COVID-19-associated meningitis
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Wajeeha Aiman, M.D.[2], Muhammad Adnan Haider, M.B.B.S.[3]
Synonyms and keywords:
Overview
In December of 2019, unknown cases of pneumonia began to spread in the Wuhan city of China. A Novel coronavirus was isolated from these cases and was later named as severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) in early January 2020. SARS-CoV-2 seems to be partially similar to severe acute respiratory syndrome coronavirus (SARS) and Middle East respiratory syndrome coronavirus (MERS). The SARS-CoV-2 is a positive-strand RNA virus belonging to the Orthocoronavirinae subfamily. The pneumonia disease caused by SARS-CoV-2 was named COVID-19 by WHO. COVID-19 was declared a pandemic by WHO on March 11, 2020. To date, around 10 million people have been infected by SARS-COV-2 in more than 215 countries and more than half a million people have been killed by the COVID-19. These numbers are increasing daily. The main mode of transmission for SARS-CoV-2 from person to person is through respiratory droplets. It can be identified in the samples of sputum, nasal and pharyngeal swabs, bronchoalveolar fluid, blood and faeces, suggesting faecal-oral transmission could be a possible route. COVID-19 has a wide range of clinical manifestations. The clinical symptoms of COVID-19 are predominantly of respiratory. The patient may be asymptomatic or can present with fever, cough, sore throat, fatigue and dyspnea. Majority of COVID-19 cases have been recognized as mild, but severe cases leading to respiratory failure, septic shock, and/or multiple organ dysfunction have also been identified. Although rare but spectrum of neurological manifestations have been reported throughout the pandemic. These neurological presentations range from headache, anosmia, encephalitis, meningitis, Guillain Barre syndrome and stroke. Meningitis is the inflammation of the coverings of the brain and spinal cord.
Historical Perspective
- Neurological symptoms in Coronavirus disease 2019 (COVID-19) patients were first reported in February 2020 in a retrospective case series study by Mao L. et al. in hospitalized COVID-19 patients in Wuhan. Ling Mao from Tongji Medical College in Wuhan, and his group reviewed the data retrospectively from January 16, 2020, to February 19, 2020. One third of the 214 hospitalized laboratory- confirmed COVID-19 patients included in this study reported at least one neurologic symptom.
- Covid-19 associated meningitis/encephalitis was first discovered by Moriguchi T. et al. a Japanese critical care physician in late February 2020 during the pandemic of SARS-Coronavirus-2: SARS-CoV-2 [1].
- Duong L et. reported a case of a young female with COVID-19 who developed meningoencephalitis without respiratory failure in Downtown Los Angeles in early April, 2020 [2].
- Bernard-Valnet R et al. reported two cases of meningoencephalitis in patients with concomitant SARS-CoV-2 infection [3]
Classification
There is no established system for the classification of SARS-CoV-2 related meningitis.
Pathophysiology
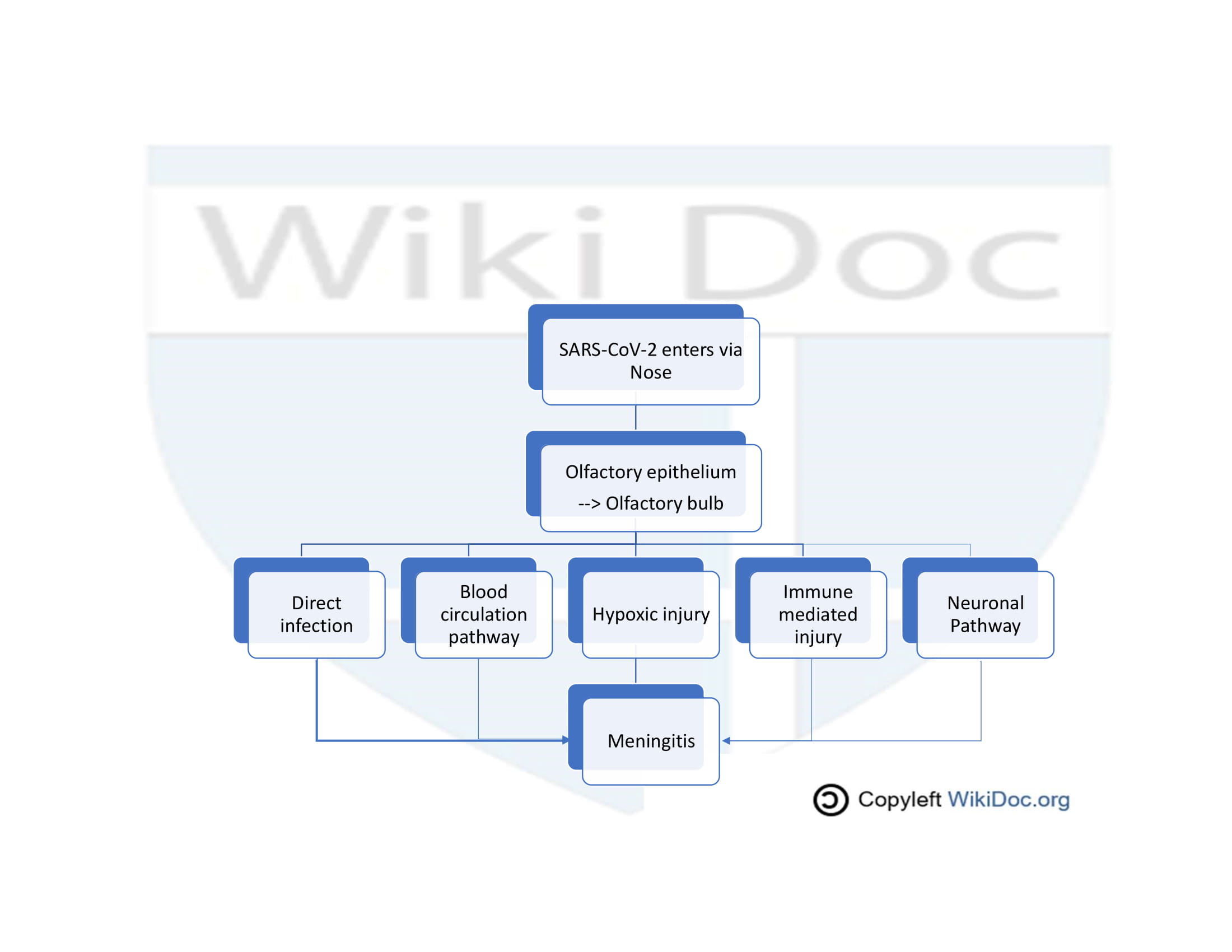
The exact pathogenesis of SARS-CoV-2 associated meningitis is not fully understood.
- Severe acute respiratory syndrome (SARS) and Middle East respiratory Syndrome (MERS) caused some neurological manifestations in 2002 and 2012 respectively[4]. As neucleic acid of SARS-CoV and MERS-CoV was found in cerebrospinal fluid and later on the autopsy of brain[5].
- SARS-CoV-2 is 79% identical to SARS-CoV and 50% to MERS-CoV[6]. Due to structural homology it is safe to say that SARS-CoV-2 causes neurological problems by the same mechanism as caused by SARS-CoV and MERS-CoV.
The proposed pathophysiology of SARS-CoV-2 associated meningitis is by following three mechanisms;
1.Direct pathway
SARS-CoV-2 directly reaches brain through cribriform plate which is located in close proximity to olfactory bulb[7]. This is supported by the facts that some patients of COVID-19 present with anosmia and hyposmia.
2. Blood circulation pathway
- Angiotensin converting enzyme-2 (ACE2) is the functional receptor of the SARS-CoV-2[8]. ACE2 is expressed on glial tissue, neurons and brain vasculature[9]
- SARS-CoV-2 binds with ACE2 precsent on vascular endothelial cells and glial tissues with the help of spike S protein.[10]
- Subsequent viral budding from endothelial cells and resultant damage to capillary endothelium favors viral entry into milieu of brain[11].
- Viral interaction with ACE2 expressed on neurons lead to damage to neurons and inflamation (encephalitis) and inflammation of brain membranes (meningitis)
3. Neuronal Pathway
- SARS-CoV-2 can reach brain via anterograde or retrograde transoport with the help of motor proteins kinesin and dynein via sensory nerve endings, especially afferent nerve endings of vagus nerve from lungs.[12]
- SARS-CoV-2 causes some gastrointestinal problems in COVID-19 patients and can reach CNS from enteric nerve and sympathetic afferent via neuronal pathway.[13]
- Exosomal cellular transport is also a pathway for SARS-CoV-2 systemic dissemination and spread to CNS.[14]
Causes
Meningitis in COVID-19 patients is caused by SARS-CoV-2 virus.
Differentiating COVID-19-associated meningitis from other Diseases
[Disease name] must be differentiated from other diseases that cause [clinical feature 1], [clinical feature 2], and [clinical feature 3], such as [differential dx1], [differential dx2], and [differential dx3].
OR
[Disease name] must be differentiated from [[differential dx1], [differential dx2], and [differential dx3].
Epidemiology and Demographics
The incidence/prevalence of [disease name] is approximately [number range] per 100,000 individuals worldwide.
OR
In [year], the incidence/prevalence of [disease name] was estimated to be [number range] cases per 100,000 individuals worldwide.
OR
In [year], the incidence of [disease name] is approximately [number range] per 100,000 individuals with a case-fatality rate of [number range]%.
Patients of all age groups may develop [disease name].
OR
The incidence of [disease name] increases with age; the median age at diagnosis is [#] years.
OR
[Disease name] commonly affects individuals younger than/older than [number of years] years of age.
OR
[Chronic disease name] is usually first diagnosed among [age group].
OR
[Acute disease name] commonly affects [age group].
There is no racial predilection to [disease name].
OR
[Disease name] usually affects individuals of the [race 1] race. [Race 2] individuals are less likely to develop [disease name].
[Disease name] affects men and women equally.
OR
[Gender 1] are more commonly affected by [disease name] than [gender 2]. The [gender 1] to [gender 2] ratio is approximately [number > 1] to 1.
The majority of [disease name] cases are reported in [geographical region].
OR
[Disease name] is a common/rare disease that tends to affect [patient population 1] and [patient population 2].
Risk Factors
There are no established risk factors for [disease name].
OR
The most potent risk factor in the development of [disease name] is [risk factor 1]. Other risk factors include [risk factor 2], [risk factor 3], and [risk factor 4].
OR
Common risk factors in the development of [disease name] include [risk factor 1], [risk factor 2], [risk factor 3], and [risk factor 4].
OR
Common risk factors in the development of [disease name] may be occupational, environmental, genetic, and viral.
Screening
There is insufficient evidence to recommend routine screening for [disease/malignancy].
OR
According to the [guideline name], screening for [disease name] is not recommended.
OR
According to the [guideline name], screening for [disease name] by [test 1] is recommended every [duration] among patients with [condition 1], [condition 2], and [condition 3].
Natural History, Complications, and Prognosis
If left untreated, [#]% of patients with [disease name] may progress to develop [manifestation 1], [manifestation 2], and [manifestation 3].
OR
Common complications of [disease name] include [complication 1], [complication 2], and [complication 3].
OR
Prognosis is generally excellent/good/poor, and the 1/5/10-year mortality/survival rate of patients with [disease name] is approximately [#]%.
Diagnosis
Diagnostic Study of Choice
The diagnostic study of choice for meningitis present in COVID-19 patients is CSF analysis with ruling out other viral panels (HSV-1 and VZV) with the help of RT-PCR. In some health facilities RT-PCR testing for SARS-CoV-2 is being done but still it is not FDA approved.
History and Symptoms
Four cases of meningitis in COVID-19 patients have been reported. The disease course of these patients is given in the table.
| Patient no. | Early symptoms | Late symptoms | CSF analysis | Viral panel | SARS-CoV-2 analysis |
|---|---|---|---|---|---|
Physical Examination
Patients with [disease name] usually appear [general appearance]. Physical examination of patients with [disease name] is usually remarkable for [finding 1], [finding 2], and [finding 3].
OR
Common physical examination findings of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
The presence of [finding(s)] on physical examination is diagnostic of [disease name].
OR
The presence of [finding(s)] on physical examination is highly suggestive of [disease name].
Laboratory Findings
An elevated/reduced concentration of serum/blood/urinary/CSF/other [lab test] is diagnostic of [disease name].
OR
Laboratory findings consistent with the diagnosis of [disease name] include [abnormal test 1], [abnormal test 2], and [abnormal test 3].
OR
[Test] is usually normal among patients with [disease name].
OR
Some patients with [disease name] may have elevated/reduced concentration of [test], which is usually suggestive of [progression/complication].
OR
There are no diagnostic laboratory findings associated with [disease name].
Electrocardiogram
There are no ECG findings associated with [disease name].
OR
An ECG may be helpful in the diagnosis of [disease name]. Findings on an ECG suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
X-ray
There are no x-ray findings associated with [disease name].
OR
An x-ray may be helpful in the diagnosis of [disease name]. Findings on an x-ray suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no x-ray findings associated with [disease name]. However, an x-ray may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
Echocardiography or Ultrasound
There are no echocardiography/ultrasound findings associated with [disease name].
OR
Echocardiography/ultrasound may be helpful in the diagnosis of [disease name]. Findings on an echocardiography/ultrasound suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no echocardiography/ultrasound findings associated with [disease name]. However, an echocardiography/ultrasound may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
CT scan
There are no CT scan findings associated with [disease name].
OR
[Location] CT scan may be helpful in the diagnosis of [disease name]. Findings on CT scan suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no CT scan findings associated with [disease name]. However, a CT scan may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
MRI
There are no MRI findings associated with [disease name].
OR
[Location] MRI may be helpful in the diagnosis of [disease name]. Findings on MRI suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no MRI findings associated with [disease name]. However, a MRI may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
Other Imaging Findings
There are no other imaging findings associated with [disease name].
OR
[Imaging modality] may be helpful in the diagnosis of [disease name]. Findings on an [imaging modality] suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
Other Diagnostic Studies
There are no other diagnostic studies associated with [disease name].
OR
[Diagnostic study] may be helpful in the diagnosis of [disease name]. Findings suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
Other diagnostic studies for [disease name] include [diagnostic study 1], which demonstrates [finding 1], [finding 2], and [finding 3], and [diagnostic study 2], which demonstrates [finding 1], [finding 2], and [finding 3].
Treatment
Medical Therapy
There is no treatment for [disease name]; the mainstay of therapy is supportive care.
OR
Supportive therapy for [disease name] includes [therapy 1], [therapy 2], and [therapy 3].
OR
The majority of cases of [disease name] are self-limited and require only supportive care.
OR
[Disease name] is a medical emergency and requires prompt treatment.
OR
The mainstay of treatment for [disease name] is [therapy].
OR
The optimal therapy for [malignancy name] depends on the stage at diagnosis.
OR
[Therapy] is recommended among all patients who develop [disease name].
OR
Pharmacologic medical therapy is recommended among patients with [disease subclass 1], [disease subclass 2], and [disease subclass 3].
OR
Pharmacologic medical therapies for [disease name] include (either) [therapy 1], [therapy 2], and/or [therapy 3].
OR
Empiric therapy for [disease name] depends on [disease factor 1] and [disease factor 2].
OR
Patients with [disease subclass 1] are treated with [therapy 1], whereas patients with [disease subclass 2] are treated with [therapy 2].
Surgery
Surgical intervention is not recommended for the management of [disease name].
OR
Surgery is not the first-line treatment option for patients with [disease name]. Surgery is usually reserved for patients with either [indication 1], [indication 2], and [indication 3]
OR
The mainstay of treatment for [disease name] is medical therapy. Surgery is usually reserved for patients with either [indication 1], [indication 2], and/or [indication 3].
OR
The feasibility of surgery depends on the stage of [malignancy] at diagnosis.
OR
Surgery is the mainstay of treatment for [disease or malignancy].
Primary Prevention
There are no established measures for the primary prevention of [disease name].
OR
There are no available vaccines against [disease name].
OR
Effective measures for the primary prevention of [disease name] include [measure1], [measure2], and [measure3].
OR
[Vaccine name] vaccine is recommended for [patient population] to prevent [disease name]. Other primary prevention strategies include [strategy 1], [strategy 2], and [strategy 3].
Secondary Prevention
There are no established measures for the secondary prevention of [disease name].
OR
Effective measures for the secondary prevention of [disease name] include [strategy 1], [strategy 2], and [strategy 3].
References
- ↑ Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J; et al. (2020). "A first case of meningitis/encephalitis associated with SARS-Coronavirus-2". Int J Infect Dis. 94: 55–58. doi:10.1016/j.ijid.2020.03.062. PMC 7195378 Check
|pmc=value (help). PMID 32251791 Check|pmid=value (help). - ↑ Duong L, Xu P, Liu A (2020). "Meningoencephalitis without respiratory failure in a young female patient with COVID-19 infection in Downtown Los Angeles, early April 2020". Brain Behav Immun. 87: 33. doi:10.1016/j.bbi.2020.04.024. PMC 7162766 Check
|pmc=value (help). PMID 32305574 Check|pmid=value (help). - ↑ Bernard-Valnet R, Pizzarotti B, Anichini A, Demars Y, Russo E, Schmidhauser M; et al. (2020). "Two patients with acute meningoencephalitis concomitant with SARS-CoV-2 infection". Eur J Neurol. doi:10.1111/ene.14298. PMC 7267660 Check
|pmc=value (help). PMID 32383343 Check|pmid=value (help). - ↑ Tsai LK, Hsieh ST, Chang YC (2005). "Neurological manifestations in severe acute respiratory syndrome". Acta Neurol Taiwan. 14 (3): 113–9. PMID 16252612.
- ↑ Schoeman D, Fielding BC (2019). "Coronavirus envelope protein: current knowledge". Virol J. 16 (1): 69. doi:10.1186/s12985-019-1182-0. PMC 6537279 Check
|pmc=value (help). PMID 31133031. - ↑ Lu R, Zhao X, Li J, Niu P, Yang B, Wu H; et al. (2020). "Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding". Lancet. 395 (10224): 565–574. doi:10.1016/S0140-6736(20)30251-8. PMC 7159086 Check
|pmc=value (help). PMID 32007145 Check|pmid=value (help). - ↑ Baig AM, Khaleeq A, Ali U, Syeda H (2020). "Evidence of the COVID-19 Virus Targeting the CNS: Tissue Distribution, Host-Virus Interaction, and Proposed Neurotropic Mechanisms". ACS Chem Neurosci. 11 (7): 995–998. doi:10.1021/acschemneuro.0c00122. PMC 7094171 Check
|pmc=value (help). PMID 32167747 Check|pmid=value (help). - ↑ Ge XY, Li JL, Yang XL, Chmura AA, Zhu G, Epstein JH; et al. (2013). "Isolation and characterization of a bat SARS-like coronavirus that uses the ACE2 receptor". Nature. 503 (7477): 535–8. doi:10.1038/nature12711. PMC 5389864. PMID 24172901.
- ↑ Turner AJ, Hiscox JA, Hooper NM (2004). "ACE2: from vasopeptidase to SARS virus receptor". Trends Pharmacol Sci. 25 (6): 291–4. doi:10.1016/j.tips.2004.04.001. PMC 7119032 Check
|pmc=value (help). PMID 15165741. - ↑ Wrapp D, Wang N, Corbett KS, Goldsmith JA, Hsieh CL, Abiona O; et al. (2020). "Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation". Science. 367 (6483): 1260–1263. doi:10.1126/science.abb2507. PMC 7164637 Check
|pmc=value (help). PMID 32075877 Check|pmid=value (help). - ↑ Baig AM, Khaleeq A, Ali U, Syeda H (2020). "Evidence of the COVID-19 Virus Targeting the CNS: Tissue Distribution, Host-Virus Interaction, and Proposed Neurotropic Mechanisms". ACS Chem Neurosci. 11 (7): 995–998. doi:10.1021/acschemneuro.0c00122. PMC 7094171 Check
|pmc=value (help). PMID 32167747 Check|pmid=value (help). - ↑ Swanson PA, McGavern DB (2015). "Viral diseases of the central nervous system". Curr Opin Virol. 11: 44–54. doi:10.1016/j.coviro.2014.12.009. PMC 4456224. PMID 25681709.
- ↑ Wong SH, Lui RN, Sung JJ (2020). "Covid-19 and the digestive system". J Gastroenterol Hepatol. 35 (5): 744–748. doi:10.1111/jgh.15047. PMID 32215956 Check
|pmid=value (help). - ↑ Alenquer M, Amorim MJ (2015). "Exosome Biogenesis, Regulation, and Function in Viral Infection". Viruses. 7 (9): 5066–83. doi:10.3390/v7092862. PMC 4584306. PMID 26393640.