Bell's palsy: Difference between revisions
No edit summary |
No edit summary |
||
| Line 18: | Line 18: | ||
'''For patient information click [[{{PAGENAME}} (patient information)|here]]''' | '''For patient information click [[{{PAGENAME}} (patient information)|here]]''' | ||
'''Editor-in-Chief:''' Gilbert Dagher, M.D. | |||
{{Editor | {{Editor Join}} | ||
==Overview== | ==Overview== | ||
Revision as of 19:32, 1 June 2010
| Bell's palsy | |
 | |
|---|---|
| ICD-10 | G51.0 |
| ICD-9 | 351.0 |
| DiseasesDB | 1303 |
| MedlinePlus | 000773 |
| eMedicine | emerg/56 |
| MeSH | D020330 |
|
WikiDoc Resources for Bell's palsy |
|
Articles |
|---|
|
Most recent articles on Bell's palsy Most cited articles on Bell's palsy |
|
Media |
|
Powerpoint slides on Bell's palsy |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Bell's palsy at Clinical Trials.gov Clinical Trials on Bell's palsy at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Bell's palsy
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Bell's palsy Discussion groups on Bell's palsy Patient Handouts on Bell's palsy Directions to Hospitals Treating Bell's palsy Risk calculators and risk factors for Bell's palsy
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Bell's palsy |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
For patient information click here
Editor-in-Chief: Gilbert Dagher, M.D.
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [1] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
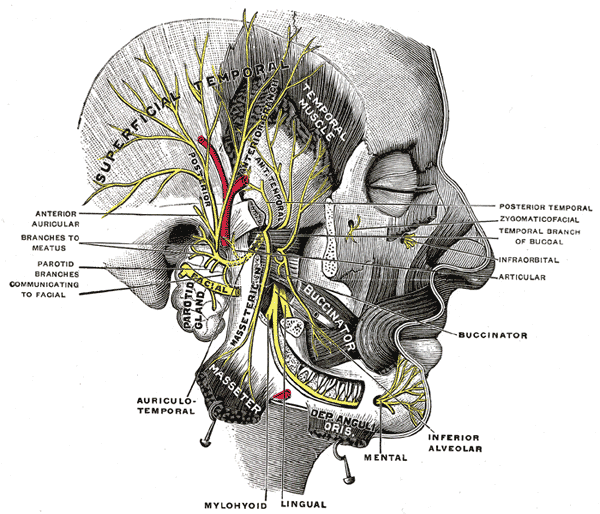
Bell's palsy (or facial palsy) is characterised by facial drooping on the affected half, due to malfunction of the facial nerve (VII cranial nerve), which controls the muscles of the face. Named after Scottish anatomist Charles Bell, who first described it, Bell's palsy is the most common acute mononeuropathy (disease involving only one nerve), and is the most common cause of acute facial nerve paralysis. The paralysis is of the infranuclear/lower motor neuron type. Bell’s palsy affects about 40,000 people in the United States every year. It affects approximately 1 person in 65 during a lifetime. Until recently, its cause was unknown in most cases, but it has now been related to both Lyme disease and Herpes Zoster.
Epidemiology
Bell's Palsy is three times more likely to strike pregnant women than non-pregnant women.[1] It is also considered to be four times more likely to occur in diabetics than the general population,[2] and it is more common in young adults
Pathophysiology & Etiology
Many cases likely due to Herpes Simplex Virus (HSV) reactivation
Other infectious causes
- Varicella-zoster virus (VZV), Ramsay-Hunt syndrome
- Lyme disease
- HIV (seroconversion)
- Adenovirus, coxsackievirus
- Mumps
- Influenza B
- Syphilis
Non-infectious causes
- Tumor
- Pontine infarct
- Temporal bone fracture
- Systemic Lupus Erythematosus (SLE)
- Sarcoidosis
Risk Factors
Pregnancy: 3rd trimester through 1st week post-partum (Relative Risk = 3)
Diabetes: present in 5-10% of patients
Prior episode: ipsilateral or contralateral recurrence rate 8-10%
Pathology
It is supposed to be the result of inflammation of the facial nerve, which produces pressure on the nerve as it exits the skull within its bony canal. Patients with facial palsy for which an underlying cause can be readily found are not generally considered to have Bell's palsy per se. These underlying problems include tumor, meningitis, stroke, diabetes mellitus, head trauma and inflammatory diseases of the cranial nerves (sarcoidosis, brucellosis, etc.) In these conditions, the neurologic findings are rarely restricted to the facial nerve. Babies can be born with facial palsy, and they exhibit many of the same symptoms as people with Bell's palsy; this is often due to a traumatic birth which causes irreparable damage to the facial nerve, i.e. acute facial nerve paralysis.

One disease that may be difficult to exclude in the differential diagnosis is involvement of the facial nerve in infections with the herpes zoster virus. The major differences in this condition are the presence of small blisters, or vesicles, of the external ear and hearing disturbances, but these findings may occasionally be lacking.
In recent years, two new suspects have been added to the possible causes of Bell's palsy. Lyme disease may produce the typical palsy, and may be easily diagnosed by looking for Lyme-specific antibodies in the blood. In endemic areas Lyme disease may be the most common cause of facial palsy. The subsequent observation of an increased incidence of antibodies to the Herpes simplex virus in patients with Bell's palsy has led many specialists to believe that this agent is the most likely underlying cause in areas where Lyme disease is uncommon.
In traditional Chinese medicine, considered an alternative medicine in the West, Bell's palsy is attributed to a "wind cold" attack brought about by exposure to wind.[3]
History and Symptoms
Onset over hours (maximal symptoms by 48 hours)
- Eyebrow sag with inability to close eye
- Nasolabial fold flattening with mouth drawn to affected side
- Inability to wrinkle forehead (peripheral lesion)
- May be associated with or preceded by ear pain (~20%)
- May be associated with:
- Impaired taste 23%
- Increased lacrimation 24%
- Hyperacusis 7%
Diagnosis
Bell's palsy is a diagnosis of exclusion; in many cases, no specific cause can be ascertained.
Testing for Lyme not indicated unless other suggestive symptoms or risk factors.
Other Imaging Findings
Imaging only if atypical symptoms or slow progression (risk of tumor). Electromyography (EMG) may help with prognosis in patients with complete cranial nerve (CN) VII paralysis
Investigation
Clinicians should determine whether all branches of the facial nerve are involved, or whether the forehead muscles are spared. Since these receive innervation from both sides of the brain, the forehead can still be wrinkled by a patient whose facial palsy is caused by a problem in the brain rather than in the facial nerve itself.
Facial palsy results from inability to control movement in the facial muscles. The facial muscles become weak or paralyzed. There is no specific treatment for Bell's palsy, and it typically subsides on its own within 2-3 weeks.
Risk Stratification and Prognosis
Excellent or complete recovery in 80% within weeks-months. Recovery depends on initial severity
- Incomplete lesions: 94% recover to normal function
- Complete lesions: 60% recover to normal function
Treatment
Eye care: nocturnal patch, lacrilube, artificial tears if poor lid closure
Pharmacotherapy
Glucocorticoids: +/- higher rate of recovery if reaction at onset
Antivirals: ACV 400 mg 5xd + prednisone better than prednisone alone
Valacyclovir: 1 g tid x 7d = easier alternative to ACV
Treatment is a matter of controversy. In patients presenting with incomplete facial palsy, treatment may be unnecessary. However, patients presenting with complete paralysis, marked by an inability to close the eyes and mouth on the involved side, are usually treated with anti-inflammatory corticosteroids. Prednisolone, a corticosteroid, if used early in treatment of Bell's palsy, significantly improves the chances of complete recovery at 3 and 9 months when compared to treatment with acyclovir, an anti-viral drug, or no treatment at all. The likely association of Bell's palsy with the herpes virus has led most American neurologists to prescribe a course of anti-viral medication (such as acyclovir) to all patients with unexplained facial palsy.
People who think they may have Bell's Palsy should consult their doctor as soon as possible. Many times, the medications will not be effective if administered too late after the onset.
Although most patients (60–80%) recover completely from Bell's palsy within several weeks, some require several months, and others may be left with deficits of varying degrees.
Complications
Major complications of the condition are chronic loss of taste (ageusia), chronic facial spasm and corneal infections. To prevent the latter, the eyes may be protected by covers, or taped shut during sleep and for rest periods, and tear-like eye drops or eye ointments may be recommended, especially for cases with complete paralysis. Where the eye does not close completely, the reflex is also affected; great care should be taken to protect the eye from injury.
Another complication can occur in case of incomplete or erroneous regeneration of the damaged facial nerve. The nerve can be thought of as a bundle of smaller individual nerve connections which branch out to their proper destinations. During regrowth, nerves are generally able to track the original path to the right destination - but some nerves may sidetrack leading to a condition known as synkinesis. For instance, regrowth of nerves controlling muscles attached to the eye may sidetrack and also regrow connections reaching the muscles of the mouth. In this way, movement of one also affects the other. For example, when the person closes the eye, the corner of the mouth will lift, or when smiling, the eye will close (synkinesis).
In addition, around 6% of patients exhibit crocodile tear syndrome on recovery, where they will shed tears while eating. This is thought to be due to faulty regeneration of the facial nerve, a branch of which controls the lacrimal and salivary glands.
References
- ↑ Bender, Paula Gillingham. "Facing Bell's Palsy while pregnant." (Commercial website). Sheknows: Pregnancy and Baby. Retrieved on 2007-09-06.
- ↑ "Bell's Palsy InfoSite & Forums: Facial Paralysis FAQs" (Website). Bell's Palsy Information Site. Retrieved on 2007-09-06.
- ↑ Pao, Fay-Meling von Moltke. (July 2005). "Bell's Palsy" (Online newsletter). Points, July 2005, Vol. 3, No. 7, via accupuncture.com. Retrieved on 2007-09-06.
Additional Resources
- Sullivan FM, Swan IRC, Donnan PT, et al. Early treatment with prednisolone or acyclovir in Bell's palsy. N Engl J Med 2007;357:1598-1607.
- "The Merck Manual"
- New England Journal of Medicine, Sept. 2004
- Lambert, Michael. (2007-03-05) "Bell's Palsy." (Website.) Emedicine. Retrieved on 2007-09-27.
External links
- managment and treatment of facial paralysis
- Bell's Palsy Information Site, has a FAQ
- Bell's Palsy and Pregnancy
- Bell's Palsy Patient Info - Neurology Channel
- Living with Facial Palsy, a site for parents of children with Facial Palsy
- Links to pictures of Bells palsy (Hardin MD/Univ of Iowa)
- Bell's Palsy Association
Template:SIB Template:PNS diseases of the nervous system
ar:شلل العصب الوجهي ca:Paràlisi de Bell de:Fazialislähmung nl:Aangezichtsverlamming van Bell fi:Bellin halvaus Template:WH Template:WikiDoc Sources