoiding mouth-to-mouth breathing and chest compressions eliminates the risk of rib fractures and transfer of infection.[44]
Self-CPR
A form of "self-CPR" termed "Cough CPR" may help a person maintain blood flow to the brain during a heart attack while waiting for medical help to arrive and has been used in a hospital emergency room in cases where "standard CPR" was contraindicated.
"Cough CPR" was the subject of a hoax chain e-mail entitled "How to Survive a Heart Attack When Alone" which wrongly cited "ViaHealth Rochester, Rochester General Hospital" as the source of the technique. Rochester General Hospital has denied any connection with the technique.[45][46]
Rapid coughing has been used in hospitals for brief periods of cardiac arrhythmia on monitored patients. One researcher has recommended that it be taught broadly to the public.[47][48]
However, “cough CPR” cannot be used outside the hospital because the first symptom of cardiac arrest is unconsciousness[49] in which case coughing is impossible. Further, the vast majority of people suffering chest pain from a heart attack will not be in cardiac arrest and CPR is not needed. In these cases attempting “cough CPR” will increase the workload on the heart and may be harmful. When coughing is used on trained and monitored patients in hospitals, it has only been shown to be effective for 90 seconds.[50]
The American Heart Association (AHA) and other resuscitation bodies,[51] do not endorse "Cough CPR", which it terms a misnomer as it is not a form of resuscitation. The AHA does recognize a limited legitimate use of the coughing technique:
"This coughing technique to maintain blood flow during brief arrhythmias has been useful in the hospital, particularly during cardiac catheterization. In such cases the patients ECG is monitored continuously, and a physician is present."[52]
Place in film and television
CPR is often severely misrepresented in movies and television as being highly effective in resuscitating a person who is not breathing and has no circulation.
A 1996 study published in the New England Journal of Medicine showed that CPR success rates in television shows was 75%.[53]
It is important to note that CPR techniques portrayed on television and in film are purposely incorrect. Actors performing simulated CPR will keep their elbows bent, to prevent force from reaching the fictional victim's heart. As well as causing significant local trauma, in theory performing CPR on healthy persons may disrupt heart rhythms.
Application on animals
It is entirely feasible to perform CPR on animals like cats and dogs. The principles and practices are virtually identical to CPR for humans. One is cautioned to only perform CPR on unconscious animals to avoid the risk of being bitten.[54]
References
- ↑ 1.0 1.1 "US National Library of Medicine Encyclopedia - Definition of CPR". Retrieved 2007-06-12.
- ↑ "US Red Cross list of courses for all skill levels". Retrieved 2007-06-12.
- ↑ "Resucitation Council UK Comment on Compression Only CPR". Retrieved 2007-06-12.
- ↑ "Silvester's method". University College London. Retrieved 2007-06-12.
- ↑ "Definition of Cardiac Arrest". American Heart Association. Retrieved 2007-06-13.
- ↑ Newsweek 2007-05-07
- ↑ "Chain of Survival Institute". Retrieved 2007-06-12.
- ↑ "British Red Cross Basic First Aid Guidelines". Retrieved 2007-06-12.
- ↑ 9.0 9.1 "Overview of CPR". American Heart Association. Retrieved 2007-06-13.
- ↑ Hughes, Colleen (25th November 2003). "Study finds factors impeding bystander CPR". Annals of Emergency Medicine (December 2003). Retrieved 2007-06-14. Check date values in:
|date=(help) - ↑ 11.0 11.1 "Adult Basic Life Support". American Heart Association. Retrieved 2007-06-13.
- ↑ "Pediatric Basic Life Support". American Heart Association. Retrieved 2007-06-13.
- ↑ "Adult Basic Life Support". American Heart Association. Retrieved 2007-06-13.
- ↑ "Pediatric Basic and Advanced Life Support". American Heart Association. Retrieved 2007-06-13.
- ↑ "Australian Resucitation Council Guidelines as of March 6" (PDF). Retrieved 2007-06-13.
- ↑ "Resucitation Council UK Paediatric Advanced Life Support Guidelines" (PDF). Retrieved 2007-06-13.
- ↑ 17.0 17.1 Swor, RA (June 1995). "Bystander CPR, ventricular fibrillation and survival in witnessed, unmonitored out-of-hospital cardiac arrest". Annals of Emergency Medicine. 25 (6): 780-4. PMID:7755200. Unknown parameter
|couauthors=ignored (help) - ↑ 18.0 18.1 Wik, L (December 1994). "Quality of bystander cardiopulmonary rescucitation influence outcome after prehospital cardiac arrest". Resuscitation. 28 (4): 195–203. PMID: 7740189. Unknown parameter
|coauthors=ignored (help) - ↑ Van Hoeyweghen, RJ (August 1993). "Quality and efficiency of bystander CPR. Belgian Cerebral Resuscitation Study Group". Resuscitation. 26 (1): 47–52. Text "; Calle P; Martens P; Buylaert WA; Delooz H" ignored (help); Unknown parameter
|coauthors=ignored (help) - ↑ Gallagher, EJ (December 1995). "Effectiveness of bystander cardiopulmonary resuscitation and survival following out-of-hospital cardiac arrest". JAMA (24). PMID: 8568985. Unknown parameter
|coauthors=ignored (help); Unknown parameter|Volume=ignored (|volume=suggested) (help) - ↑ jackson, RE (June 1997). "Who gets bystander cardiopulmonary resuscitation in a witnessed arrest?". Academy of Emergency Medicine. 4 (6): 560–4. PMID: 9189184. Unknown parameter
|coauthors=ignored (help) - ↑ 22.0 22.1 Bossaert, L (1989). "Bystander cardiopulmonary resuscitation in out-of-hospital cardiac arrest. The Cerebral Resuscitation study group". Resuscitation. 17 (Suppl S55-69). PMID: 2551021. Unknown parameter
|coauthors=ignored (help) - ↑ Cummins, RO (March 1985). "Survival of out-of-hospital cardiac arrest with early initiation of cardiopulmonary resuscitation". American Journal of Emergency Medicine. 3 (2): 114–9. PMID: 3970766. Unknown parameter
|coauthors=ignored (help) - ↑ Athanasuleas, Constantine (2006). "Sudden cardiac death: directing the scope of resuscitation towards the heart and brain" (PDF). Resuscitation. 70 (1): 44–51. PMID 16759784 Template:ISSN. Retrieved 2007-05-02. Unknown parameter
|coauthors=ignored (help) - ↑ Guilfoy, Christine (18th July 2006). "Heart has enough oxygen to survive hypothermia". American Journal of Physiology - Heart and Circulatory Physiology. Retrieved 2007-06-14. Check date values in:
|date=(help) - ↑ Eich, Christoph (2005). "Recovery of a hypothermic drowned child after resuscitation with cardiopulmonary bypass followed by prolonged extracorporeal membrane oxygenation" (PDF). Resuscitation. 67 (1): 145–8. PMID 16129537 Template:ISSN doi:10.1016/j.resuscitation.2005.05.002. Retrieved 2007-01-29. Unknown parameter
|coauthors=ignored (help) - ↑ 27.0 27.1 "CPR statistics". American Heart Association. Retrieved 2007-06-14.
- ↑ WebMD Medical News. "Real CPR isn't everything it seems to be". Retrieved 2007-06-13.
- ↑ 29.0 29.1 http://www.americanheart.org/presenter.jhtml?identifier=4483
- ↑ 30.0 30.1 Brindley, Peter G (2002-08-20). "Predictors of survival following in-hospital adult cardiopulmonary rescuitation". Canadian Medical Association Journal. 174 (4). Retrieved 2007-06-14. Unknown parameter
|coauthors=ignored (help) - ↑ 31.0 31.1 31.2 "Resucitation Council Comment on CPR study". Resuscitation Council UK. April 2007. Retrieved 2007-06-14.
- ↑ "CPREzy". Retrieved 2007-08-18.
- ↑ Perkins, Gavin D (23rd August 2004). "CPREzy: an evaluation during simulated cardiac arrest on a hospital bed" (PDF). Resuscitation. 64 (2005). Unknown parameter
|coauthors=ignored (help); Check date values in:|date=(help) - ↑ Boyle, Andrew J (March 2002). "CPREzy:an evaluation during simulated cardiac arrest on a hospital bed". Resuscitation. 54 (2002). Unknown parameter
|coauthors=ignored (help) - ↑ "CPR Glove Website". Retrieved 2007-08-18.
- ↑ Rosenwald, Mike. "The glove that saves lives". Popular Science Magazine. Retrieved 2007-08-20.
- ↑ Steen; et al. (2002). "Evaluation of LUCAS, a new device for automated mechanical compression and active decompression". Resuscitation. 55.
- ↑ Rubertsson; et al. (2006). "Increased restoration of spontaneous circulation after cardiac arrest with the LUCAS device compared to manual chest compressions". Resuscitation. 69.
- ↑ Casner, M (Jan–Mar 2005). "The impact of a new CPR assist device on the rate of return of spontaneous circulation in out-of-hospital cardiac arrest". Prehospital Emergency Care. 9 (1). Unknown parameter
|coauthors=ignored (help) - ↑ Hallstrom, Al. "Manual chest compression vs use of an automated chest compression device during resuscitation following out-of-hospital cardiac arrest" (PDF). Journal of the American Medical Association. 295 (22). Unknown parameter
|coauthors=ignored (help) - ↑ DeNoon, Daniel J (2007-03-16). "CPR: Mouth-to-mouth not much help". Retrieved 2007-06-13.
- ↑ "A better sort of CPR". Retrieved 2007-06-16.
- ↑ Ewy, Gordon A (24th November 2004). "A new Cardiopulmonary resuscitation". Circulation. American Heart Association. 111 (2134–2142). Retrieved 2007-06-15. Check date values in:
|date=(help) - ↑ http://www.emsvillage.com/articles/article.cfm?id=2214
- ↑ "ViaHealth Rochester General Hospital statement on 'Cough CPR' email". Retrieved 2007-06-13.
- ↑ "Snopes Urban Legends Reference - Cough CPR". Retrieved 2007-06-13.
- ↑ Rieser M (1992). "The use of cough-CPR in patients with acute myocardial infarction". J Emerg Med. 10 (3): 291–3. PMID 1624741. Unknown parameter
|month=ignored (help) - ↑ Associated Press (October 31, 2003). "Cough may help during heart attack -- Technique may allow patients to stay conscious, study finds".
- ↑ Australian Resuscitation Council Newsletter (2003) Vol. 27 No. 3 p. 2; available at http://www.resus.org.au/newsletters/newsletter_nov_2003.pdf
- ↑ Australian Resuscitation Council Newsletter (2005) Vol. 29 No. 3 p. 2; available at http://www.resus.org.au/newsletters/newsletter_dec2005.pdf
- ↑ Australian Resuscitation Council Newsletter (2005) Vol. 29 No. 3 p. 2; available at http://www.resus.org.au/newsletters/newsletter_dec2005.pdf
- ↑ "Cough CPR". American Heart Association. Retrieved 2007-06-13.
- ↑ "CPR statistics". American Heart Association. Retrieved 2007-06-13.
- ↑ "CPR for Cats & Dogs". University of Washington School of Medicine.
See also
- Basic Life Support (BLS)
- Cardiocerebral Resuscitation (CCR), a similar technique.
- CPR mask
- Resusci Anne
- Face shield
- Advanced cardiac life support
Template:Link FA Template:Link FA ar:انعاش القلب والرئتين bs:Kardiopulmonalna reanimacija ca:Reanimació cardiopulmonar cs:Kardiopulmonální resuscitace de:Herz-Lungen-Wiederbelebung hr:Kardiopulmonalna reanimacija it:Rianimazione cardiopolmonare he:החייאה nl:Reanimatie no:Hjerte-lunge-redning simple:Cardiopulmonary resuscitation sr:Кардиопулмонална реанимација fi:Painelu-puhalluselvytys sv:Hjärt- och lungräddning yi:סי-פי-אר