Cardiac tamponade pathophysiology
|
Cardiac tamponade Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Cardiac tamponade pathophysiology On the Web |
|
American Roentgen Ray Society Images of Cardiac tamponade pathophysiology |
|
Risk calculators and risk factors for Cardiac tamponade pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Varun Kumar, M.B.B.S. Ramyar Ghandriz MD[3]
Overview
Cardiac tamponade occurs when the pericardial space fills up with fluid faster than the pericardial sac can stretch. If the amount of fluid increases slowly (such as in hypothyroidism) the pericardial sac can expand to contain a liter or more of fluid prior to tamponade occurring. If the fluid occurs rapidly (as may occur after trauma or myocardial rupture) as little as 100 ml can cause tamponade.[1]
Pathophysiology
Anatomy and Physiology of Pericardium
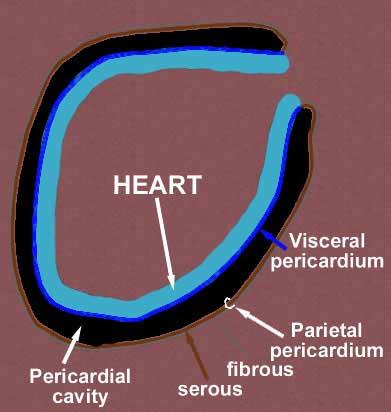
Layers of the Pericardium
- The pericardium is made up of two layers:
- Fibrous pericardium
- Serous pericardium
- Smooth internal layer made up of 2 components:
- Parietal: reflects onto fibrous pericardium
- Visceral: reflects onto heart and great vessels and forms the epicardium, the external layer of the heart wall
- Smooth internal layer made up of 2 components:
- Pericardial cavity: Potential space between parietal and visceral layers. It contains a serous fluid film that occupies the cavity and functions as lubricant against friction by all chest movements.[2][3][4]
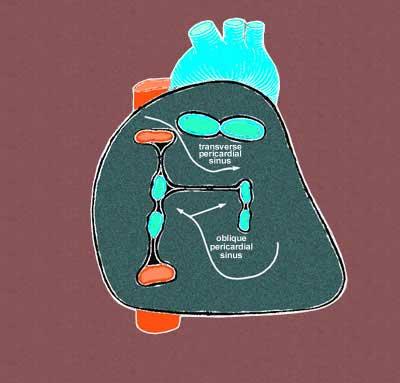
Pericardial Sinuses
- There are two small chambers or sinuses located where the visceral and parietal pericardia are continuous with one another within the pericardial cavity.
- Transverse sinus:
- Located posterior to the pulmonary trunk and ascending aorta at the level between the superior vena cava and aortic arch
- Formed after dorsal mesocardium rupture embryonically
- Functional role is to allow the unhindered expansion of great arteries posteriorly during cardiac systole
- Utilized surgically to pass surgical clamps or place ligatures around great arteries.
- Oblique sinus:
- A blind recess (cul-de-sac) posterior to the left atrium between superior vena cava, right and left pulmonary veins inferior to the transverse sinus
- Formed embryonically by the incorporation of the pulmonary vein tributaries into the left atrium
- Functional role believed to be the expansion of the left atrium upon the normal collapse of the thorax[5][6][7]
Pathogenesis
The outer pericardium is made of fibrous tissue [8] which does not easily stretch, and so once fluid begins to enter the pericardial space, pressure starts to increase [9].
Ordinarily, drainage from the pericardium occurs via the thoracic duct and the right lymphatic duct into the right pleural space. In the absence of disease, the normal pericardium contains only 20-50 cc of serous fluid due to ultrafiltration from the blood. Up to about 75 cc can accumulate acutely in the pericardium without hemodynamic compromise. Much greater amounts of fluid can accumulate chronically over a prolonged period of time as the pericardial sac stretches slowly to accommodate the fluid without hemodynamic compromise. However, if the volume of the fluid accumulation is too rapid and or large, then the hemodynamic compromise can occur with a rise in pericardial pressure. This in turn reduces stroke volume, and eventually, cardiac output.
If fluid continues to accumulate, then with each successive diastole, less and less blood enters the ventricles, as the increasing pressure presses on the heart and forces the septum to bend into the left ventricle, leading to a decreased stroke volume [10]. This causes obstructive shock to develop, and if left untreated, cardiac arrest may occur (in which case the presenting rhythm is likely to be Pulseless electrical activity).
Below is a video demonstrating hemorrhagic effusion leading to cardiac tamponade. {{#ev:youtube|QwgfuDegC5Y}}
Gross Pathology
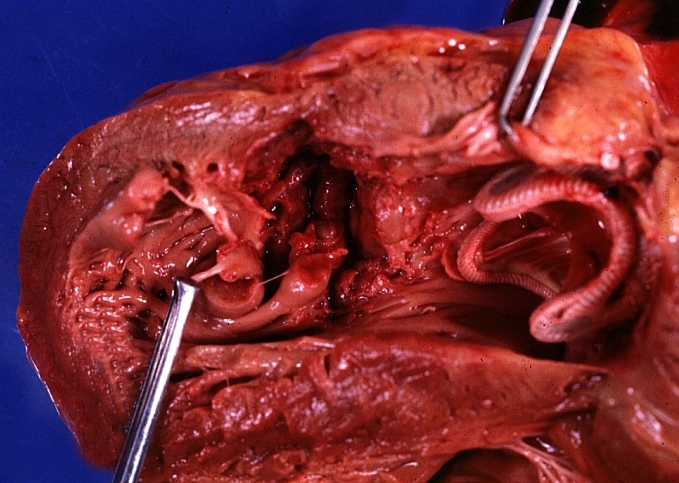
-
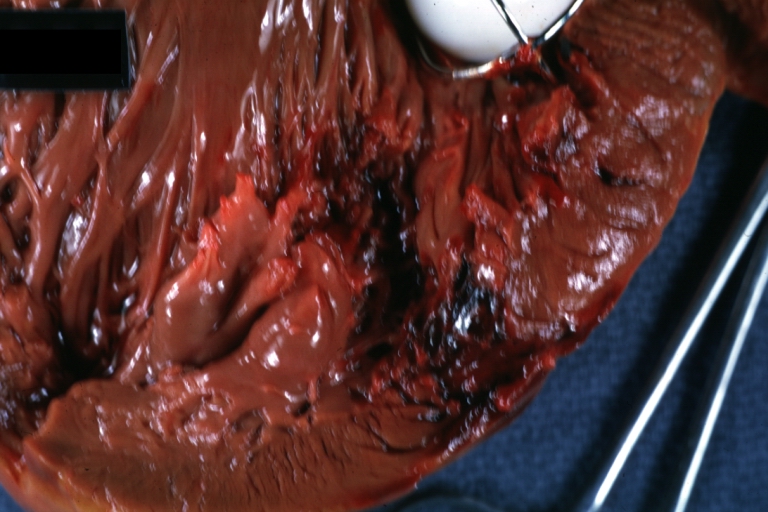
HEART: Myocardial Rupture Following Mitral Valve Replacement: Gross, an excellent example with valve and obviously ruptured heart wall.
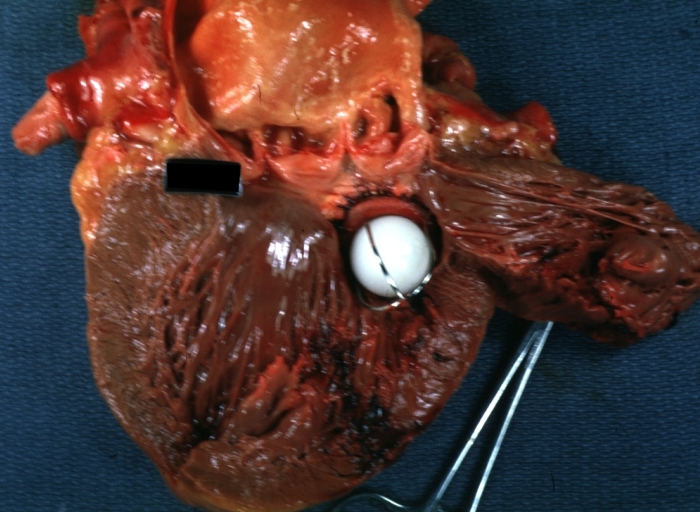
-
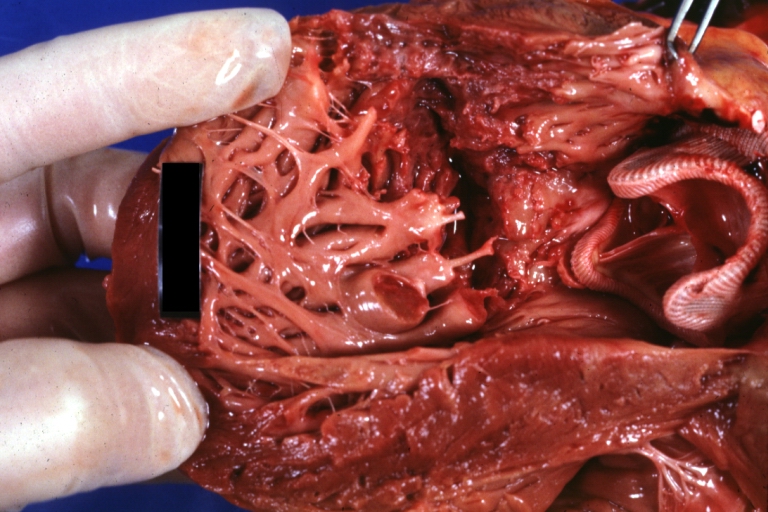
HEART: Myocardial Rupture Following Mitral Valve Replacement: Gross, natural color view from within left ventricle caged plastic ball with steel complete struts
-
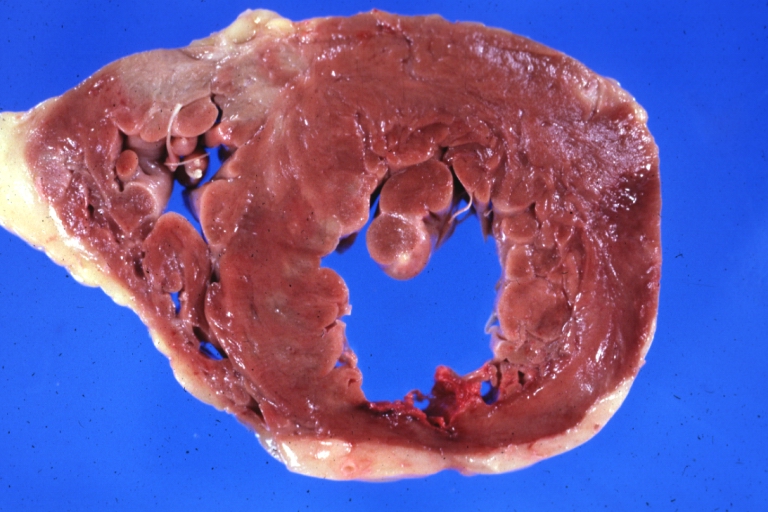
HEART: Myocardial Rupture Following Mitral Valve Replacement: Gross, natural color portion of caged plastic ball prosthesis shown with close-up of ruptured left ventricular wall
-
HEART: Myocardial Rupture Following Mitral Valve Replacement: Gross, natural color close-up view of torn myocardium and bottom of hetero or homograft valve
-
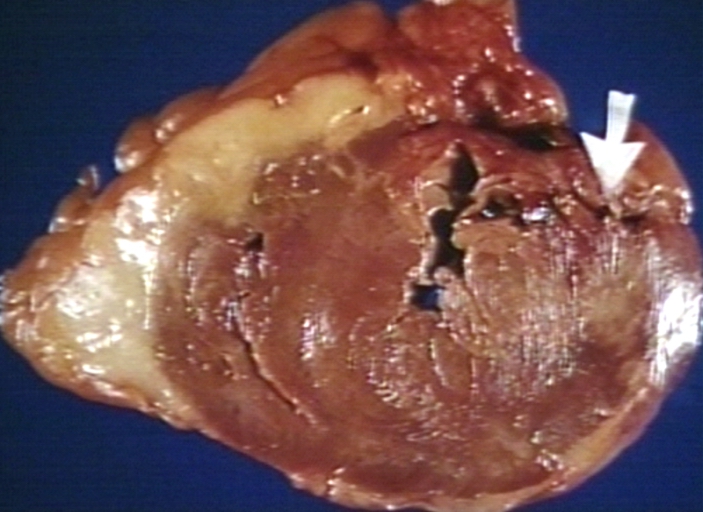
HEART: Infarct; Acute, Ruptured: Gross, natural color horizontal section ventricle anterior infarct not easily appreciated with thinning of myocardium
-
HEART: Rupture after myocardial infarction.
References
- ↑ *Fornauer, Andrew (2003). "Pericardial Tamponade Complicating Central Venous Interventions". Journal of Vascular and Interventional Radiology. PMID 12582195. Unknown parameter
|coauthors=ignored (help); Unknown parameter|month=ignored (help) - ↑ Kishore, K. (2003). The Heart of Structural Development: The Functional Basis of the Location and Morphology of the Human Vascular Pump. J Postgrad Med, 49:282-4.
- ↑ Moore, K. L., Agur, A. M., & Dalley, A. F. (2011). Essential Clinical Anatomy - Fourth Edition. Lippincott Williams & Wilkins.
- ↑ Tank, P. W. (2009). Grant's Dissector - Fourteenth Edition. Lippincott Williams & Wilkins.
- ↑ Kishore, K. (2003). The Heart of Structural Development: The Functional Basis of the Location and Morphology of the Human Vascular Pump. J Postgrad Med, 49:282-4.
- ↑ Moore, K. L., Agur, A. M., & Dalley, A. F. (2011). Essential Clinical Anatomy - Fourth Edition. Lippincott Williams & Wilkins.
- ↑ Tank, P. W. (2009). Grant's Dissector - Fourteenth Edition. Lippincott Williams & Wilkins.
- ↑ Thibodeau, G.A., Patton, K.T. (2000). Anatomy & Physiology. Missouri: Mosby ISBN 9780323010962
- ↑ Mattson Porth, C. (Ed.) (2005) (7th Ed.) Pathophysiology: Concepts of Altered Health States. Philadelphia : Lippincott Williams & Wilkins ISBN 978-0781749886
- ↑ Mattson Porth, C. (Ed.) (2005) (7th Ed.) Pathophysiology: Concepts of Altered Health States. Philadelphia : Lippincott Williams & Wilkins ISBN 978-0781749886