COVID-19-associated abdominal pain: Difference between revisions
(Created page with "__NOTOC__ {{SI}} {{CMG}} ==Overview== ==Historical Perspective== *[Disease name] was first discovered by [...") |
No edit summary |
||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
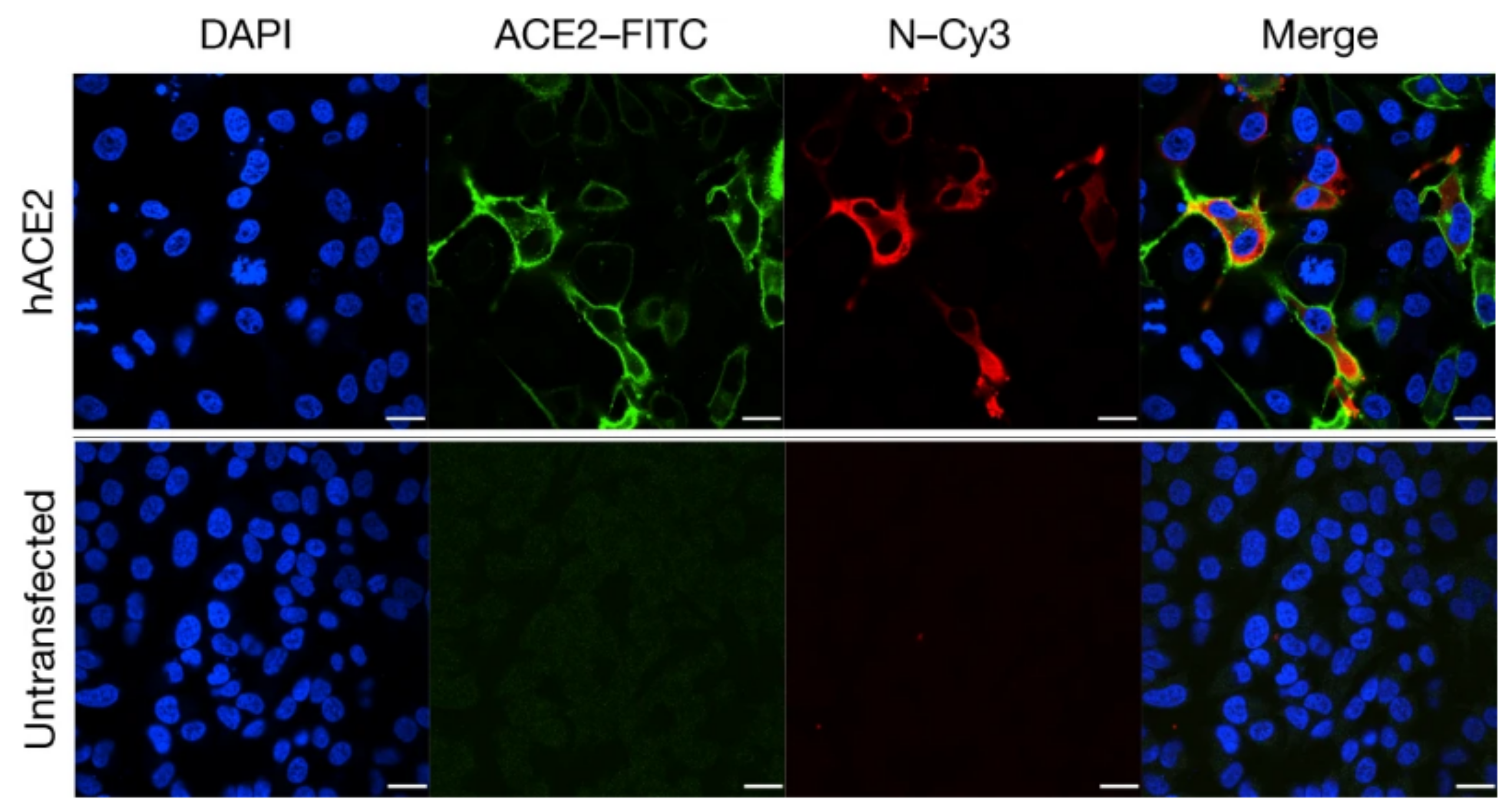
{{SI}} | [[File:HeLa cell with ACE2 receptor SARS-COV-2.png|thumb|right|500px|Transfection of HeLa cells with the ACE2 receptor makes them susceptible to SARS-CoV-2 infection. hACE2, human ACE2;<span style="color: green">green<span style="color: black">, ACE2;<span style="color: red">red<span style="color: black">, viral protein (N);<span style="color: blue">blue<span style="color: black">, DAPI (nuclei). Scale bars, 10 μm-By Peng Zhou et al - https://www.nature.com/articles/s41586-020-2012-7, CC BY 4.0, https://commons.wikimedia.org/w/index.php?curid=91229428.jpg]] | ||
{{CMG}} | {{SI}} | ||
{{CMG}}; {{AE}} [[User:Javaria Anwer|Javaria Anwer M.D.]][mailto:javaria.anwer@gmail.com] | |||
{{SK}} [[COVID-19 associated abdominal pain]], [[COVID associated abdominal pain]], [[COVID likned abdominal pain]], [[COVID-19 linked abdominal pain]], [[coronavirus associated abdominal pain]], [[coronavirus related belly pain]], [[abdominal pain associated with COVID-19]], [[abdominal pain associated with SARS CoV2]], [[SARS CoV2 related abdominal pain]], [[SARS CoV2 linked abdomin pain]], [[abdominal pain and COVID-19]], [[abdominal pain and SARS CoV2]] ,[[abdominal pain in COVID]], [[abdomin pain in COVID]], [[abdominal pain in nCoV]], [[abdominal discomfort in COVID-19]], [[abdominal discomfort in SARS CoV2]] | |||
==Overview== | ==Overview== | ||
Abdominal pain is a vast entity and sometimes a challenge due to its various potential diagnoses. Although [[COVID-19]] is mainly a respiratory disease, abdominal pain is one of the symptoms of [[COVID-19]] infection. | |||
==Historical Perspective== | ==Historical Perspective== | ||
*[ | *A cluster of cases of [[pneumonia]] in Wuhan, China was first reported on December 31st, 2019 by Wuhan Municipal Health Commission, China. A novel coronavirus was eventually identified. The first disease [[outbreak]] news on the new virus was first published by [[WHO]] on 5th January 2020.<ref name="urlWHO Timeline - COVID-19">{{cite web |url=https://www.who.int/news-room/detail/27-04-2020-who-timeline---covid-19?gclid=EAIaIQobChMIpYj3w_qi6gIVi8myCh04KgZ6EAAYASAAEgJ0yvD_BwE |title=WHO Timeline - COVID-19 |format= |work= |accessdate=}}</ref> | ||
* | *On March 12, 2020, [[WHO]] declared the COVID-19 outbreak a [[pandemic]]. | ||
*In [ | *Initially [[COVID-19]] was primarily known as a respiratory disease. In the initial phase of the [[pandemic]], the [[screening]] criteria for [[COVID‐19]] did not include [[symptoms]] of abdominal pain. | ||
*On Feb 3rd, 2020, a study published by Wang D et al. first described abdominal pain as one of the less common symptoms of [[COVID-19]].<ref name="WangHu2020">{{cite journal|last1=Wang|first1=Dawei|last2=Hu|first2=Bo|last3=Hu|first3=Chang|last4=Zhu|first4=Fangfang|last5=Liu|first5=Xing|last6=Zhang|first6=Jing|last7=Wang|first7=Binbin|last8=Xiang|first8=Hui|last9=Cheng|first9=Zhenshun|last10=Xiong|first10=Yong|last11=Zhao|first11=Yan|last12=Li|first12=Yirong|last13=Wang|first13=Xinghuan|last14=Peng|first14=Zhiyong|title=Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China|journal=JAMA|volume=323|issue=11|year=2020|pages=1061|issn=0098-7484|doi=10.1001/jama.2020.1585}}</ref> | |||
== | *With the increasing evidence and ongoing research, abdominal pain is now reported to be a common symptom in patients with [[COVID-19]], and the viral infection is suspected in a patient presenting with [[abdominal pain]]. Research is underway to develop a better understanding of the etiology, risk factors, and treatment of [[abdominal pain]] associated with [[COVID-19]]. | ||
*[ | |||
==Pathophysiology== | ==Pathophysiology== | ||
* | *[[Angiotensin-converting enzyme|ACE 2]] acts as the [[COVID-19|SARS-CoV2]] receptor for [[infectivity]] and the entrance into the cell. Research has shown [[Angiotensin-converting enzyme|ACE 2]] receptors in [[esophagus|esophageal]] [[epithelium|epithelial cells]], [[ileum|ileal]] and [[colon]] [[ enterocytes]] making them vulnerable to [[COVID-19]] infection. The detection of viral [[nucleocapsid]] protein in gastrointestinal [[epithelial cells]] and viral RNA in [[fecal]] [[specimens]] reflects the infectivity and chance of direct viral damage of organs.<ref name="ZouChen2020">{{cite journal|last1=Zou|first1=Xin|last2=Chen|first2=Ke|last3=Zou|first3=Jiawei|last4=Han|first4=Peiyi|last5=Hao|first5=Jie|last6=Han|first6=Zeguang|title=Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection|journal=Frontiers of Medicine|volume=14|issue=2|year=2020|pages=185–192|issn=2095-0217|doi=10.1007/s11684-020-0754-0}}</ref><ref name="pmid32222988">{{cite journal |vauthors=Tian Y, Rong L, Nian W, He Y |title=Review article: gastrointestinal features in COVID-19 and the possibility of faecal transmission |journal=Aliment. Pharmacol. Ther. |volume=51 |issue=9 |pages=843–851 |date=May 2020 |pmid=32222988 |pmc=7161803 |doi=10.1111/apt.15731 |url=}}</ref><ref name="pmid32264791">{{cite journal |vauthors=Gheblawi M, Wang K, Viveiros A, Nguyen Q, Zhong JC, Turner AJ, Raizada MK, Grant MB, Oudit GY |title=Angiotensin-Converting Enzyme 2: SARS-CoV-2 Receptor and Regulator of the Renin-Angiotensin System: Celebrating the 20th Anniversary of the Discovery of ACE2 |journal=Circ. Res. |volume=126 |issue=10 |pages=1456–1474 |date=May 2020 |pmid=32264791 |pmc=7188049 |doi=10.1161/CIRCRESAHA.120.317015 |url=}} | ||
</ref> The entry of the virus causes disruption of the [[enterocytes]] and may lead to [[inflammation]], impaired cell permeability, and cellular damage. | |||
* The abdominal pain can be due to direct viral infection of the [[gastrointestinal tract]] via cellular [[angiotensin converting enzyme| ACE 2]] receptors in several abdominal organs, making them susceptible to viral infection. | |||
==Clinical Features== | ==Clinical Features== | ||
==Differentiating [ | ==Differentiating abdominal pain due to [[COVID-19]] from other Diseases== | ||
*[ | *If the patient complains of [[diarrhea ]] and abdominal pain stool test for bacterial, viral, and treatment-related causes of diarrhea. [[Clostridium difficile]] and other enteric pathogens can help differentiate alternate causes. | ||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
* | * Based upon the meta-analysis including 78 studies the Weighted Pooled Prevalence (WPP) of abdominal pain associated with [[COVID-19]] is approximately 6.2% (2.6%-10.3%). Although the data comes from four studies, the WPP of abdominal pain at illness onset was 4.1% and at admission was 7.3%.<ref name="TariqSaha2020">{{cite journal|last1=Tariq|first1=Raseen|last2=Saha|first2=Srishti|last3=Furqan|first3=Fateeha|last4=Hassett|first4=Leslie|last5=Pardi|first5=Darrell|last6=Khanna|first6=Sahil|title=Prevalence and Mortality of COVID-19 patients with Gastrointestinal Symptoms: A Systematic Review and Meta-analysis|journal=Mayo Clinic Proceedings|year=2020|issn=00256196|doi=10.1016/j.mayocp.2020.06.003}}</ref> | ||
*'''Age''': Very limited data is available about the detailed demographics of the patients having abdominal pain as one of the symptoms of [[COVID-19]] infection. A study reporting 10 cases presenting with abdominal pain as one of the symptoms showed the mean age of 50±18 years. | |||
*'''Race''': Data from 12797 patients showed a higher weighted pooled prevalence of abdominal pain associated with [[COVID-19]] in the non-Chinese subgroup. | |||
=== | |||
=== | |||
=== | |||
* | |||
*[ | |||
==Risk Factors== | ==Risk Factors== | ||
* | *The main risk factor for the development of the disease is [[COVID-19]] infection. | ||
*The incidence of abdominal pain and diarrhea was higher in patients with severe [[COVID-19]] | |||
== Natural History, Complications and Prognosis== | == Natural History, Complications and Prognosis== | ||
*The majority of patients with | *The majority of patients with abdominal pain | ||
*If left untreated, | |||
*If left untreated, | *Common complications | ||
*Common complications | *Prognosis is generally good. | ||
*Prognosis is generally | |||
== Diagnosis == | == Diagnosis == | ||
===Diagnostic Criteria=== | ===Diagnostic Criteria=== | ||
* | *There are no established diagnostic criteria to identify the cause of abdominal pain in [[COVID-19|SARS-CoV2]] patient. Abdominal [[ultrasound]] or [[CT scan]], and blood tests showing deranged liver functions can give a clue of possible gastrointestinal involvement. | ||
=== History and Symptoms === | |||
*The patient may have abdominal pain as an accompanying symptom along with other [[COVID-19|SARS-CoV2]] infection symptoms such as anorexia, fever, cough, and malaise. Very few patients present with abdominal pain as the sole symptom and high suspicion is required in order to reach the diagnosis. | |||
=== Symptoms === | |||
* | |||
=== Physical Examination === | === Physical Examination === | ||
*Patients with [ | *Patients with abdominal pain associated with [[COVID-19]] can be in distress due to their general condition or the severity of abdominal pain. A person with [[pancreatitis]] will appear [[dehydrated]], [[lethargic]] and in severe pain. | ||
* | *PThe patient can be febrile due to [[COVID-19]] infection, hypothermic, or have a normal temperature. The case study described the maximum temperature of patients to be 39°C. | ||
*The limited data does not report distended abdomen, tenderness, or hypo/hyperactive bowel sounds in patients who presented with abdominal pain associated with [[COVID]]. | |||
*Shallow breathing can be due to severe [[respiratory distress]] or severe [[abdominal pain]].<ref name="pmid32309266">{{cite journal |vauthors=Poggiali E, Ramos PM, Bastoni D, Vercelli A, Magnacavallo A |title=Abdominal Pain: A Real Challenge in Novel COVID-19 Infection |journal=Eur J Case Rep Intern Med |volume=7 |issue=4 |pages=001632 |date=2020 |pmid=32309266 |pmc=7162568 |doi=10.12890/2020_001632 |url=}}</ref> | |||
: | |||
=== Laboratory Findings === | === Laboratory Findings === | ||
*There are no specific laboratory findings associated with [ | *There are no specific laboratory findings associated with abdominal pain in [[COVID-19]] patients. Biochemical markers of liver injury may appear in lab tests.<ref name="pmid32309266">{{cite journal |vauthors=Poggiali E, Ramos PM, Bastoni D, Vercelli A, Magnacavallo A |title=Abdominal Pain: A Real Challenge in Novel COVID-19 Infection |journal=Eur J Case Rep Intern Med |volume=7 |issue=4 |pages=001632 |date=2020 |pmid=32309266 |pmc=7162568 |doi=10.12890/2020_001632 |url=}}</ref> | ||
*Serum potassium levels are normal in patients but an important test to exclude life-threatening conditions in patients presenting with abdominal pain. | |||
*[[Bilirubin]] can be high, C-reactive protein, [[liver function tests]], [[alanine aminotransferase|ALT]], [[aspartate aminotransferase|AST]] and [[gamma glutamyltransferase|Gamma GT]] can be high. | |||
*[[Complete blood count]] provides information about the infectious status of the patient via increased [[white blood cells|WBCs]], or [[lymphocytes]] indicating viral infection. | |||
*Value of [[CRP]] and [[procalcitonin]] also help in excluding inflammation and bacterial source of infection.<ref name="pmid32309266">{{cite journal |vauthors=Poggiali E, Ramos PM, Bastoni D, Vercelli A, Magnacavallo A |title=Abdominal Pain: A Real Challenge in Novel COVID-19 Infection |journal=Eur J Case Rep Intern Med |volume=7 |issue=4 |pages=001632 |date=2020 |pmid=32309266 |pmc=7162568 |doi=10.12890/2020_001632 |url=}}</ref> | |||
===Imaging Findings=== | ===Imaging Findings=== | ||
* | *[[Ultrasound]] of the abdomen may or may not show any abnormal findings. Bowel [[inflammatory]] signs (peri-intestinal inflammatory reaction) | ||
*[[CT scan]] abdomen: CT scan maybe normal or confirm the peri-intestinal inflammatory reaction.<ref name="pmid32309266">{{cite journal |vauthors=Poggiali E, Ramos PM, Bastoni D, Vercelli A, Magnacavallo A |title=Abdominal Pain: A Real Challenge in Novel COVID-19 Infection |journal=Eur J Case Rep Intern Med |volume=7 |issue=4 |pages=001632 |date=2020 |pmid=32309266 |pmc=7162568 |doi=10.12890/2020_001632 |url=}}</ref> | |||
* | |||
=== Other Diagnostic Studies === | === Other Diagnostic Studies === | ||
*[ | *A study by Poggiali et al. strongly recommends bedside lung [[ultrasound]] to detect the signs of respiratory [[CPVID-19]] infection even when there are no respiratory symptoms.<ref name="pmid32309266">{{cite journal |vauthors=Poggiali E, Ramos PM, Bastoni D, Vercelli A, Magnacavallo A |title=Abdominal Pain: A Real Challenge in Novel COVID-19 Infection |journal=Eur J Case Rep Intern Med |volume=7 |issue=4 |pages=001632 |date=2020 |pmid=32309266 |pmc=7162568 |doi=10.12890/2020_001632 |url=}}</ref> | ||
== Treatment == | == Treatment == | ||
=== Medical Therapy === | === Medical Therapy === | ||
*The mainstay of therapy for [[COVID-19]] associated abdominal pain is supportive care and antiviral therapy, including lopinavir and [[ritonavir]] tablets. Treating the infection treats the direct cause of gut damage. | |||
*Response to medical therapy can be monitored with the patient's general condition, symptoms, [[vital signs]], and [[ultrasound|US]] of the abdomen or[[CT scan]] abdomen if required. | |||
*The mainstay of therapy for [ | |||
*Response to | |||
=== Surgery === | === Surgery === | ||
* | *An acute abdomen may require surgery but [[COVID-19]] infected gut issues are health primarily with treating the infection itself. | ||
=== Prevention === | === Prevention === | ||
* | *The only prevention for [[COVID-19]] associated abdominal pain is the prevention and early diagnosis of the [[coronavirus-19]] infection itself. According to the CDC, the measures include:<ref name="urlHow to Protect Yourself & Others | CDC">{{cite web |url=https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html |title=How to Protect Yourself & Others | CDC |format= |work= |accessdate=}}</ref> | ||
**Frequent handwashing with soap and water for at least 20 seconds or using a [[alcohol rub|alcohol based hand sanitizer]] with at least 60% alcohol. | |||
**Staying at least 6 feet (about 2 arms’ length) from other people who do not live with you. | |||
**Covering your mouth and nose with a cloth face cover when around others and covering sneezes and coughs. | |||
**Cleaning and [[disinfect]]ing. | |||
==References== | ==References== | ||
Revision as of 00:14, 28 June 2020
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Javaria Anwer M.D.[2]
Synonyms and keywords: COVID-19 associated abdominal pain, COVID associated abdominal pain, COVID likned abdominal pain, COVID-19 linked abdominal pain, coronavirus associated abdominal pain, coronavirus related belly pain, abdominal pain associated with COVID-19, abdominal pain associated with SARS CoV2, SARS CoV2 related abdominal pain, SARS CoV2 linked abdomin pain, abdominal pain and COVID-19, abdominal pain and SARS CoV2 ,abdominal pain in COVID, abdomin pain in COVID, abdominal pain in nCoV, abdominal discomfort in COVID-19, abdominal discomfort in SARS CoV2
Overview
Abdominal pain is a vast entity and sometimes a challenge due to its various potential diagnoses. Although COVID-19 is mainly a respiratory disease, abdominal pain is one of the symptoms of COVID-19 infection.
Historical Perspective
- A cluster of cases of pneumonia in Wuhan, China was first reported on December 31st, 2019 by Wuhan Municipal Health Commission, China. A novel coronavirus was eventually identified. The first disease outbreak news on the new virus was first published by WHO on 5th January 2020.[1]
- On March 12, 2020, WHO declared the COVID-19 outbreak a pandemic.
- Initially COVID-19 was primarily known as a respiratory disease. In the initial phase of the pandemic, the screening criteria for COVID‐19 did not include symptoms of abdominal pain.
- On Feb 3rd, 2020, a study published by Wang D et al. first described abdominal pain as one of the less common symptoms of COVID-19.[2]
- With the increasing evidence and ongoing research, abdominal pain is now reported to be a common symptom in patients with COVID-19, and the viral infection is suspected in a patient presenting with abdominal pain. Research is underway to develop a better understanding of the etiology, risk factors, and treatment of abdominal pain associated with COVID-19.
Pathophysiology
- ACE 2 acts as the SARS-CoV2 receptor for infectivity and the entrance into the cell. Research has shown ACE 2 receptors in esophageal epithelial cells, ileal and colon enterocytes making them vulnerable to COVID-19 infection. The detection of viral nucleocapsid protein in gastrointestinal epithelial cells and viral RNA in fecal specimens reflects the infectivity and chance of direct viral damage of organs.[3][4][5] The entry of the virus causes disruption of the enterocytes and may lead to inflammation, impaired cell permeability, and cellular damage.
- The abdominal pain can be due to direct viral infection of the gastrointestinal tract via cellular ACE 2 receptors in several abdominal organs, making them susceptible to viral infection.
Clinical Features
Differentiating abdominal pain due to COVID-19 from other Diseases
- If the patient complains of diarrhea and abdominal pain stool test for bacterial, viral, and treatment-related causes of diarrhea. Clostridium difficile and other enteric pathogens can help differentiate alternate causes.
Epidemiology and Demographics
- Based upon the meta-analysis including 78 studies the Weighted Pooled Prevalence (WPP) of abdominal pain associated with COVID-19 is approximately 6.2% (2.6%-10.3%). Although the data comes from four studies, the WPP of abdominal pain at illness onset was 4.1% and at admission was 7.3%.[6]
- Age: Very limited data is available about the detailed demographics of the patients having abdominal pain as one of the symptoms of COVID-19 infection. A study reporting 10 cases presenting with abdominal pain as one of the symptoms showed the mean age of 50±18 years.
- Race: Data from 12797 patients showed a higher weighted pooled prevalence of abdominal pain associated with COVID-19 in the non-Chinese subgroup.
Risk Factors
- The main risk factor for the development of the disease is COVID-19 infection.
- The incidence of abdominal pain and diarrhea was higher in patients with severe COVID-19
Natural History, Complications and Prognosis
- The majority of patients with abdominal pain
- If left untreated,
- Common complications
- Prognosis is generally good.
Diagnosis
Diagnostic Criteria
- There are no established diagnostic criteria to identify the cause of abdominal pain in SARS-CoV2 patient. Abdominal ultrasound or CT scan, and blood tests showing deranged liver functions can give a clue of possible gastrointestinal involvement.
History and Symptoms
- The patient may have abdominal pain as an accompanying symptom along with other SARS-CoV2 infection symptoms such as anorexia, fever, cough, and malaise. Very few patients present with abdominal pain as the sole symptom and high suspicion is required in order to reach the diagnosis.
Physical Examination
- Patients with abdominal pain associated with COVID-19 can be in distress due to their general condition or the severity of abdominal pain. A person with pancreatitis will appear dehydrated, lethargic and in severe pain.
- PThe patient can be febrile due to COVID-19 infection, hypothermic, or have a normal temperature. The case study described the maximum temperature of patients to be 39°C.
- The limited data does not report distended abdomen, tenderness, or hypo/hyperactive bowel sounds in patients who presented with abdominal pain associated with COVID.
- Shallow breathing can be due to severe respiratory distress or severe abdominal pain.[7]
Laboratory Findings
- There are no specific laboratory findings associated with abdominal pain in COVID-19 patients. Biochemical markers of liver injury may appear in lab tests.[7]
- Serum potassium levels are normal in patients but an important test to exclude life-threatening conditions in patients presenting with abdominal pain.
- Bilirubin can be high, C-reactive protein, liver function tests, ALT, AST and Gamma GT can be high.
- Complete blood count provides information about the infectious status of the patient via increased WBCs, or lymphocytes indicating viral infection.
- Value of CRP and procalcitonin also help in excluding inflammation and bacterial source of infection.[7]
Imaging Findings
- Ultrasound of the abdomen may or may not show any abnormal findings. Bowel inflammatory signs (peri-intestinal inflammatory reaction)
- CT scan abdomen: CT scan maybe normal or confirm the peri-intestinal inflammatory reaction.[7]
Other Diagnostic Studies
- A study by Poggiali et al. strongly recommends bedside lung ultrasound to detect the signs of respiratory CPVID-19 infection even when there are no respiratory symptoms.[7]
Treatment
Medical Therapy
- The mainstay of therapy for COVID-19 associated abdominal pain is supportive care and antiviral therapy, including lopinavir and ritonavir tablets. Treating the infection treats the direct cause of gut damage.
- Response to medical therapy can be monitored with the patient's general condition, symptoms, vital signs, and US of the abdomen orCT scan abdomen if required.
Surgery
- An acute abdomen may require surgery but COVID-19 infected gut issues are health primarily with treating the infection itself.
Prevention
- The only prevention for COVID-19 associated abdominal pain is the prevention and early diagnosis of the coronavirus-19 infection itself. According to the CDC, the measures include:[8]
- Frequent handwashing with soap and water for at least 20 seconds or using a alcohol based hand sanitizer with at least 60% alcohol.
- Staying at least 6 feet (about 2 arms’ length) from other people who do not live with you.
- Covering your mouth and nose with a cloth face cover when around others and covering sneezes and coughs.
- Cleaning and disinfecting.
References
- ↑ "WHO Timeline - COVID-19".
- ↑ Wang, Dawei; Hu, Bo; Hu, Chang; Zhu, Fangfang; Liu, Xing; Zhang, Jing; Wang, Binbin; Xiang, Hui; Cheng, Zhenshun; Xiong, Yong; Zhao, Yan; Li, Yirong; Wang, Xinghuan; Peng, Zhiyong (2020). "Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China". JAMA. 323 (11): 1061. doi:10.1001/jama.2020.1585. ISSN 0098-7484.
- ↑ Zou, Xin; Chen, Ke; Zou, Jiawei; Han, Peiyi; Hao, Jie; Han, Zeguang (2020). "Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection". Frontiers of Medicine. 14 (2): 185–192. doi:10.1007/s11684-020-0754-0. ISSN 2095-0217.
- ↑ Tian Y, Rong L, Nian W, He Y (May 2020). "Review article: gastrointestinal features in COVID-19 and the possibility of faecal transmission". Aliment. Pharmacol. Ther. 51 (9): 843–851. doi:10.1111/apt.15731. PMC 7161803 Check
|pmc=value (help). PMID 32222988 Check|pmid=value (help). - ↑ Gheblawi M, Wang K, Viveiros A, Nguyen Q, Zhong JC, Turner AJ, Raizada MK, Grant MB, Oudit GY (May 2020). "Angiotensin-Converting Enzyme 2: SARS-CoV-2 Receptor and Regulator of the Renin-Angiotensin System: Celebrating the 20th Anniversary of the Discovery of ACE2". Circ. Res. 126 (10): 1456–1474. doi:10.1161/CIRCRESAHA.120.317015. PMC 7188049 Check
|pmc=value (help). PMID 32264791 Check|pmid=value (help). - ↑ Tariq, Raseen; Saha, Srishti; Furqan, Fateeha; Hassett, Leslie; Pardi, Darrell; Khanna, Sahil (2020). "Prevalence and Mortality of COVID-19 patients with Gastrointestinal Symptoms: A Systematic Review and Meta-analysis". Mayo Clinic Proceedings. doi:10.1016/j.mayocp.2020.06.003. ISSN 0025-6196.
- ↑ 7.0 7.1 7.2 7.3 7.4 Poggiali E, Ramos PM, Bastoni D, Vercelli A, Magnacavallo A (2020). "Abdominal Pain: A Real Challenge in Novel COVID-19 Infection". Eur J Case Rep Intern Med. 7 (4): 001632. doi:10.12890/2020_001632. PMC 7162568 Check
|pmc=value (help). PMID 32309266 Check|pmid=value (help). - ↑ "How to Protect Yourself & Others | CDC".